
Epidemiology
- 263 cases
- most aged 45 - 69
- 53% male
- 50% occurred during sport
- 66% avulsions displaced > 2cm
- 5% had sciatic nerve symptoms
Etiology
Violent contraction
- forced hip flexion with knee extended
Sporting injury
- water skiing
Anatomy
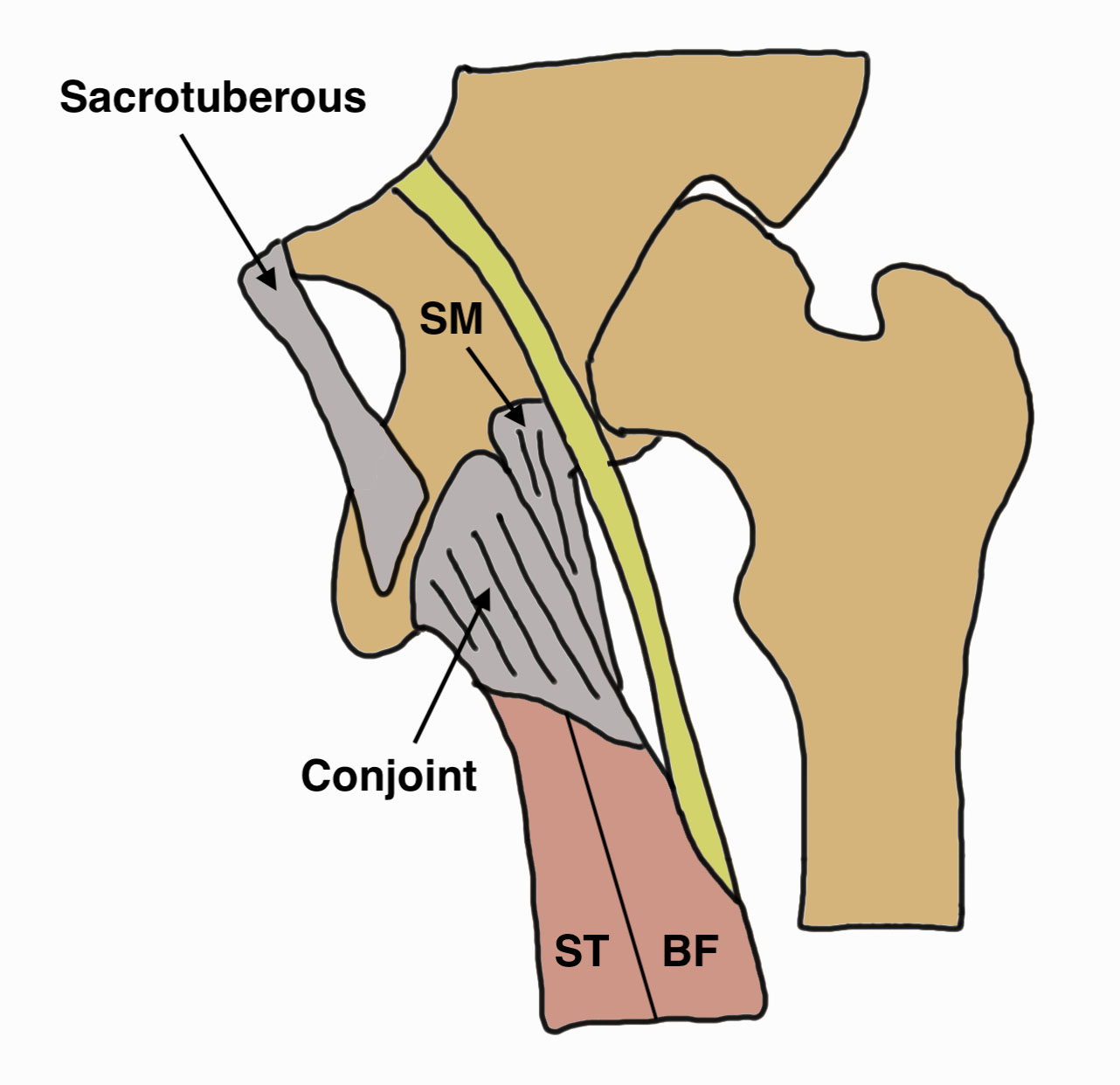
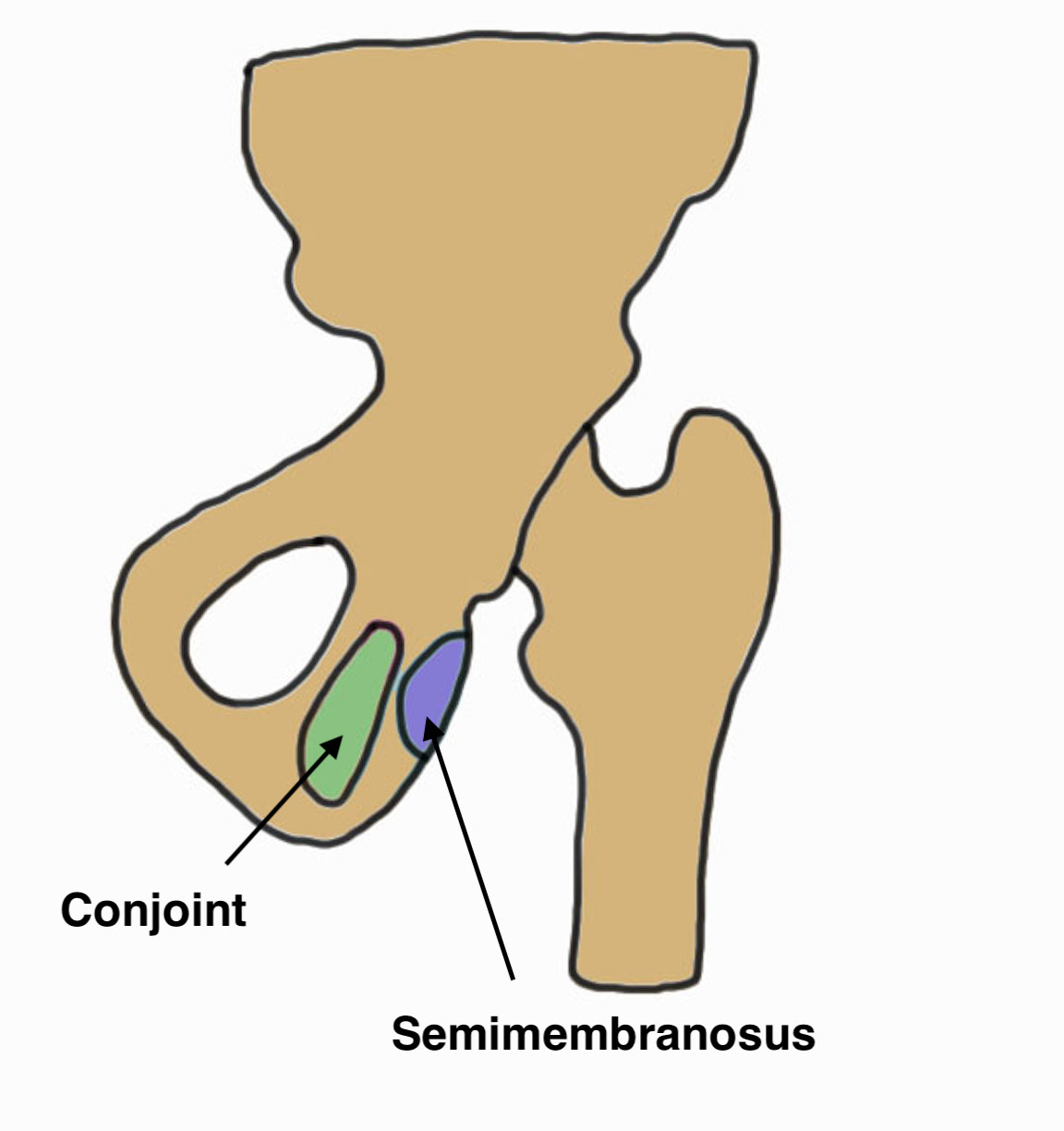

Hamstring by definition originate from the (lateral aspect of) the ischial tuberosity
Conjoint tendon
- biceps femoris and semitendinosus
- posterolateral aspect of the ischial tuberosity
Semimembranosus
- separate attachment
- anterolateral aspect of the ischial tuberosity
Symptoms
