Epidemiology
Average age 6 years (4 - 10)
20% distal humeral fracture
- second most common elbow fracture
- after supracondylar
Mechanism

Pull off
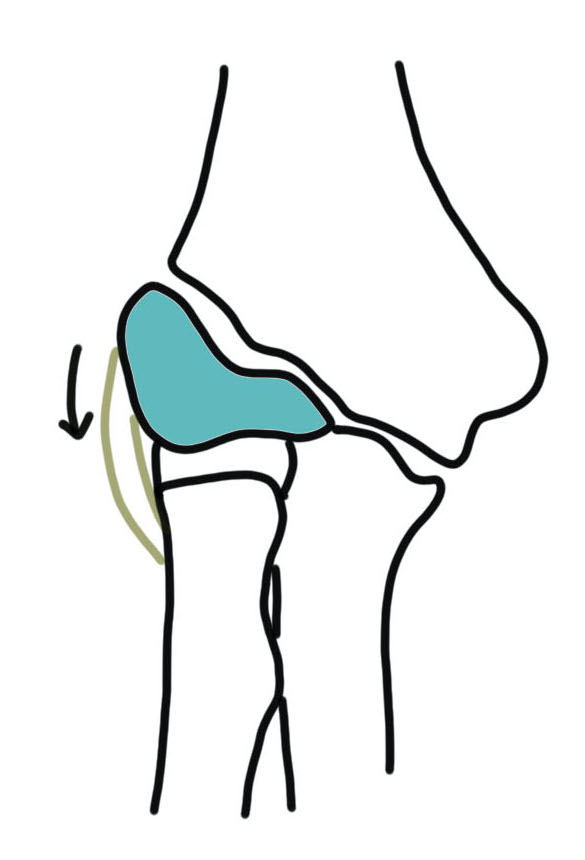
Pull Off
- more common
- fall on outstretched arm
- lateral condyle is pulled off by the common extensor origin
- varus stress

Push off
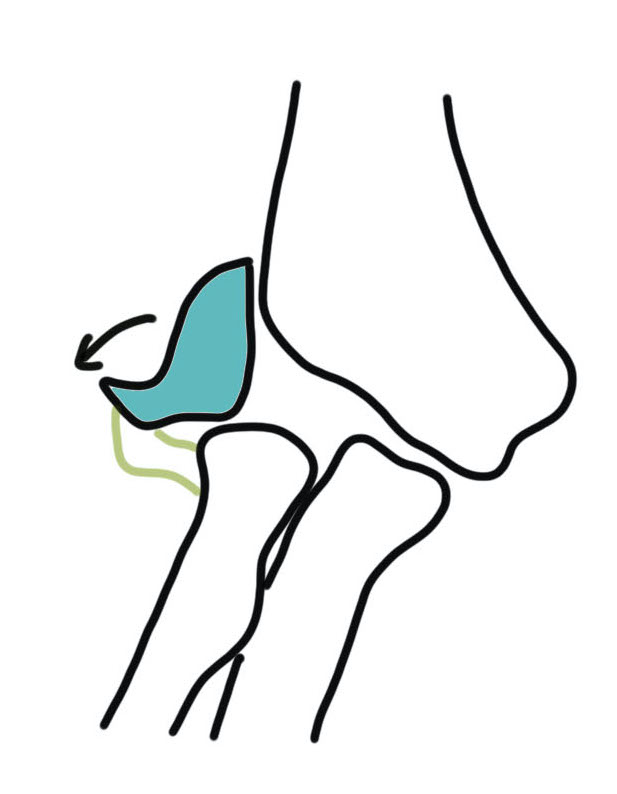
Push off
- radial head pushes off the lateral condyle
- valgus stress
Classification
Anatomical
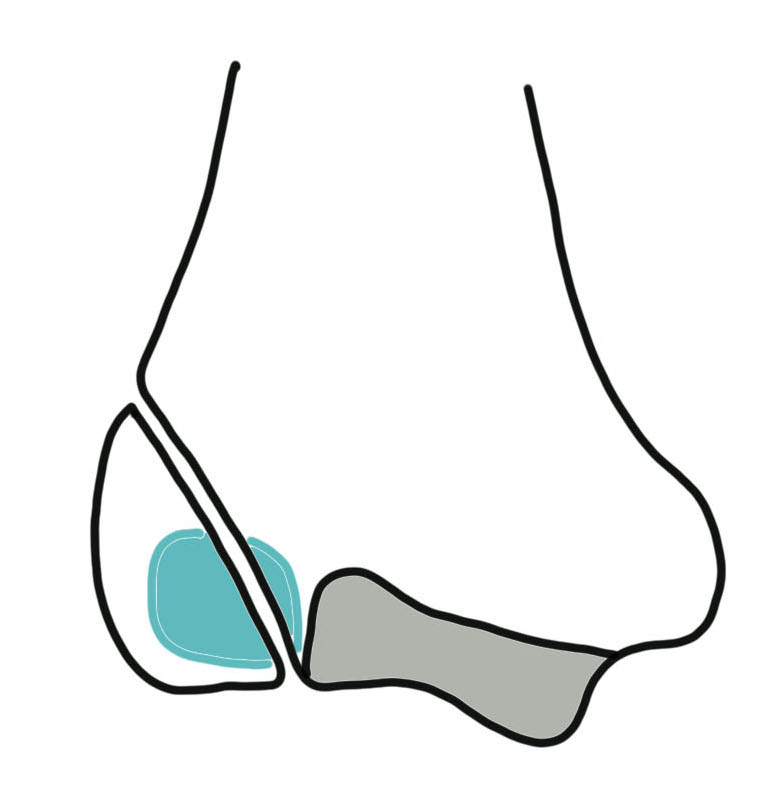
Milch I
Milch I
- SH IV
- fracture line lateral to trochlear groove
- elbow stable
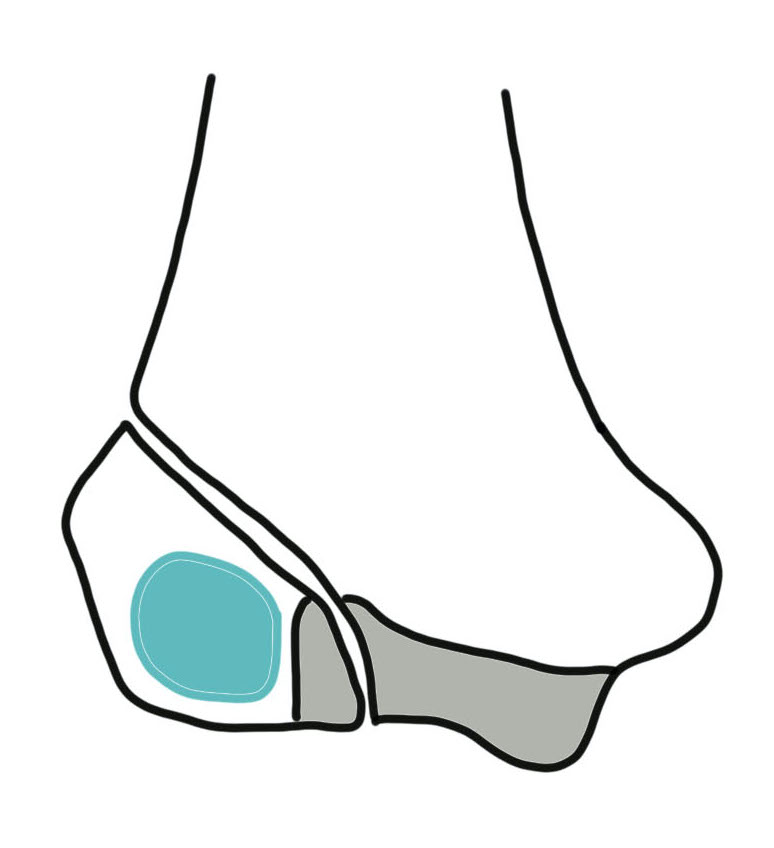

Milch II
Milch II
- SH II
- fracture line goes more medially into trochlear notch
- lateral wall of trochlear part of fracture fragment
- more common
- elbow can be unstable


Lateral condyle fracture with elbow dislocation
Displacement ~ Weiss Classification
