
Epidemiology
Rare - 2% of acute dislocations
Easily missed diagnosis
Etiology
Usually secondary major trauma
- MVA
- Seizures
- Electrocution
- Alcohol-related injuries
Examination
Loss of external rotation
- arm held across chest
- limited active and passive ROM
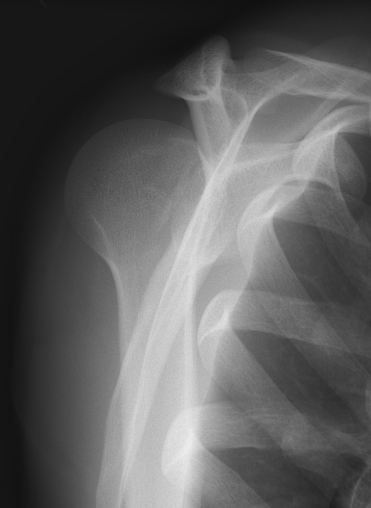
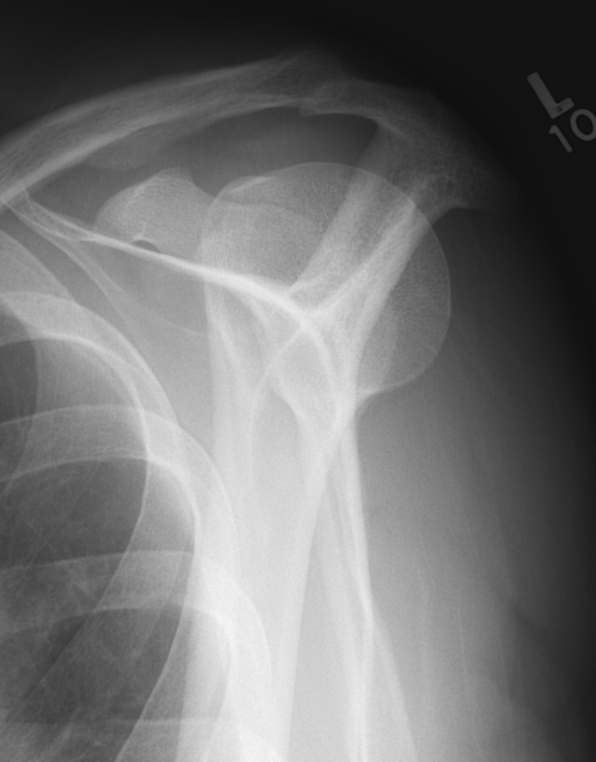
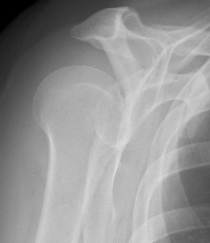
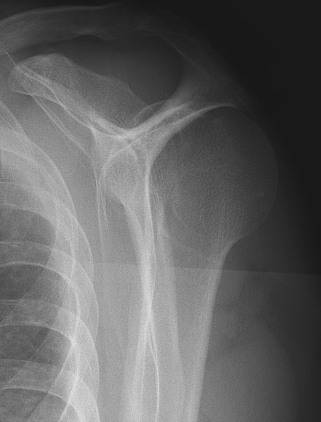
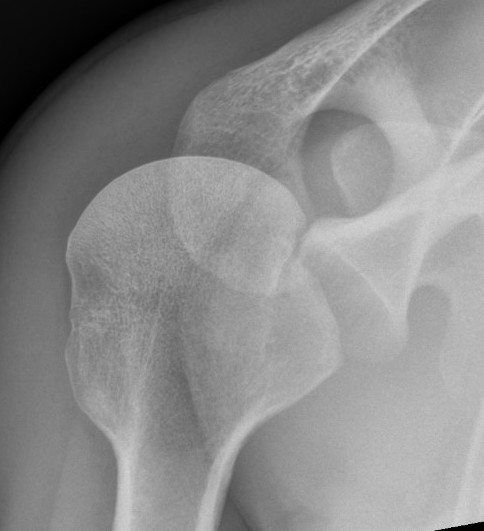
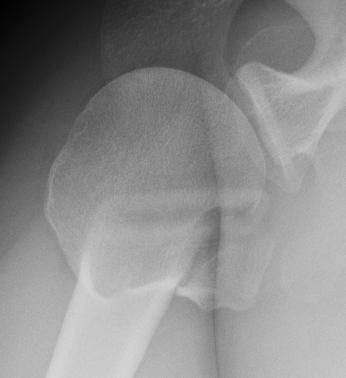
AP Xray