Sudden onset pain
Chronic tears
- weakness
- difficulty sprinting
Signs
Large haematoma / bruise down back of leg
Palpable defect
Distal retraction of muscle into thigh with contraction



Xray
Exclude bony avulsion
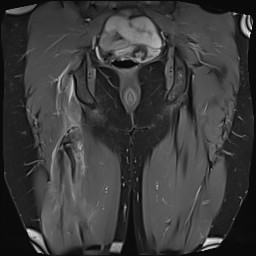
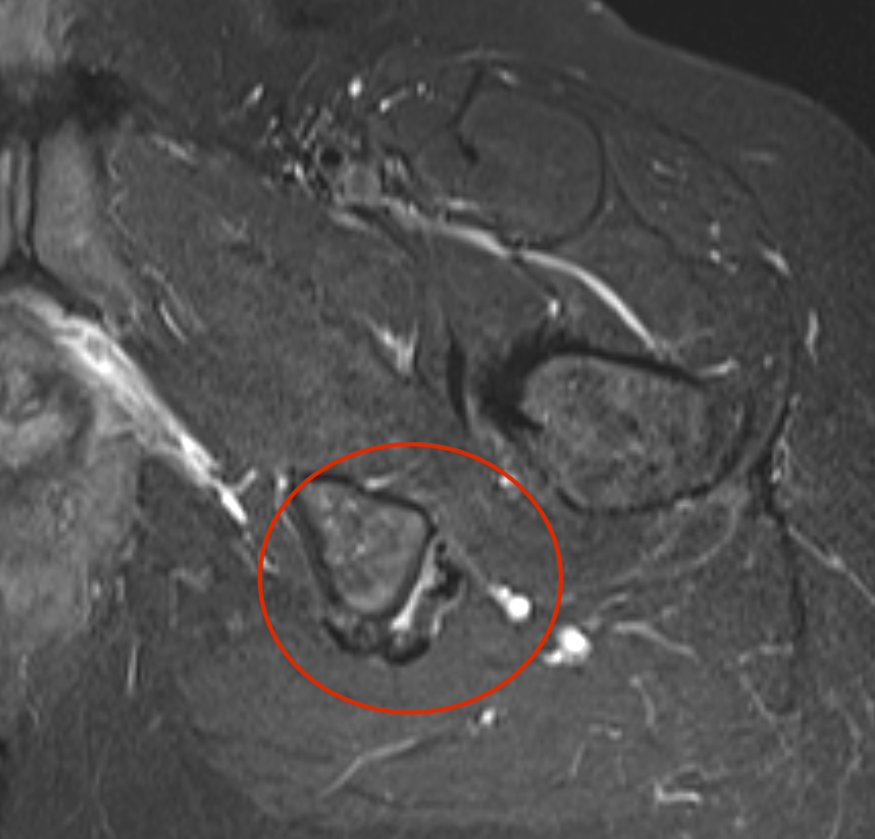
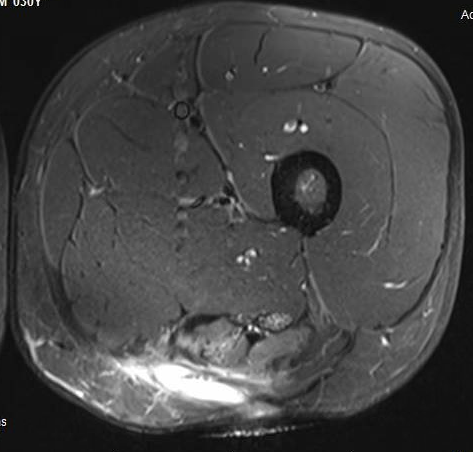
MRI
Complete / retracted tears
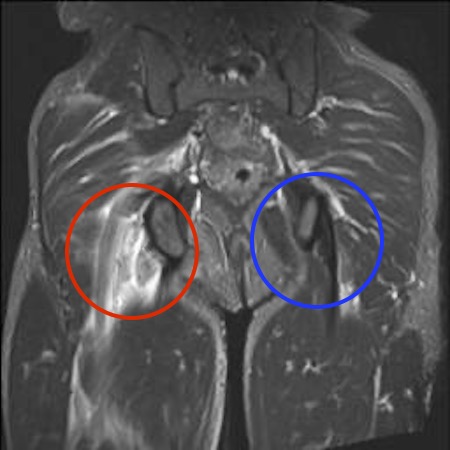
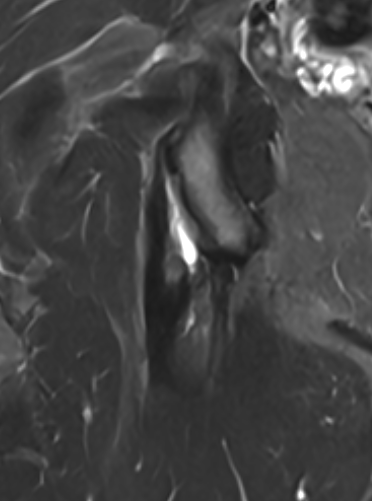
Proximal hamstring tear on right (red circle), normal insertion on tuberosity on left (blue circle)

Proximal hamstring avulsion on right - red circle is retracted hamstring tendon, blue circle is normal insertion on left
