Non-operative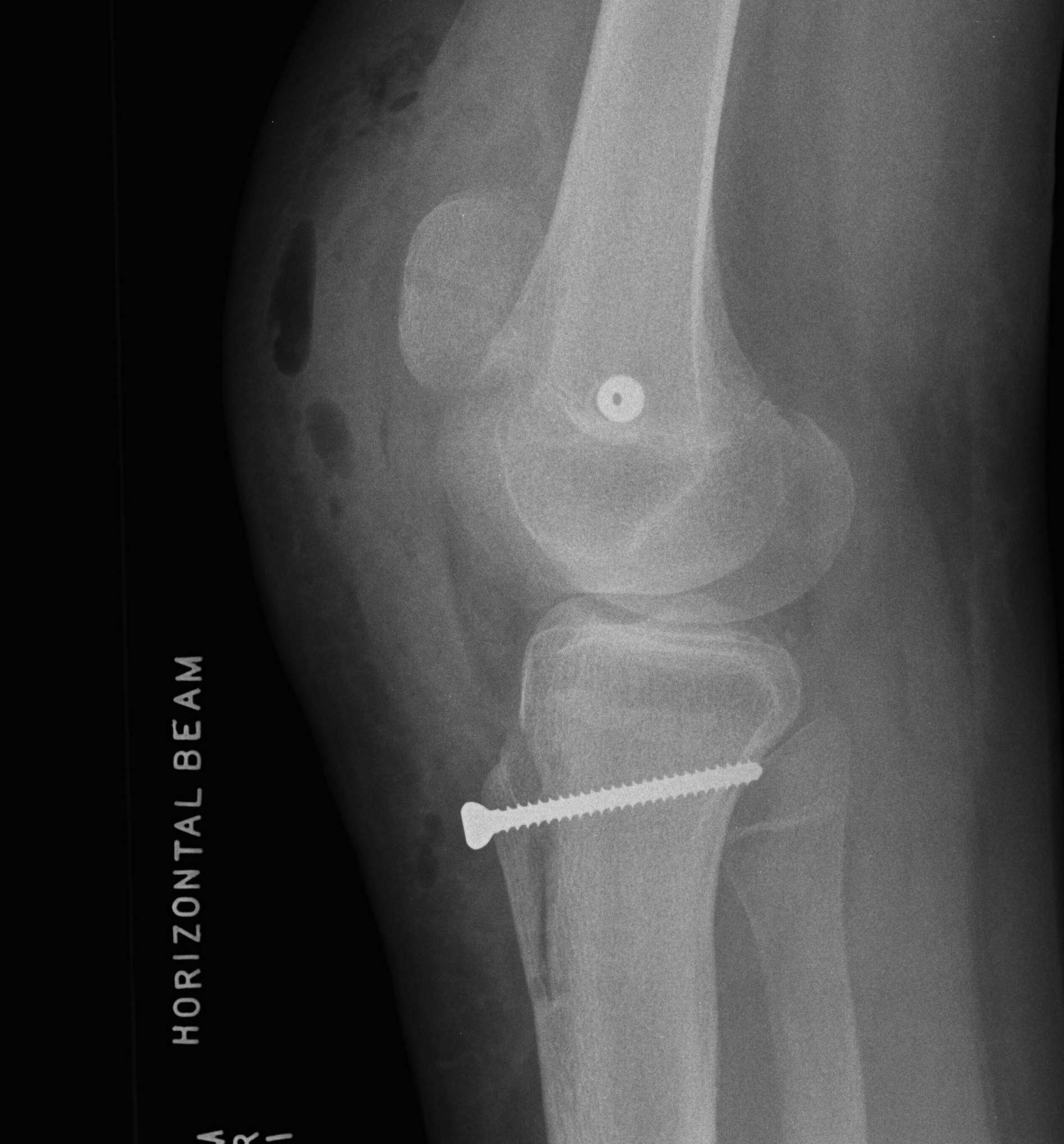
Results
90% respond
- very important
- 6 - 12 months minimum before offering surgery
Physiotherapy
1. Stretches
- quads stretches
- ITB
- lateral retinaculum
2. Quads strengthening
- avoid pain
- PFJ contact pressures lowest from 0-30o
- short arc quads extension
- closed chain VMO exercises
3. Taping / bracing
- patella cut out brace
- little hard evidence
- may provide proprioceptive feedback
Operative
Indications
For failure of non-operative treatment
- patella tilt with lateral patella pain
- recurrent instability
Options
Depends on pathology
- assessment and investigation critical for deciding treatment
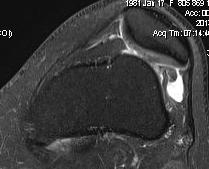
1. Isolated Patella tilt
Indications
- clinical and xray patella tilt
- no instability / malalignment
- excessive lateral pressure syndrome
Techniques
1. Arthroscopic lateral release
- knee in extension
- camera in AM portal
- hook diathermy in AL portal
- 5mm lateral to patella / 1cm superior to patella / down to anterolateral portal
- release retinaculum under vision
- must ensure SLGA coagulated / can visualise
- let down tourniquet at end of procedure
- ensure can evert patella 90o at end
2. Smiley knife release
- arthroscopy
- insert in AL portal
- divide retinaculum by feel
Post op
- drain 24 hours
- protect for 1 week
Results
McGinty et al Clin Orthop 1981
- 32/39 G/E results
Complications
A. Haemarthrosis
- can be major / problematic
- insert drain, splint and minimise activities first few weeks
- manage via early washout / insertion drain
B. Medial subluxation
- extending release too far into VL
- performing lateral release when have ligamentous laxity and instability
Patella subluxation / recurrent dislocation
Issues
- must have had long non operative period
- treatment depends on cause
- different treatment options in skeletally immature
Treatment algorithm