Abnormal overlap of humeral head on glenoid

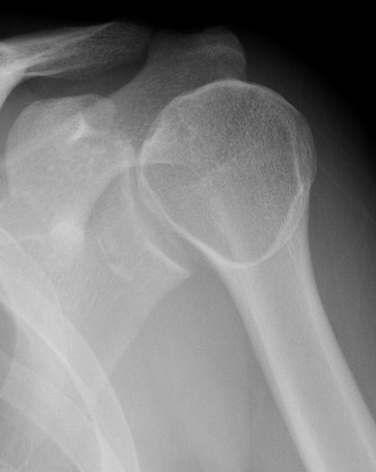

Light-bulb sign - globular head secondary to internal rotation of the humeral head


Vacant Glenoid Cavity - > 6 mm space between humeral head and anterior rim of glenoid
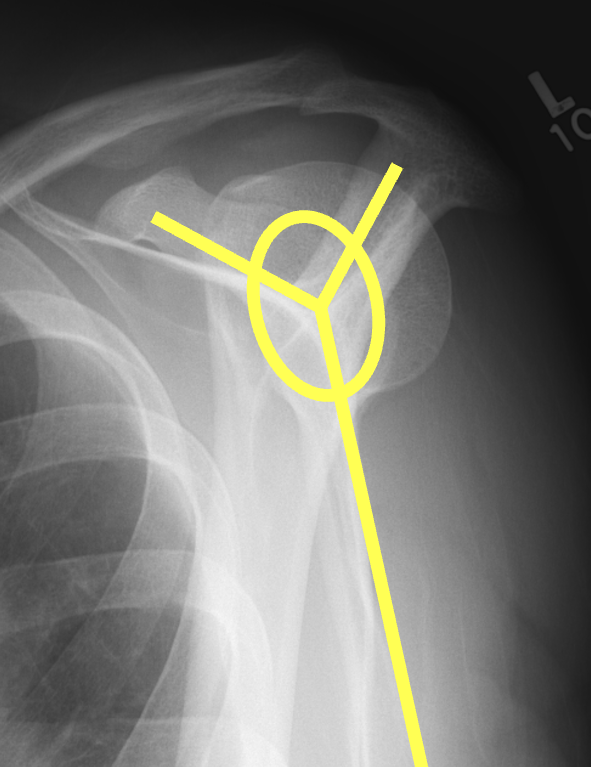
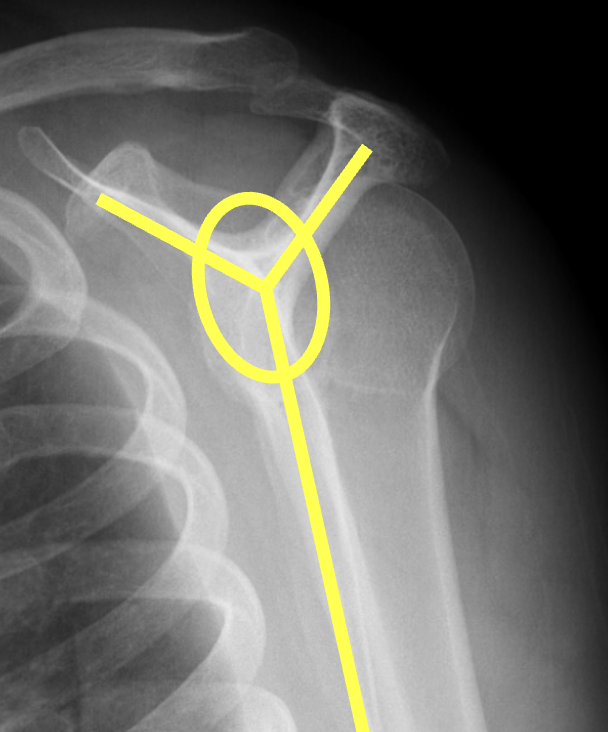
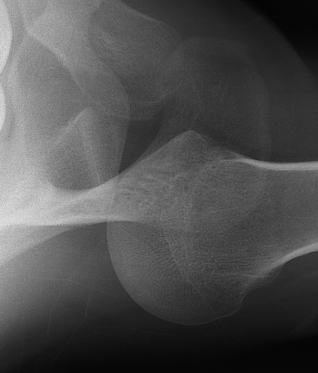
Scapular lateral
Center of the humeral head must be centered on the Y / Mercedes sign
Y is formed by
- coracoid anteriorly
- scapular spine posteriorly
- scapula body inferiorly
Normal scapular lateral