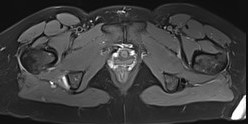
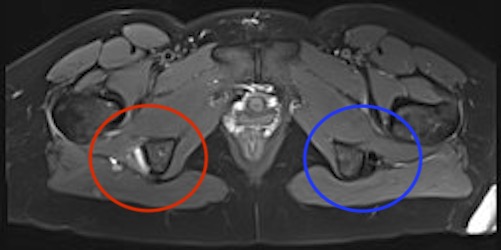
Proximal hamstring tear on right (red circle), normal insertion on left (blue circle)
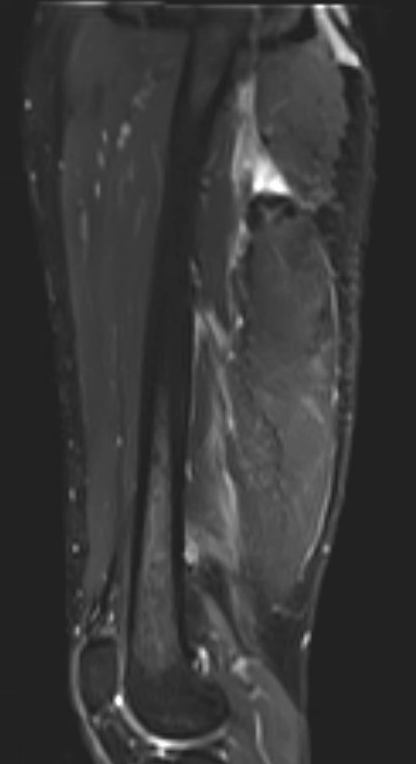
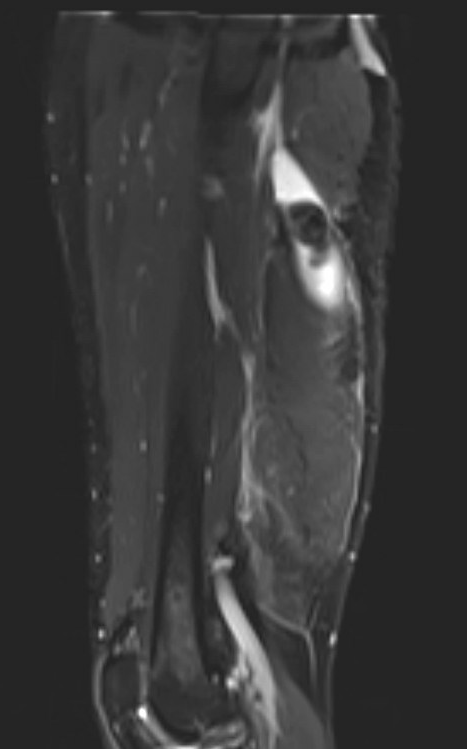
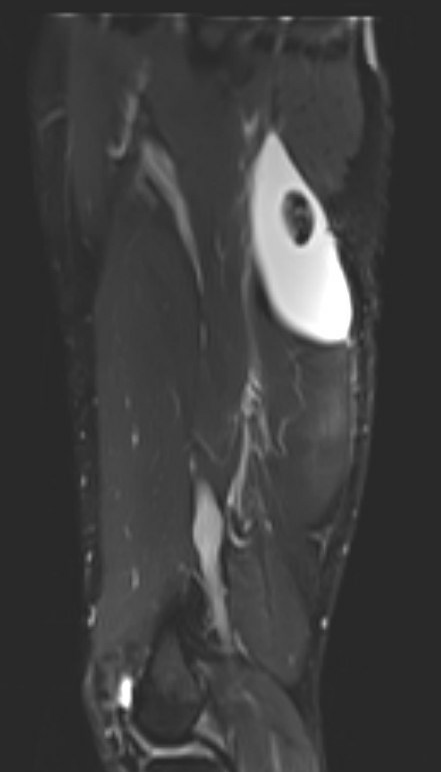
Proximal hamstring avulsion, with tendon floating in hematoma / seroma
Incomplete tears
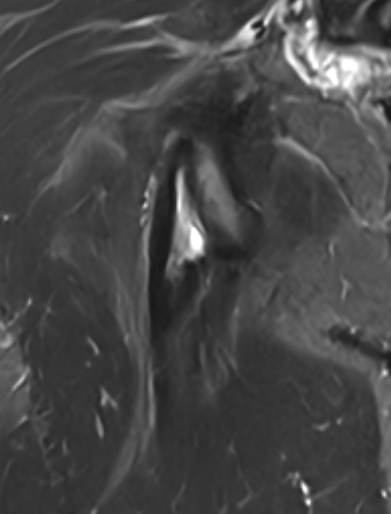
High grade partial tear proximal hamstring
High grade partial tear proximal hamstring
Classification
Type 1: Osseous avulsions
Type 2: Tear at the musculotendinous junction