Type I: < 2 mm displaced with articular surface intact
Type II: 2 - 4 mm displaced with articular surface intact
Type III: < 4 mm displaced, articular surface disrupted
Clinical
Age 6
History fall
Lateral pain
Swelling
X-ray
Undisplaced
- typically metaphyseal flake
- looks minimally displaced on AP and lateral
- perform an internal oblique x-ray to exclude displacement


Displaced


CT
MRI
Not typically used due to need for sedation
Management
Non operative
Indication

Undisplaced
Displaced < 2 mm
Technique
Confirm fracture is truly undisplaced
- internal oblique xray
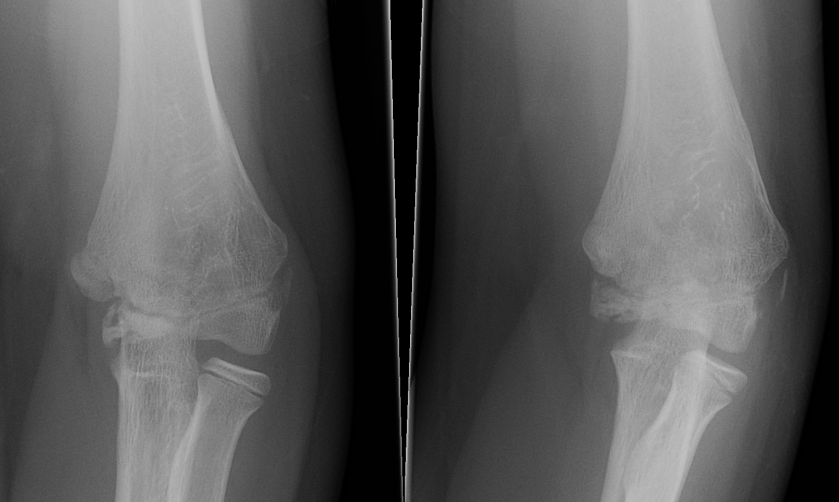
- xray other arm
Serial xrays for first 3 weeks
Remove case 4 - 6 weeks


Injured left elbow v injury right elbow
Results
Knapik et al J Paediatr Orthop 2017
- systematic review of 6 studies
- nonoperative management of lateral condyle fractures < 2 mm displaced