1. Recurrent subluxation + normal alignment (TTTG < 15 - 20)
- lateral release (only do if patella tilt / tight laterally or will dislocate medially)
- MPFL reconstruction / VMO advancement / medial reefing
2. Recurrent subluxation + malalignment (TTTG > 20)
- above + add TTT (tibial tuberosity transfer)
- Roux-Goldthwaite instead of TTT if physis open
3. Above + Excessive femoral anteversion
- consider DRFO (derotation femoral osteotomy)
4. Above + Excessive external tibial torsion (> 45 degrees)
- consider tibial derotation osteotomy
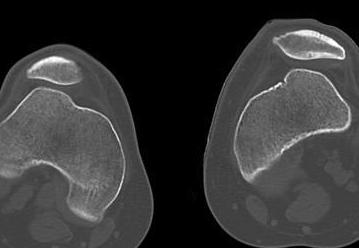
5. Trochlea dysplasia
- trochleoplasty
5. Patella alta
- distalise TT
Surgical Algorithm
1. Perform lateral release
- rarely needed
- most patients are ligamentous lax / hypermobile patella
- may be needed in chronic setting or if congenital
2. Perform TTT (if TTTG > 20)
- incision over TTT
- medialise at least 1 cm
- ensure some element of Fulkerson / anteriorise
- can distalise if patella alta
- secure with screws (2 x small fragment usually sufficient)
- reassess stability
3. MPFL reconstruction (with TTT, or if TTTG < 20)
- acts as checkrein to lateral displacement
- usually harvest hamstring autograft
- medial incision
- beware overtightening (will give pain) / patella fracture (drill holes in patella)
- reassess for stability
4. Lateral Trochlea Elevation
- still unstable after above operations
- small lateral incision
- beware fracturing lateral femoral condyle
- need to be able to take bone graft from iliac crest
Skeletally Immature
Roux-Goldthwaite
Indications
- skeletally immature with malalignment
Technique
- lateral half PT rerouted
- under medial PT
- stitched to MCL / sartorius
Technique Modification
Take medial half patella tendon
- suture to MCL
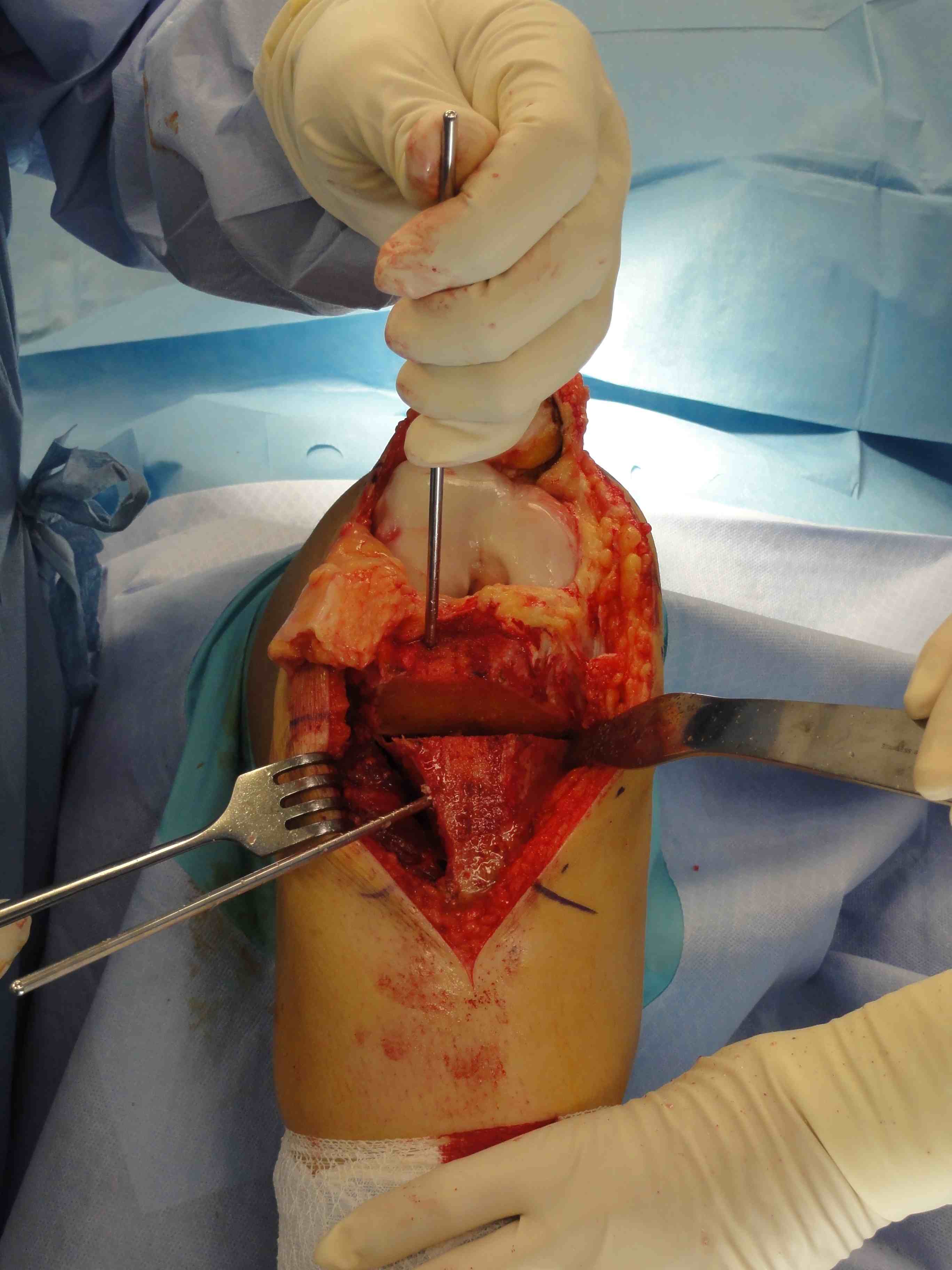
PT transfer + MPFL
- incision midway between PT and MCL
- identify patella tendon
- divide in two
- sharp dissection of medial half off bone