Posterior shoulder dislocation

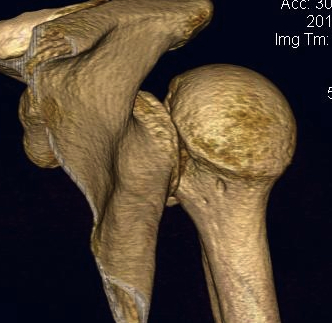
Posterior shoulder dislocations
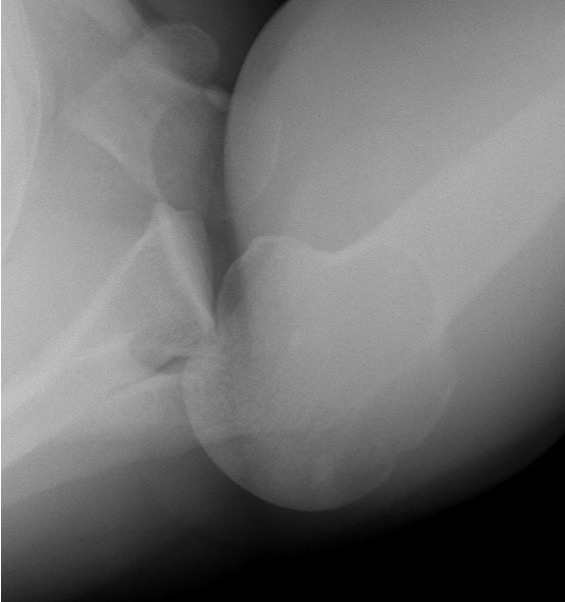
Axillary Xray
Diagnostic - humeral head posterior to glenoid with evidence of reverse Hill Sachs
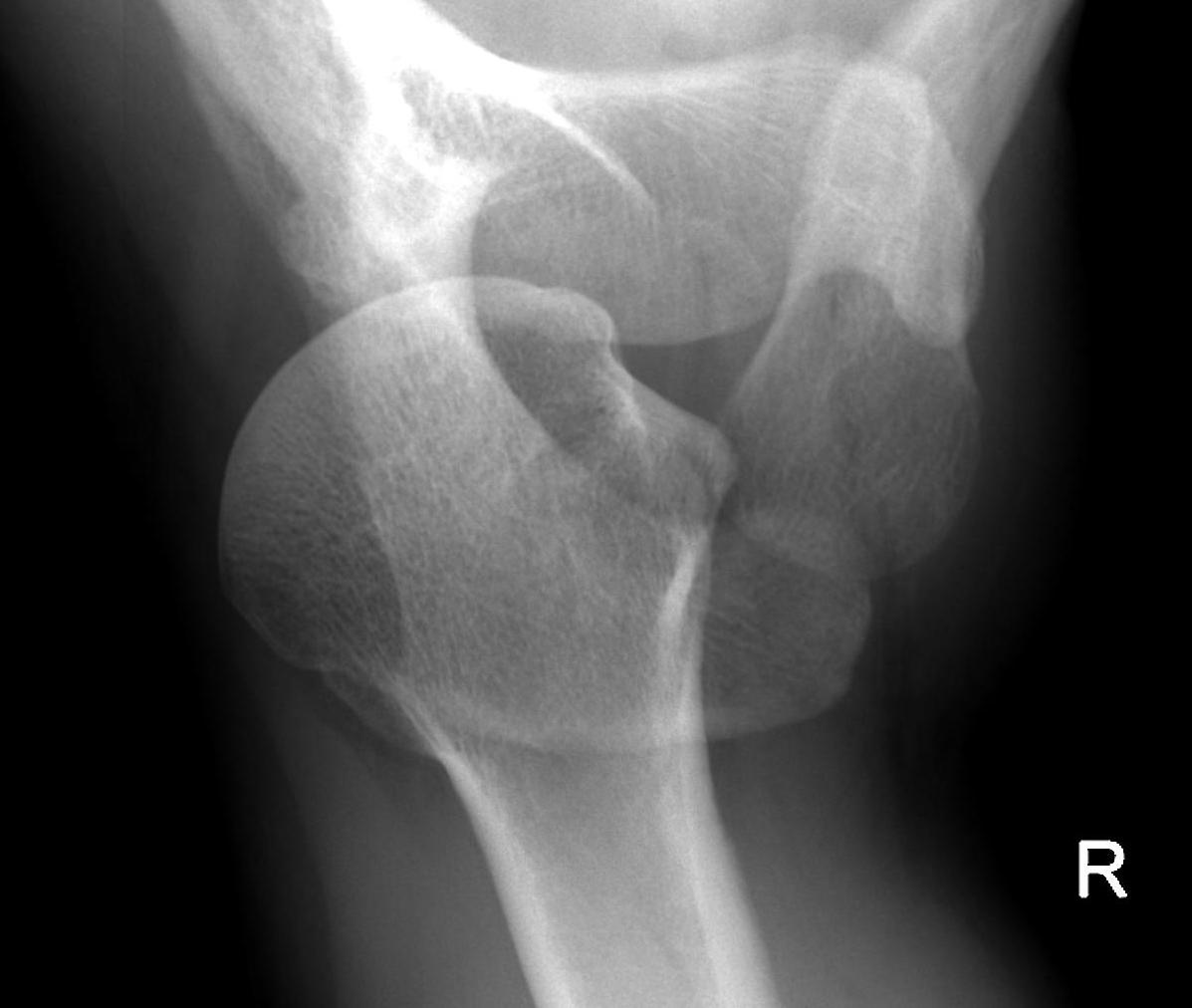
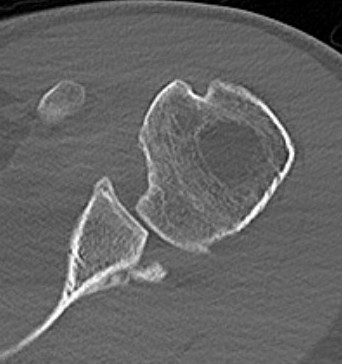
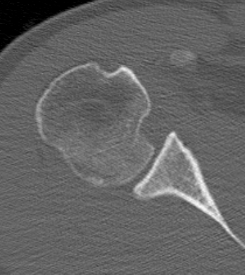