- risk of subsequent displacement 15%, usually within first week
- associated with non union and malunion
Internal oblique xray
Edmonds et al J Paediatr Orthop 2021
- 140 cases lateral condyle fracture treated non operatively
- displacement < 1.2 mm on internal oblique had failure rate of 58%
- displacement > 1.2 mm on internal oblique had failure rate of 1%
Kurtulmus et al Eur J Orthop Surg Traumatol 2014
- 27 patients with < 2 mm displacement on AP view
- 16 found to have > 2 mm displacement on subsequent internal oblique view
Operative
Surgical indications
1. Unstable / Milch II
2. Displaced > 2 mm
Options
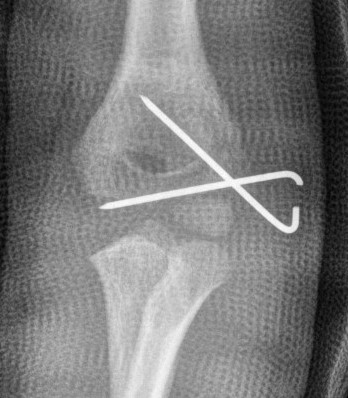
1. Closed reduction and percutaneous K wires
2. Open reduction and K wire or screw
Closed reduction and percutaneous K wires


Indications
- residual displacement < 2 mm
- no rotation
- confirm joint surface anatomically reduced (arthrogram)