- dissect medially
- divide fascia and retinaculum to expose MCL
- suture to MCL with 2.0 non absorbable sutures
- through same incision can harvest hamstrings for MPFL reconstruction
Results
Fondren et al JBJS Am 1985
- 43/47 G/E results
Medial Operations
2. Medial imbrication
Indications
- MPFL needs to be intact or won't work
- laxity / stretched / attenuated structures
Technique
Insall procedure
- medial flap sutured 1 cm over lateral flap
Results
Scuderi et al JBJS Am 1988
- combined with lateral release
- normal and abnormal Q angle
- 42/52 G/E 81%
Barber et al Arthroscopy 2008
- TTT + medical plication in 34 knees
- 91.4% stability
Zhao AJSM 2012
- RCT MPFL v medial plicaiton
- 100 patients
- recurrent instability 7% v 16%
- better Kujala scores in MPFL
3. VMO advancement
Madigan procedure
- VMO detached and advanced laterally and distally
- sutured to fascia on patella
Trochleoplasty
Indication
- trochlea dysplasia
- if after MPFL and TTT the patella still unstable at end of case
Techniques
1. Dejour Trochleoplasty
- lift up anterior aspect femoral condyles
- deepening of trochlea
- replacement of LFC
- risk of chondral fracture / AVN / non union / displacement
Utting et al JBJS Br 2008
- 50/54 92%
- combined with other procedures as required
2. Elevate lateral edge of lateral femoral condyle
- insert osteotome
- gently elevate without fracturing chondral surface
- insert 2 - 3 mm of iliac crest bone graft
- no need for stabilisation
Results
Nelitz et al AJSM 2013
- trochleoplasty + MPFL in 26 knees
- no redislocation, no complications
- 96% statisfied
Tibial Derotation Osteotomy
Indication
- excessive external tibial torsion > 45 degrees
- 1 / 5000 people


Results
Drexler et al KSSTA 2013
- good outcome for 15/17 knees
Chronic Dislocation

Chronic / congenital
- patella subluxed out of joint
- patella alta
- treat with identical principles
- lateral release / TTT / MPFL reconstruction