Type 3: Incomplete avulsion from bone
Type 4: Complete avulsion with only minimal retraction
Type 5: Complete avulsion with retraction > 2 cm
Management
Operative versus non operative management
- systematic review of 24 studies and 800 proximal hamstring avulsions
- satisfaction: operative 90% versus nonoperative 53%
- strength: operative 85%% versus nonoperative 64%
- functional score: operative 73% versus nonoperative 70%
Non operative
Indications
- single tendon tears
- partial tears
- minimally retracted tears
- chronic tears
- low function individuals
Operative
Outcomes
Function
Hillier-Smith et al Bone J Open 2022
- 35 studies and 1500 surgically repaired cases
- 93% satisfaction
- mean functional outcome score 74
- mean strength 87% compared to other leg
- return to sport 85%
- rerupture rate 1.2%
- sciatic nerve dysfunction 3.5%
- better outcomes with acute repair or partial tears
Timing / chronicity
Shambaugh et al Orthop J Sports Med 2020
- 93 proximal hamstring repairs
- no difference in outcome < 3 weeks versus < 6 weeks
- increased weakness with repairs > 6 weeks compared < 6 weeks
Best et al Orthop J Sports Med 2021
- 204 cases proximal hamstring repairs
- worse outcomes with repair > 6 weeks
Partial tears