Technique
- reduce by extension and varus
- pronation uses flexor mass to pull lateral condyle forward
- percutaneous K wire
Open reduction and K wires / screw fixation
AO surgery reference lateral approach distal humerus
Vumedi video open lateral condyle fracture
Lateral approach to distal humerus
- curved incision over lateral supracondylar ridge of humerus, and over proximal radius
- proximally intermuscular interval between brachioradialis & triceps
- proximally elevate brachioradialis and ECRL off the distal humerus
- distally split common extensor origin between ECRB and EDC and elevate anteriorly
Don't dissect posteriorly to protect blood supply
Don't need to dissect distal fragment
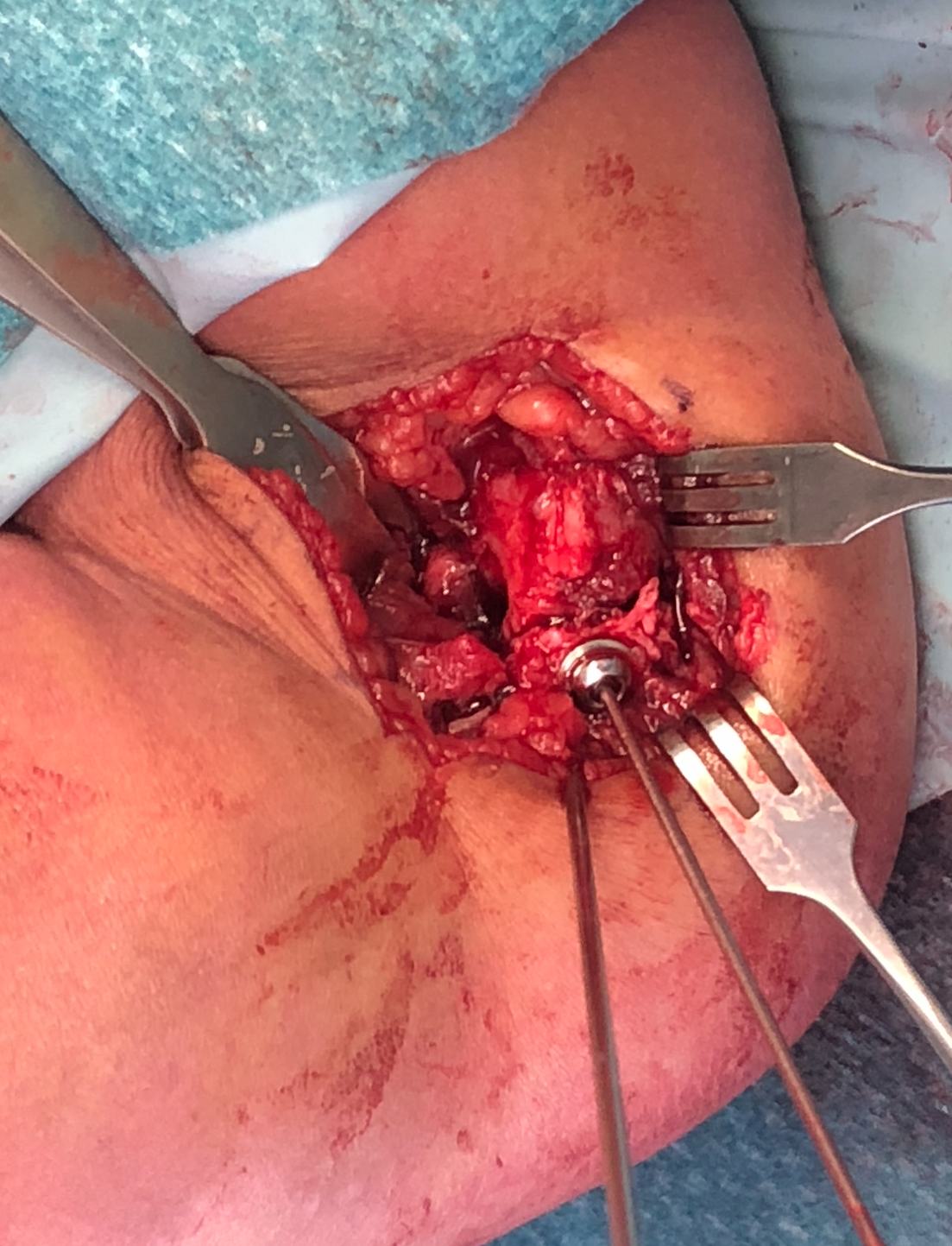
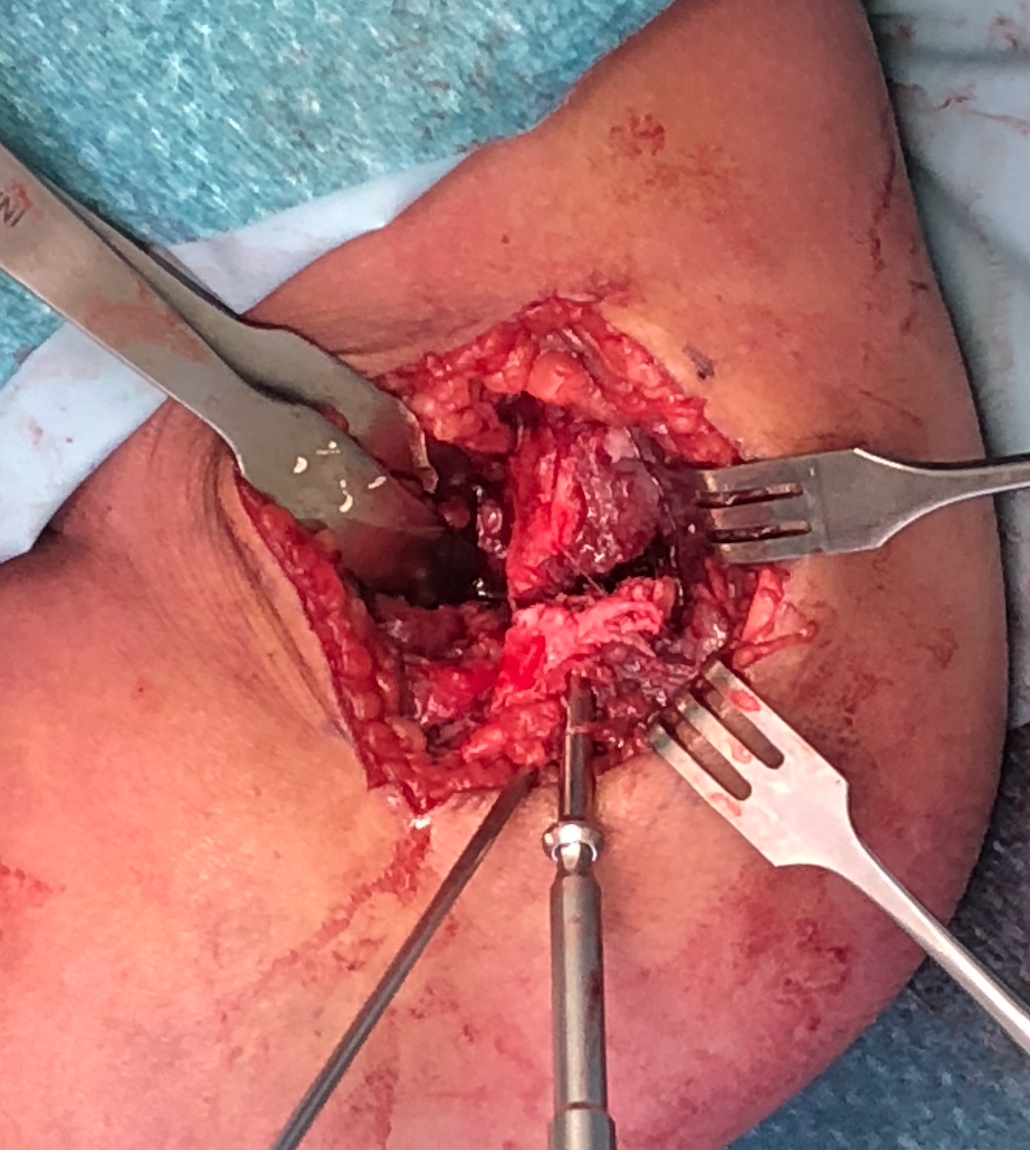
Use anterior homan retractor across distal humerus to elevate anterior capsule
