Definition
Repeated dislocation of patella with minimal trauma
- 15-20% of paediatric acute patella dislocations
- more common girls
- often bilateral
Dislocation occurs unexpectedly when quadriceps contracted with knee in flexion
Direction
Usually lateral
Medial is usually iatrogenic
- excessive lateral release
- lateral release for incorrect reasons
- overtightening of medial structures
Anatomy
Ossification
Usually one ossification centre usually that appears at age 3 & closes soon after puberty
Facets
Retropatellar surface has 7 facets
- 3 on lateral side
- 3 on medial side
- 1 extra on medial side (odd facet)
Lateral surface larger than medial
- lateral cartilage thicker than medial
- medial & lateral separated by median ridge
Medial facet & odd facet are separated by another long ridge
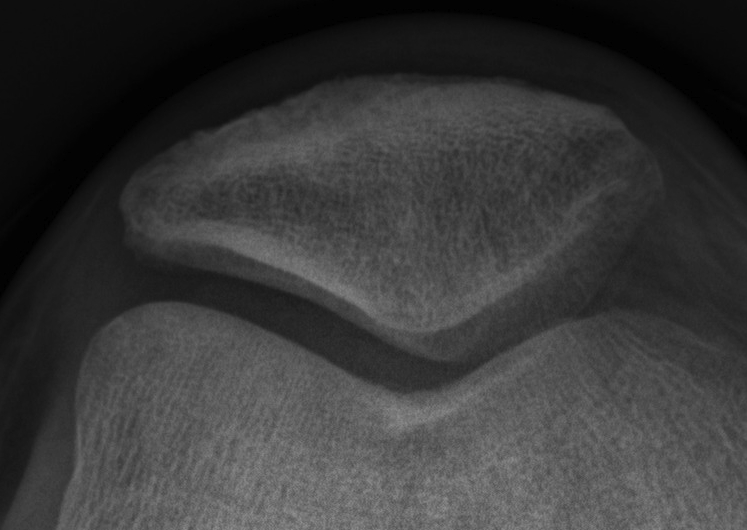
Tracking
Tracking is dynamic
- lateral in full extension
- more medial & central with flexion
Relies on normal static and dynamic stabilisers
Static Constraints
1. Bony contours of femur
- prominence of LFC anteriorly
2. Normal rotational profile
3. MPFL is constant / static checkrein to patella
Dynamic Constraints
Quadriceps is dynamic stabilizer
- VMO fibers attach to patella at 65° angle
Biomechanics Goodfellow 1976
0° No PF contact
20° Most distal part patella contacts trochlea
0-30° Median patella ridge lies lateral to the centre of the trochlea
30-60° Patella moves medially to be centered in groove
60-90° Deeply engaged in trochlear groove & is held by ST tension
90° Entire articular surface contacts except odd facet
>90° Patella tilts so that medial facet articulates with the MFC
135° Odd facet contacts lateral border of MFC
Aetiology Patella Instability
Complicated / Multifactorial
Valgus malalignment
Ligamentous laxity
Insufficient medial structures (MPFL rupture / medial retinaculum laxity / VMO atrophy)
Tight lateral retinaculum
Trochlea dysplasia
Patella alta
Abnormal rotational profile (femoral anteversion / external tibial torsion)
Bony
- patella alta / baja
- trochlea / patella hypoplasia / dysplasia
Soft tissue
- VMO atrophy / medial retinaculum laxity / torn MPFL
- tight lateral structures (capsule, retinaculum, ITB)
- ligamentous laxity
Alignment
- femoral anteversion
- external tibial torsion
- genu valgum
History
Pain
Beware unrelenting pain
- chondral damage
- patella tilt / lateral patella syndrome
Instability
Traumatic vs. atraumatic onset
Direction of instability
Age first dislocation
Subsequent dislocations
- mechanism, frequency
- ? voluntar
Treatment to date
Effusions
Examination
Generalised ligamentous laxity
Wynne-Davies Criteria
- positive if 3 of 5 bilateral signs
- hyperextension of the MCP joints parallel to forearm
- touch thumb passively to forearm
- elbows hyperextend beyond 0o
- knees hyperextend beyond 0o
- ankle DF > 45o
Patient Standing
Valgus Malalignment
Patella
1. Squinting patella
- with femoral anteversion patellae point inwards when standing
2. Grasshopper eyes
- patella sits high & lateral due to patella alta
Gait
In toeing
- internally rotated foot progression angle
- indicates femoral anteversion / tibial torsion
Patella Tracking
Patient sitting over side of bed
- flex and extend knee
- compare normal to abnormal side (if not bilateral)
J-sign
- lateral subluxation of patella as knee approaches full extension
- patella sharply deviates laterally in terminal extension
- indicates some degree of mal-tracking
![]()
![]()
Knee Examination
Previous incisions
VMO wasting
Effusion
ROM
- exclude extensive mechanism tightness
- symmetrical heels to buttocks
Knee extended (3)
1. Tenderness
- lateral retinaculum
- retropatellar space
- Bassett's sign (tender medial epicondyle / acute MPFL avulsion)
2. Clarke's Test / patella grind
- produces anterior knee pain with PFJ pathology
- compress patella and ask patient to contract quads
- very non specific test
3. Patellar tilt test


Evaluates tension of lateral restraint
- patient supine and relaxed with knees extended
- examiner's thumb on lateral aspect of patella
- lateral edge of patella elevated from the lateral condyle and medial edge depressed
Abnormal if unable to tilt lateral patella to horizontal
Knee flexed 30o over pillow (3)
1. Q (quadriceps) angle

Measurement
- line from ASIS to centre of patella
- line from centre of patella to tibial tuberosity
- angle subtended is Q angle
Values
- normal 10o men, 15o women
- abnormal if > 15o in males and > 20o in females
Causes increased Q angle
- femoral anteversion (squinting patellae)
- external tibial torsion
- lateral tibial tuberosity
- genu valgum
2. Sage mobility
Test at 30o flexion
- move patella medially and laterally
- graded in number of quadrants patella displaces
- > 50% displacement = insufficient restraints


Lateral glide
- >3 quadrants suggests incompetent med restraints
Medial glide
- > 3 suggests incompetent lateral restraint / hypermobile patella
- < 1 suggests tight lateral retinaculum
3. Apprehension test (Fairbank)
Patient supine and relaxed
- place relaxed knee at 30 degrees & push patella laterally as flex
- can also do with knee flexed over edge of bed
- positive test is a quads contraction & apprehension
Rotational Profile
Prone
1. Lateral border of feet
- if curved, metatarsus adductus
2. External tibial torsion
- intermalleolar axis > 30o
- Thigh foot angle > 15o
3. Femoral anteversion
- IR > 45o
- Gage's trochanteric angle > 15 - 20o