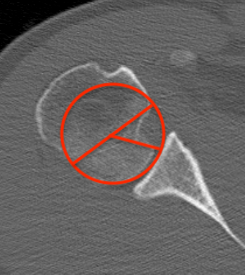
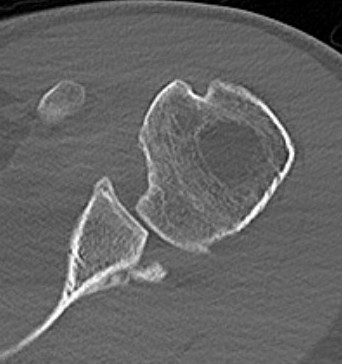
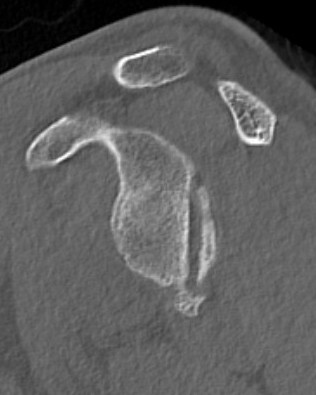
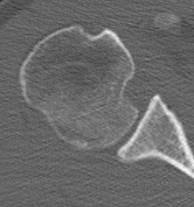
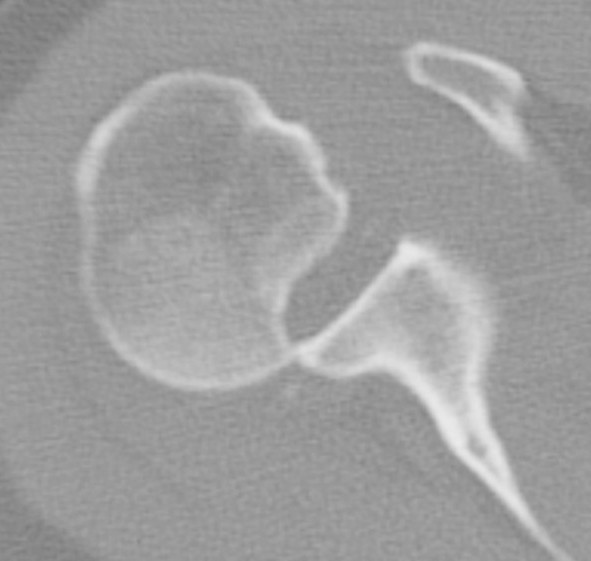
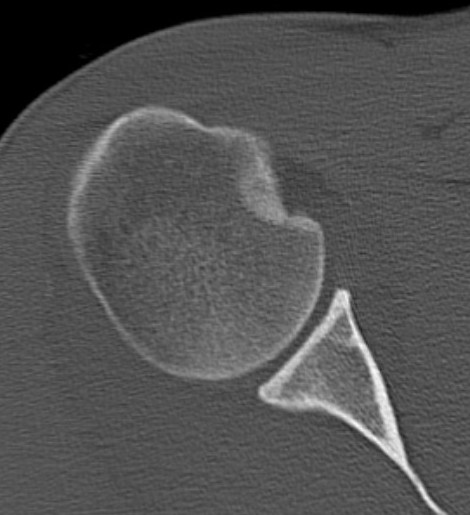
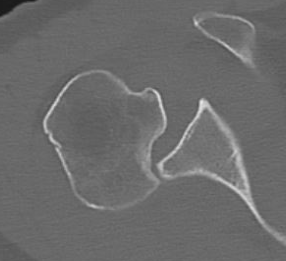
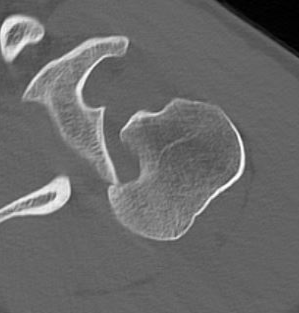
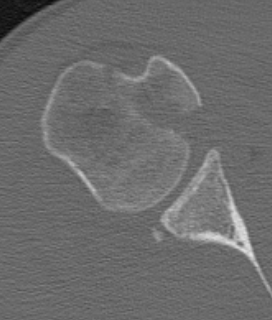
CT scan
Confirms dislocation