- visualize distal joint line and perform anatomical reduction under vision
- one K wire parallel to joint surface across fracture into trochlea
- one K wire at 45 degrees to first engaging medial metaphysis
- bury K wires as need to be in for 6 weeks
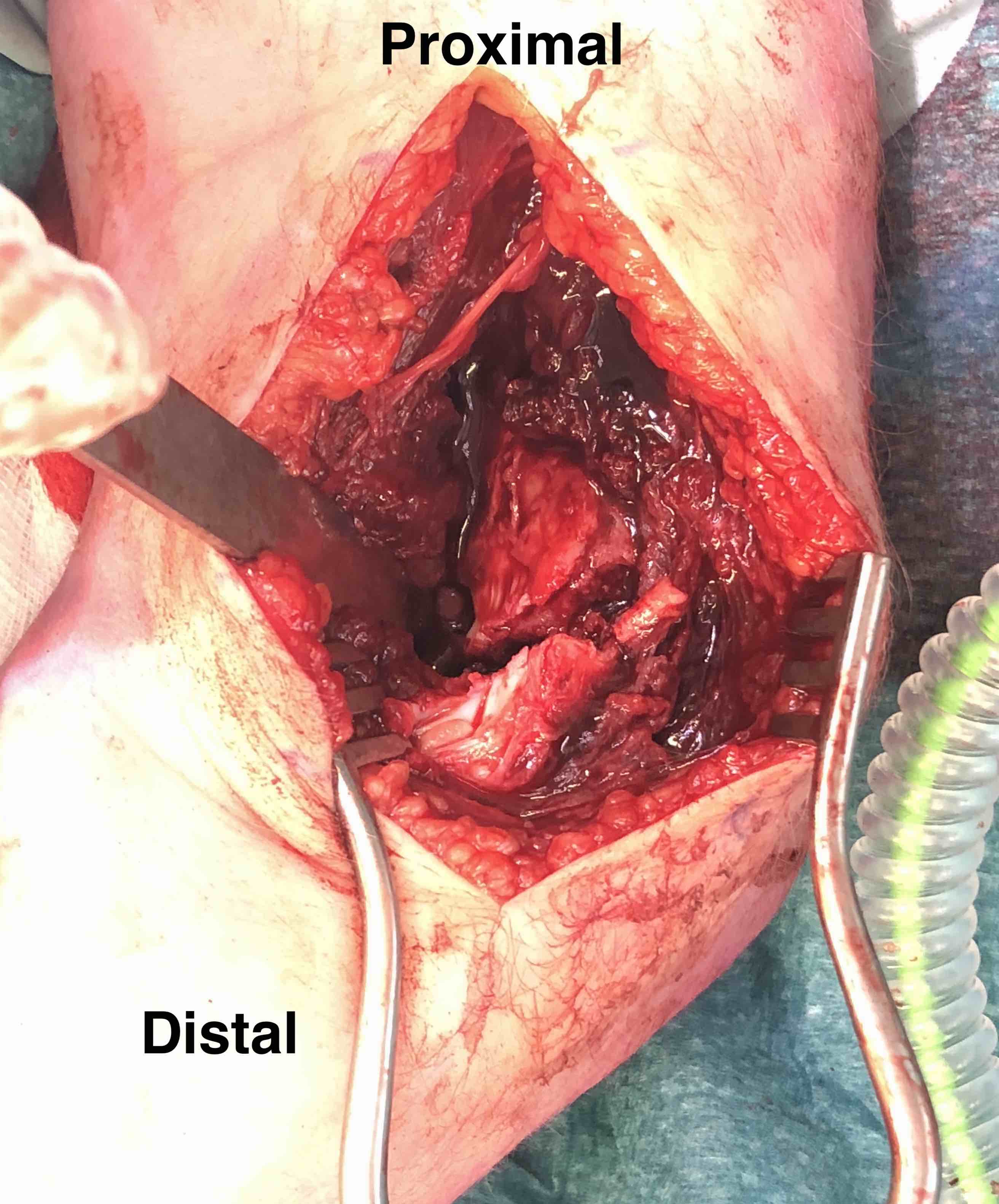
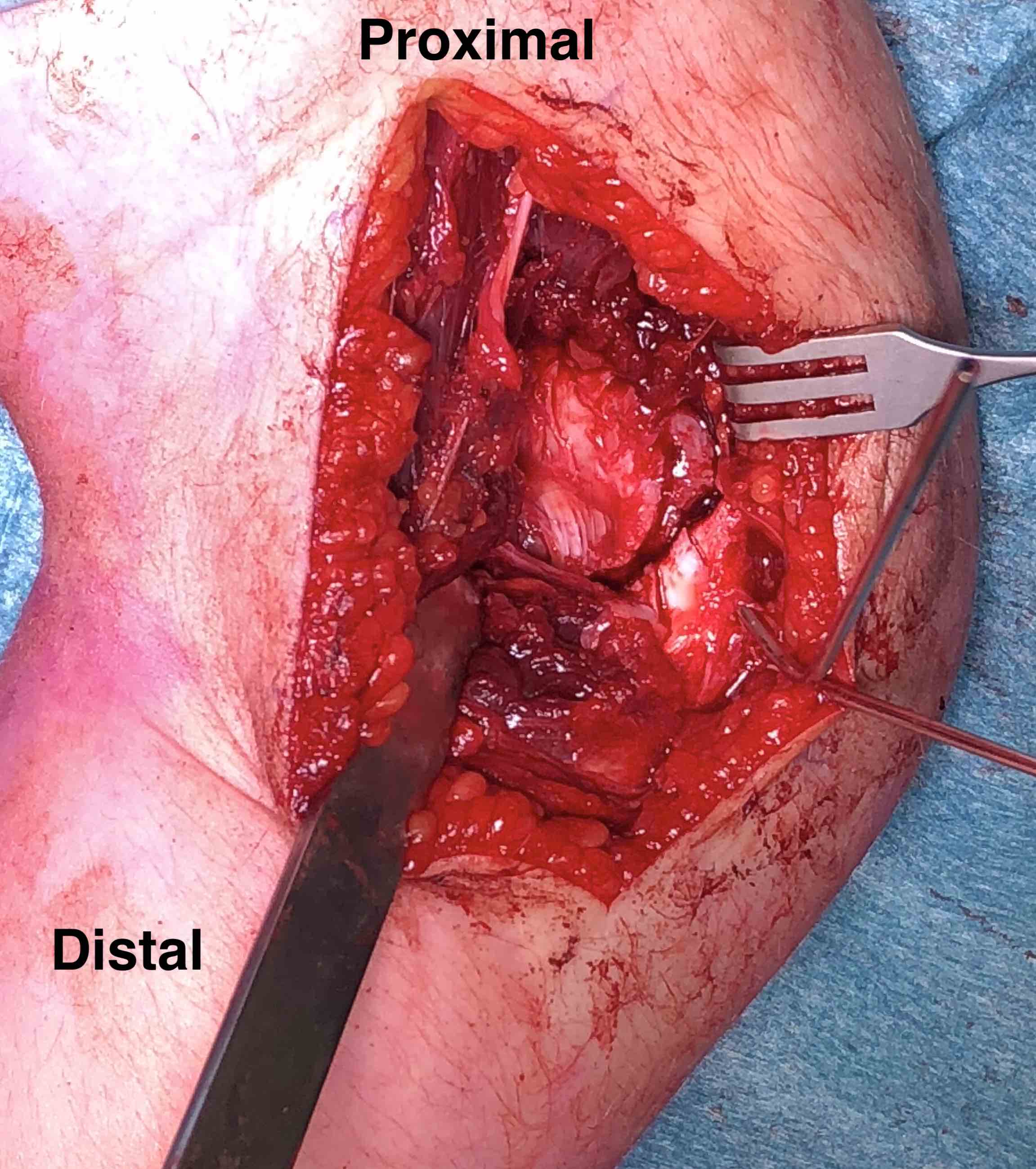
Open reduction of displaced lateral condyle in left elbow



Post op
- very real risk of non union
- elbow in POP for 6 weeks
- don't remove K wires until obvious union at 6 weeks
Results
Closed v open reduction
Pennock et al J Paediatr Orthop 2016
- lateral condyle fractures displaced 2 - 5 mm
- 51 open reduction and pinning, 23 closed reduction and pinning
- all healed by 12 weeks
- no major complications in closed reduction and percutaneous pinning
- open reduction had 1 AVN, 1 osteomyelitis, 1 refracture requiring repeat surgery