Kayani et al Am J Sports Med 2020
- 41 patients with incomplete chronic partial tears
- excellent outcomes with operative repair
Complications
Lawson et al Orthop J Sports Med 2023
- 43 articles and 2800 surgically repaired proximal hamstring avulsions
- major complication rate 4.6%
- 1.7% sciatic nerve injury
- 1% seroma / 1% superficial infection, 0.4% deep infection
- 0.8% of DVT / PE
- 2.4% posterior femoral cutaneous nerve numbness
- 0.8% rerupture
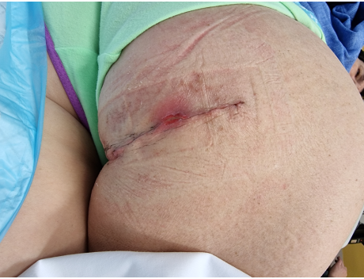

Postoperative infection
Surgical Technique
Vumedi/proximal hamstring repair
Vumedi/chronic proximal hamstring repair
Vumedi/high grade avulsions proximal hamstrings
Position
- patient prone with knee slightly flexed
Incision
- longitudinal incision - better for retracted or chronic injury, find and protect sciatic nerve distally
- horizontal incisions - can use in more acute setting

Superficial dissection
- divide fascia in line with incision
- preserve posterior femoral cutaneous nerve
- identify and elevate inferior edge of gluteus maximus
Deep dissection
- identify and preserve sciatic nerve (lateral to hamstring)
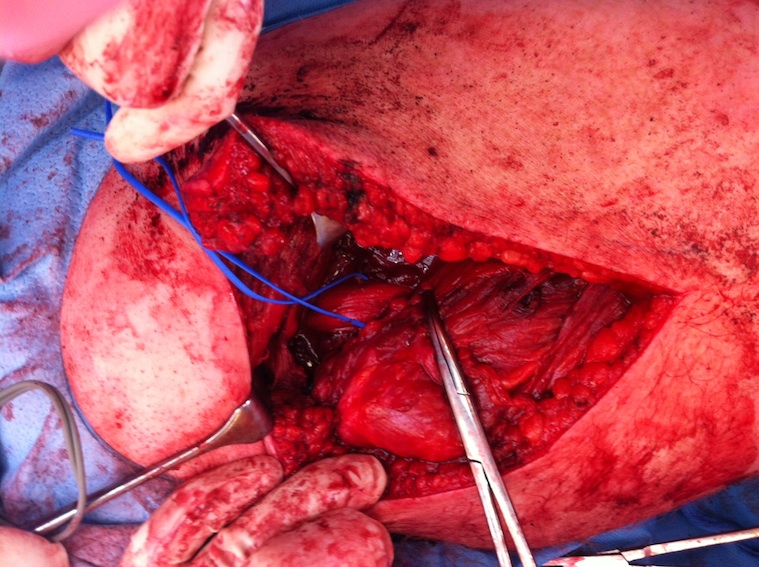
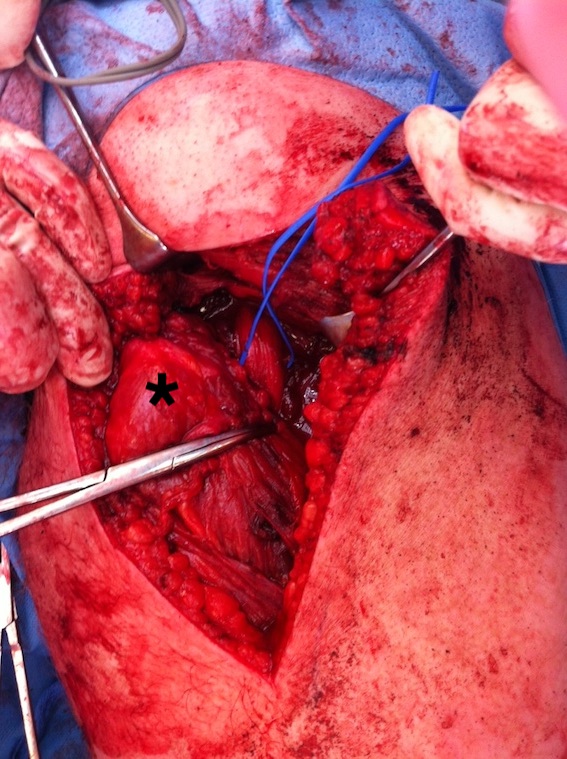

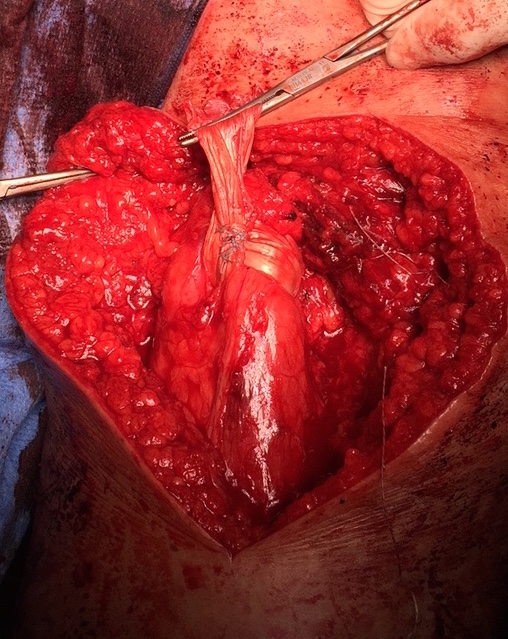