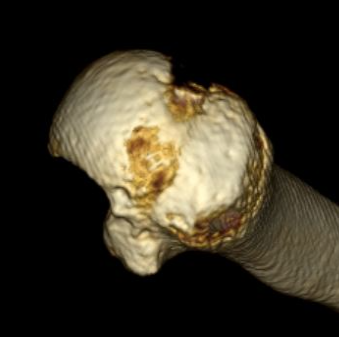
Reverse Hill Sachs
Humeral head defect
- caused by impaction of anterior humeral head on posterior glenoid
- intra-articular
- measured as a percentage of the articular surface
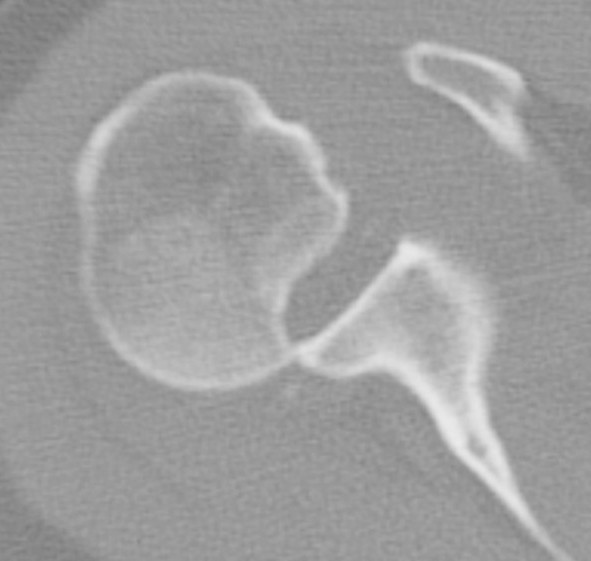