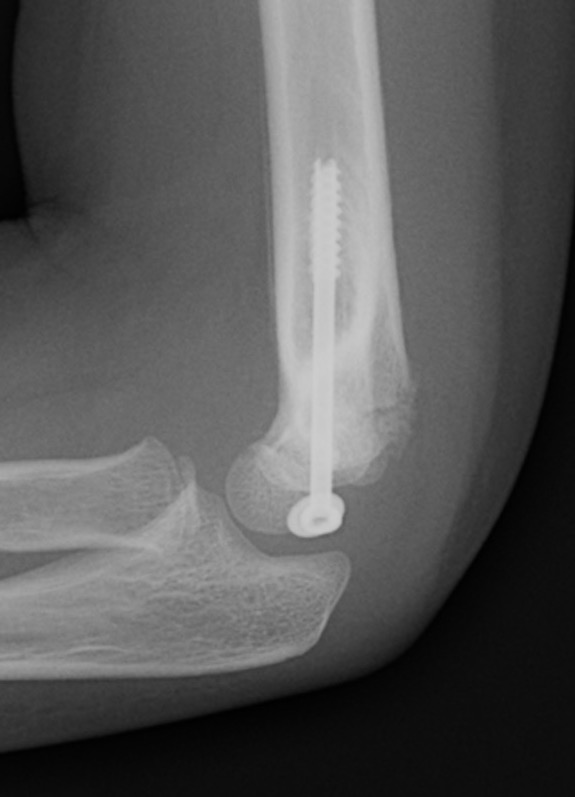
K wires v screws
Screw
- compression of fragment
- potentially less non union
- more difficult to remove
- 60 patients treated with lag screws or K wires
- no difference in outcome
- less stiffness in screw fixation due to earlier mobilisation

Delayed Presentation
Definition
Presentation after 3 weeks
Option 1. Reduction and ORIF
Risk of AVN and growth arrest due to excessive soft tissue stripping
- exact incidence / risk is unknown
- best option if fragment is displaced and mobile
- may do up to 6 weeks to 6 months
- controversial
Option 2. Bone graft and screw in situ
Will have valgus deformity
- delayed osteotomy
Complications
Issues
Higher rate of complications in comparison to supracondylar fractures
- intra-articular fracture
- transphyseal fracture
- inherently unstable
- tenuous blood supply (AVN)
- synovial fluid in fracture site (non union)
- often need open reduction and thus more scarring
Tan et al Arch Orthop Trauma Surg 2018
- systematic review of 2440 cases
- nonunion 1.6%
- flexion loss 10%, extension loss 11%
- valgus deformity 6% / varus deformity 8%
- prominent lateral condyle 27%
- fishtail deformity 14%
- growth plate closure 5%
- AVN 2%
- neurological deficit 11%
Non Union

Incidence
1.6%
- higher with increasing displacement
Definition
Delayed union - 6 weeks
Non union - 12 weeks
Causes
1. Non operative treatment / missed displaced fractures of the lateral condyle
2. Surgical malreduction
Salgueiro et al J Paediatr Orthop 2017
- 210 surgical cases
- delayed union and nonunion associated with > 1mm residual fracture gap after surgery
Presentation
Pain
Loss of ROM
Cubitus valgus
Tardy ulna nerve palsy
Management non displaced non union
Observe for union until 3 months
- then screw fixation +/- graft metaphyseal non-union
Management displaced non-union
A. Reduce and ORIF +/- bone graft
- though to be acceptable if < 6 months and fragment mobile
B. ORIF in situ +/- bone graft
- later osteotomy for malunion / valgus instability



In situ screw fixation delayed nonunion
Results
Park et al J Paediatr Orthop 2015
- in situ fixation of 16 cases of nonunion with screw
- average 5 months post surgery with average 6 mm displacement
- all united
- 3/16 residual deformity
Cubitus Varus / Overgrowth lateral condyle

Common problem
- little cosmetic or functional problem
Cubitus Valgus and Tardy Ulnar Nerve Palsy
Causes
- AVN
- nonunion
- malunion
- physeal arrest / malunion
Management
- anterior transposition nerve
- +/- osteotomy
Fishtail Deformity
AVN trochlea and fishtail deformity
Causes
- trochlear AVN
- central growth arrest
- often asymptomatic