Lesser tuberosity fractures

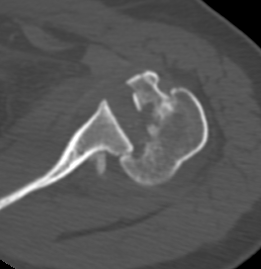

Posterior glenoid fractures / bony bankart

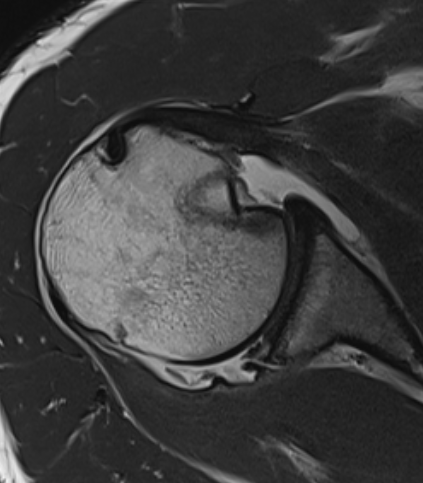
MRI
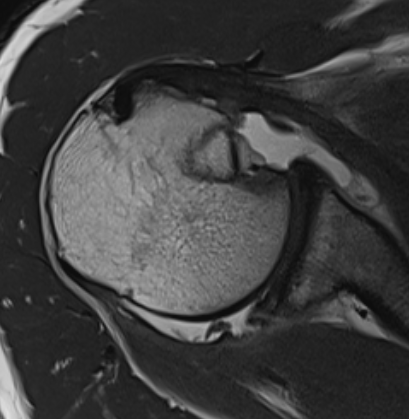
Acute MRI demonstrating reverse Hill Sachs and posterior labral tear
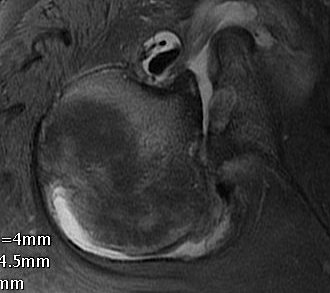

Chronic posterior shoulder dislocation with humeral head remodelling and glenoid bony deficiency
Management
Closed reduction
Issues that limit closed reduction
Chronic injuries > 2 - 4 weeks old
Locked dislocations - reverse Hills sachs lesion on glenoid rim
Large Hill Sachs defects - recurrent dislocation / instability
Technique
Conscious sedation
- arm adducted
- arm flexed to 90o
- increasing IR first to unlock head
- traction
Place into external rotation brace / gunslinger cast


Breg Arc and Donjoy X-ACT shoulder external rotation braces
Acute surgical management
Indication
Failure closed reduction / locked posterior dislocation
Recurrent dislocation - unable to maintain reduction in gunslinger / external rotation brace
Displaced lesser tuberosity fractures
Displaced posterior bony bankart fractures
Technique
Anterior deltopectoral approach - reduce humeral head
Address bony defects
- reverse Hill Sachs / anterior humeral head defect
- posterior bony bankart
Humeral head Defect Management
| Reverse Hills Sachs < 25% | Reverse Hills Sachs 25% - 40% | Reverse Hills Sachs > 40% |
|---|---|---|
|
Non operative Elevate and bone graft if acute Subscapularis / lesser tuberosity transfer |
Subscapularis / lesser tuberosity transfer Osteochondral allograft Hemicap |
Osteochondral allograft Arthroplasty |
 |
 |
 |
Subscapularis +/- Lesser tuberosity transfers
Indications
Defects 25%



Options
McLaughlin - subscapularis transfer into defect / makes defect extra-articular
Neer modification - lesser tuberosity + subscapularis transfer into defect
Technique
Vumedi modified McLaughlin video
Vumedi modified McLaughlin video 2
Results
- systematic review of modified McLauglin for locked posterior dislocation
- 9 studies and 97 shoulders
- reverse Hill Sachs 20 - 50%
- 100% union
- complication 1% (screw loosening)
- recurrent instability 2% (epileptic patients)
Osteochondral Allograft Reconstruction
Indication
Reverse Hills Sachs defects 25 - 50%
Technique
Video J Sports Med 2022 Reverse Hill Sachs Allograft
Surgical technique Reverse Hill Sachs Allograft PDF
Case 1: Lesser tuberosity osteotomy, removal comminuted articular fragment, insertion osteochondral allograft



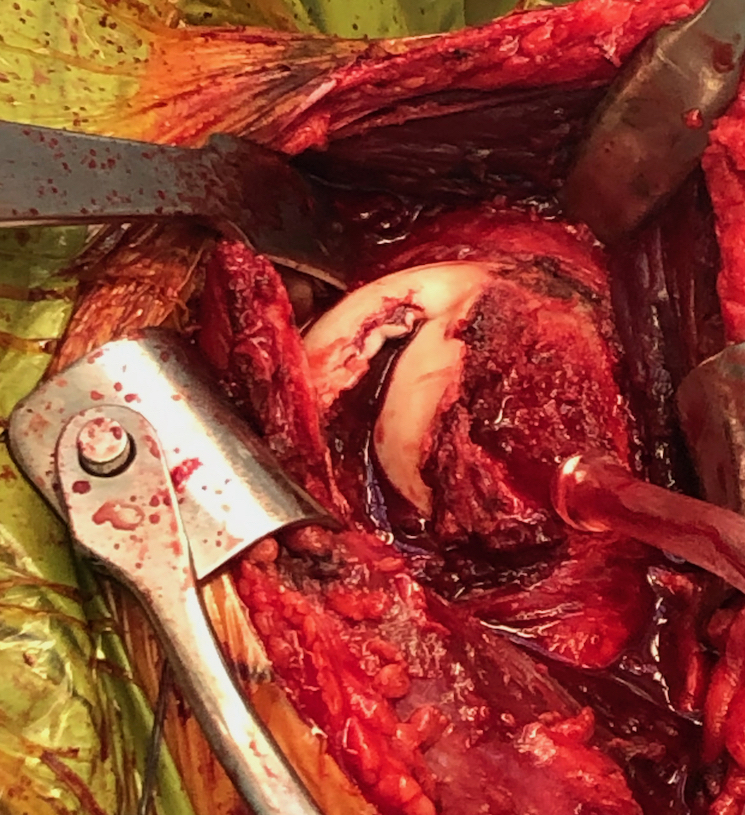

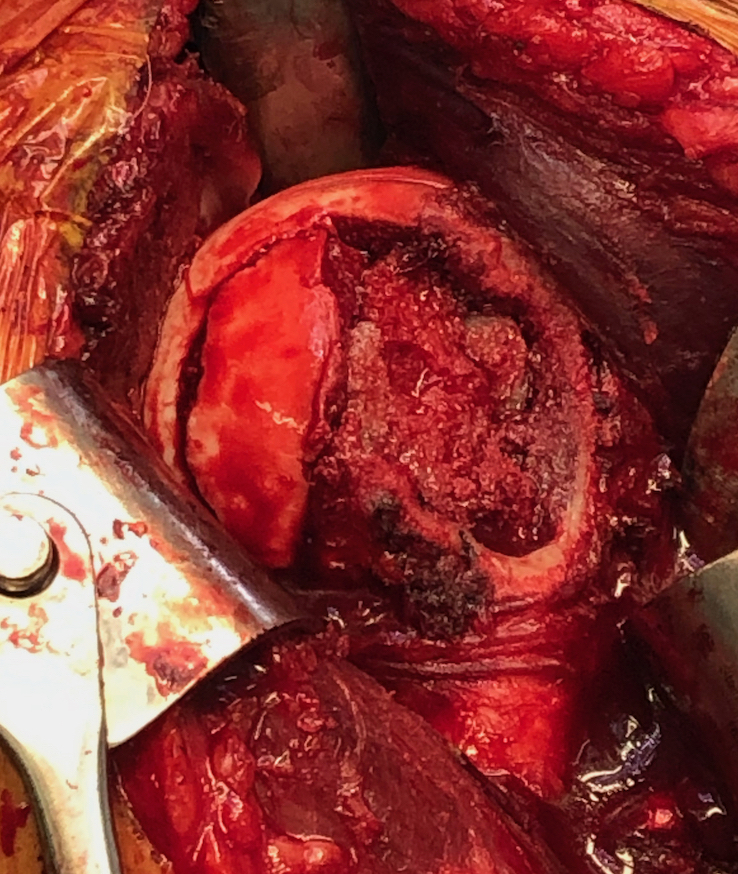


Case 2: Osteochondral allograft with anchor repair of subscapularis



Results
- systematic review of McLaughlin and humeral head allograft for reverse Hill Sachs
- 14 studies and 150 patients
- no difference in outcomes between 2 groups
- OA: McLaughlin 11%, allograft 21%
Lesser tuberosity ORIF

Hemiarthroplasty / TSR