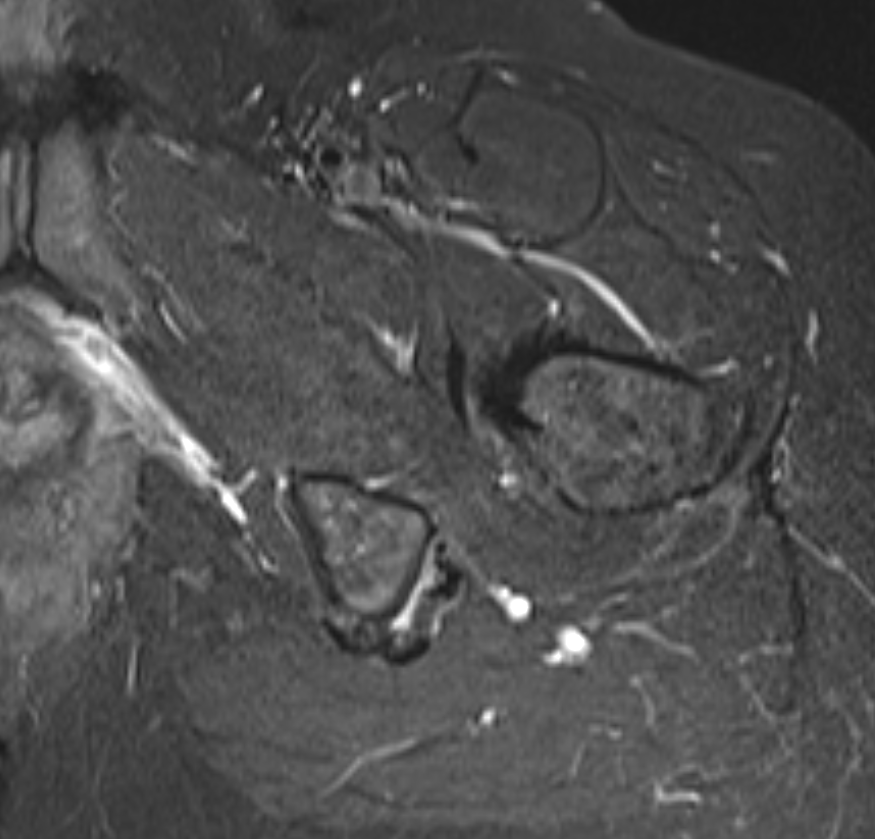
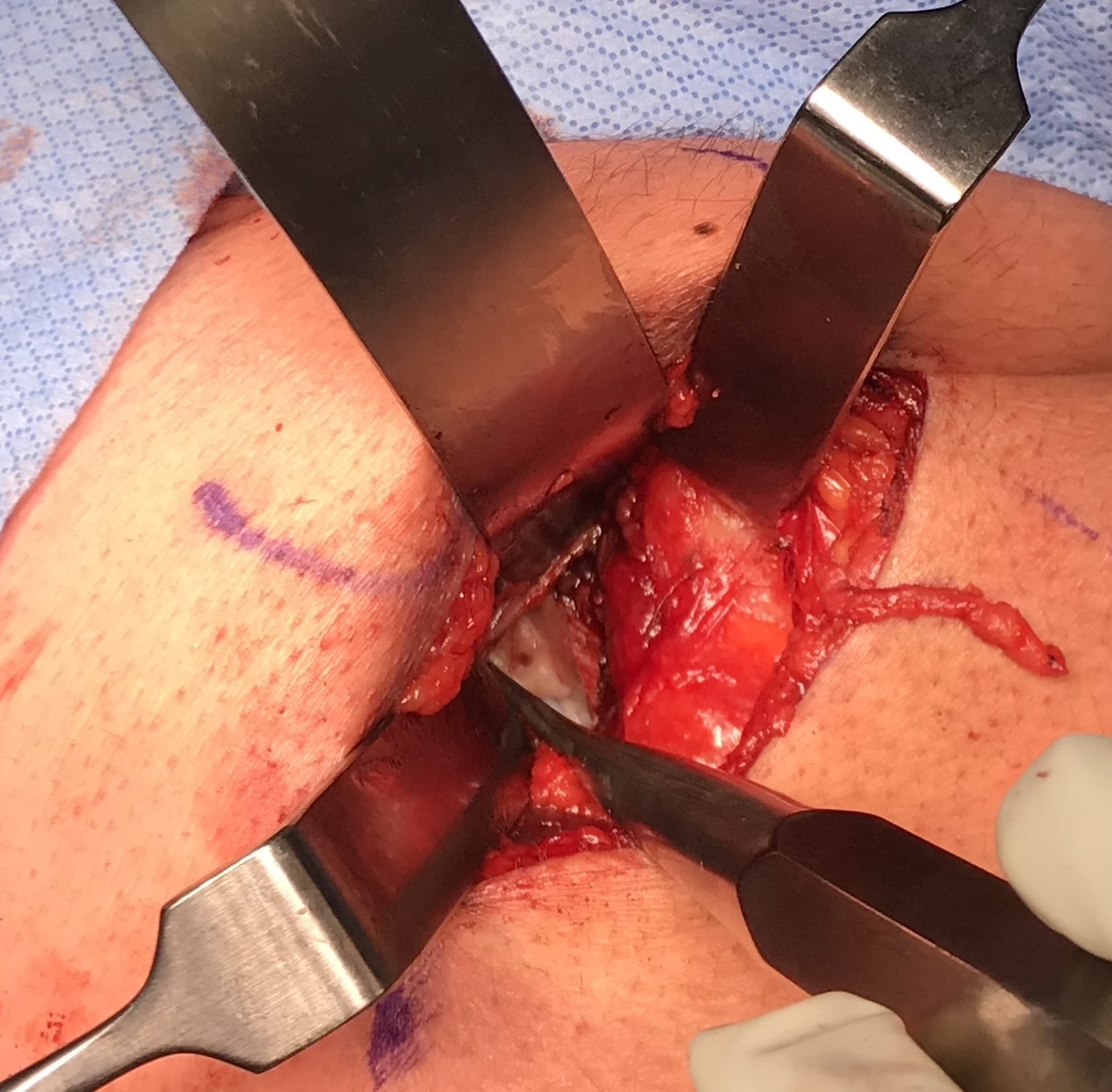
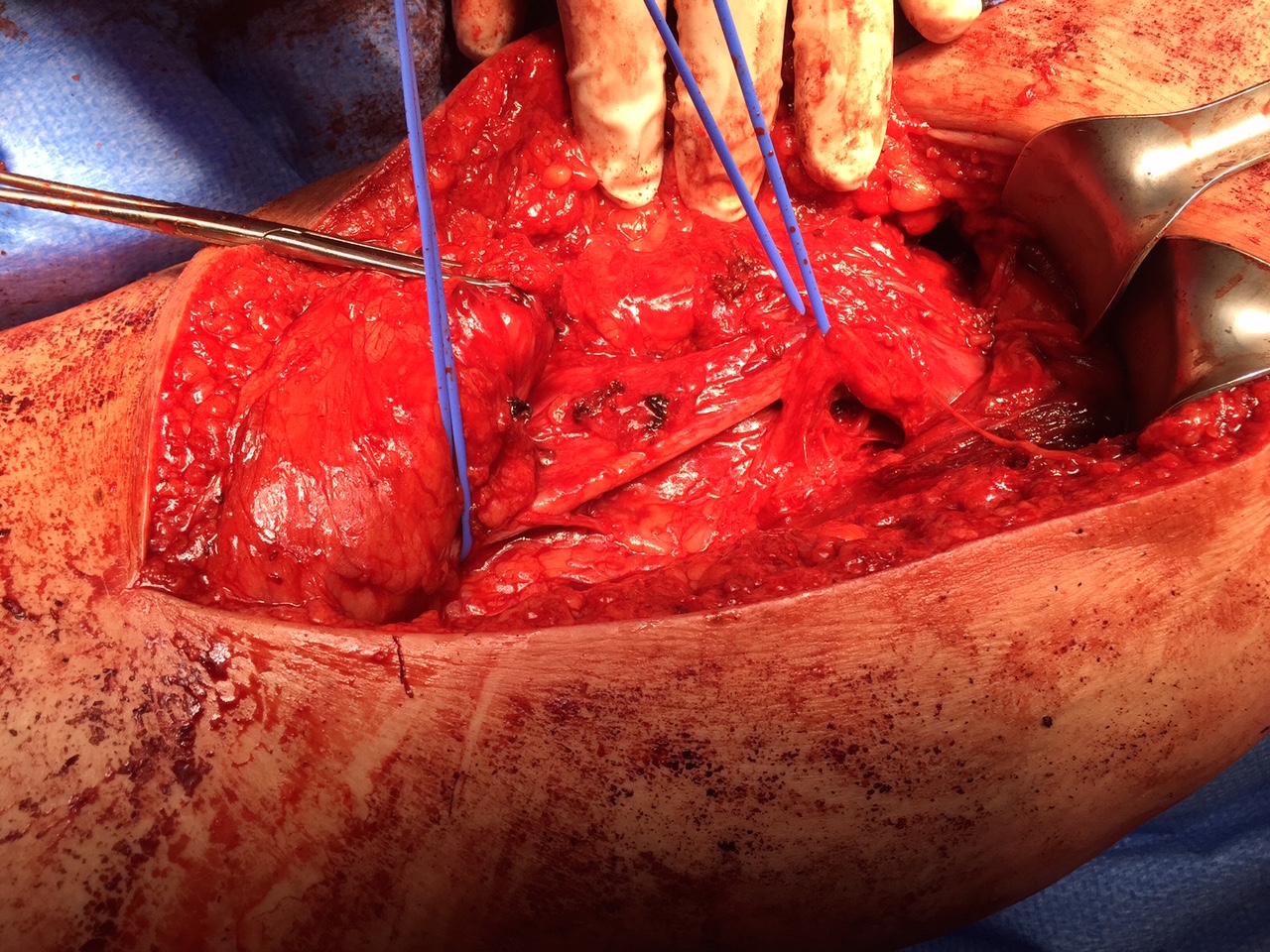
Hamstring (*) with sciatic nerve lateral to hamstring (blue vessiloop)
Identify and release proximal hamstring tendon
Stump of the conjoint tendon (*)
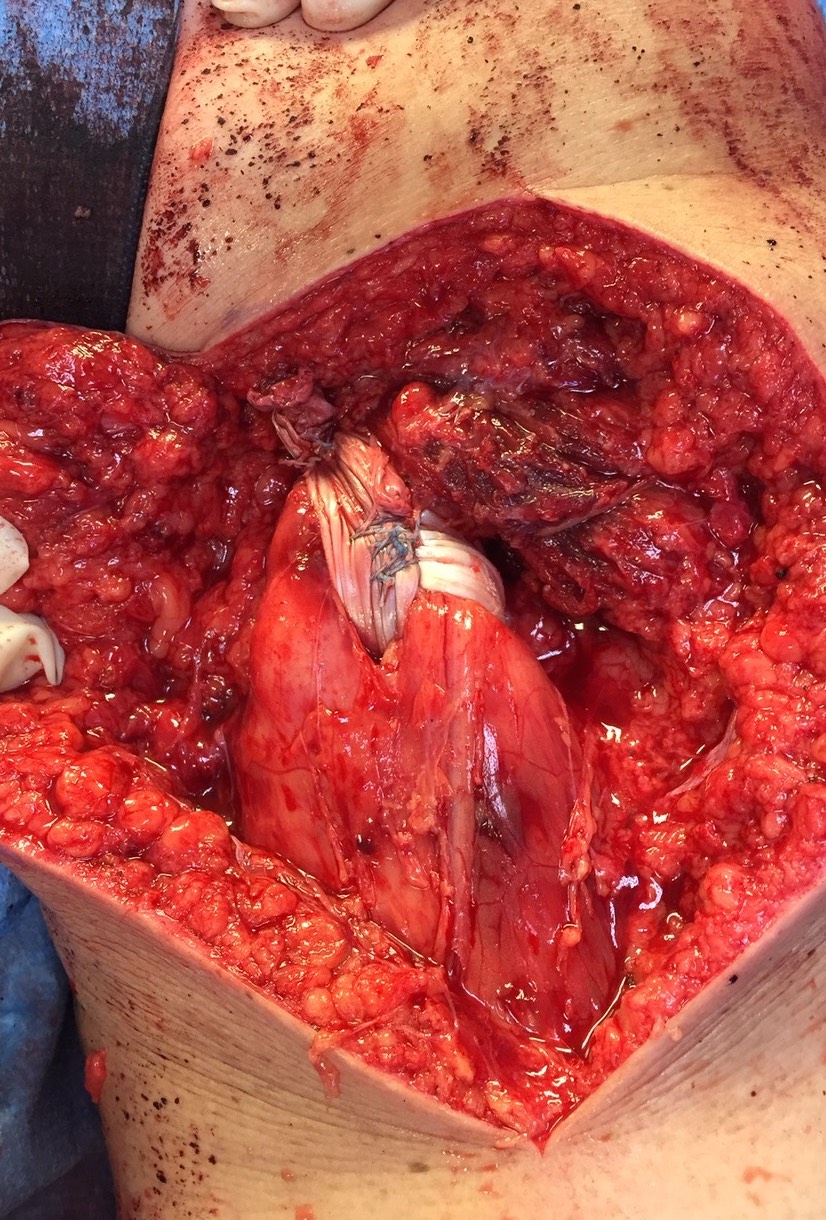
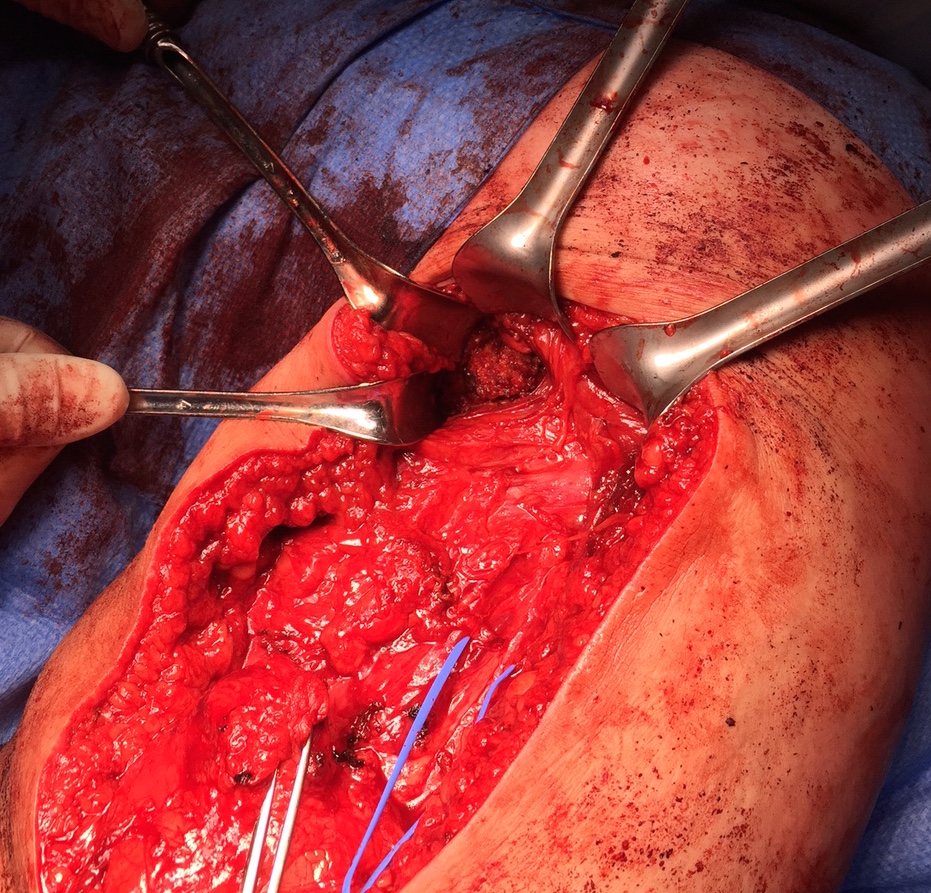
Expose ischial tuberosity
- superior retractor on ischial tuberosity
- medial and lateral retractors, care with sciatic nerve
- use osteotomes to create bleeding
- 2 - 3 suture anchors, double loaded
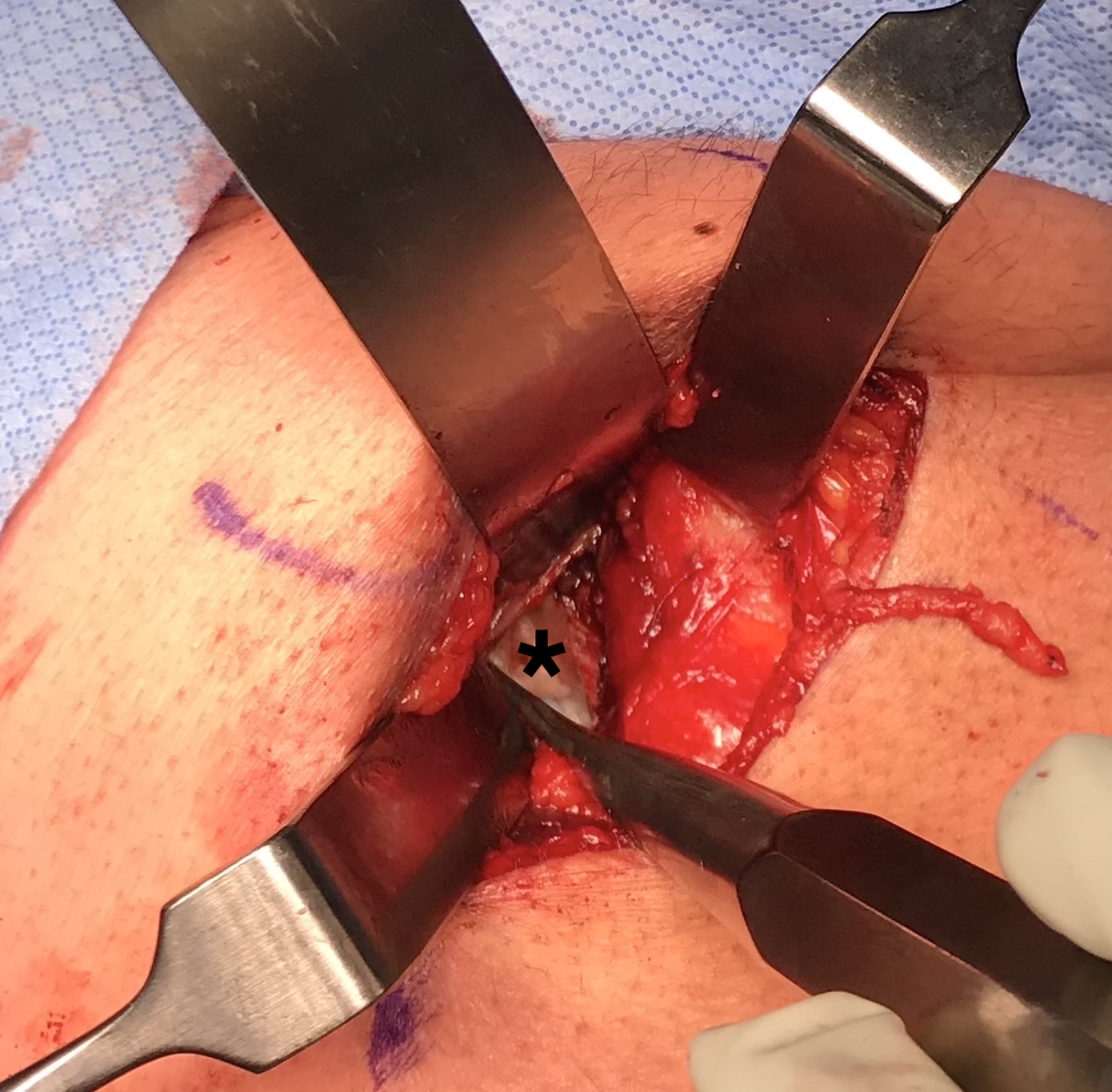
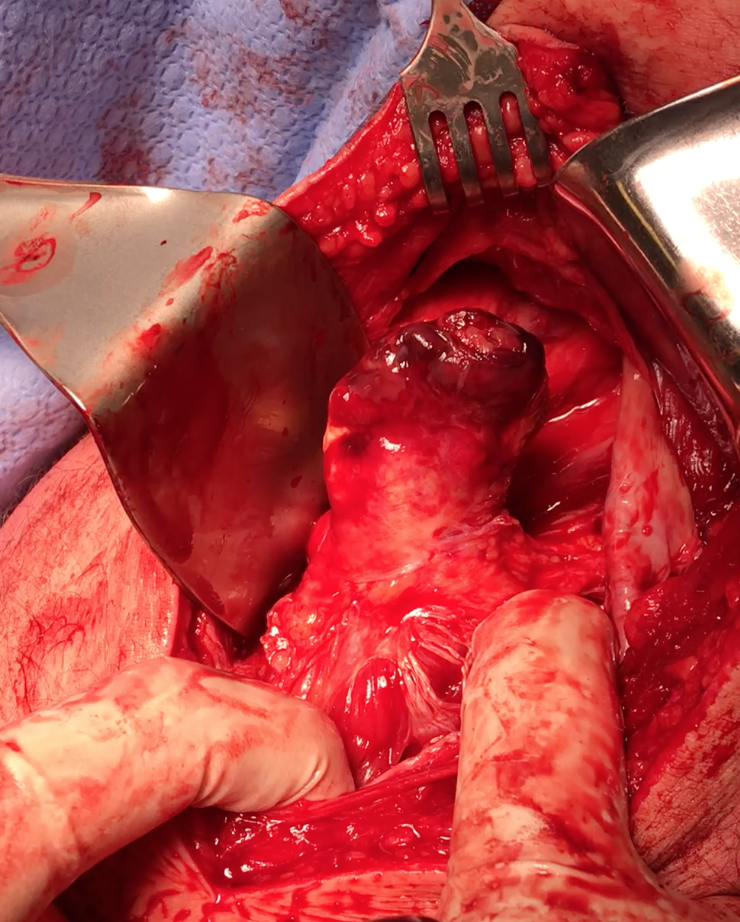
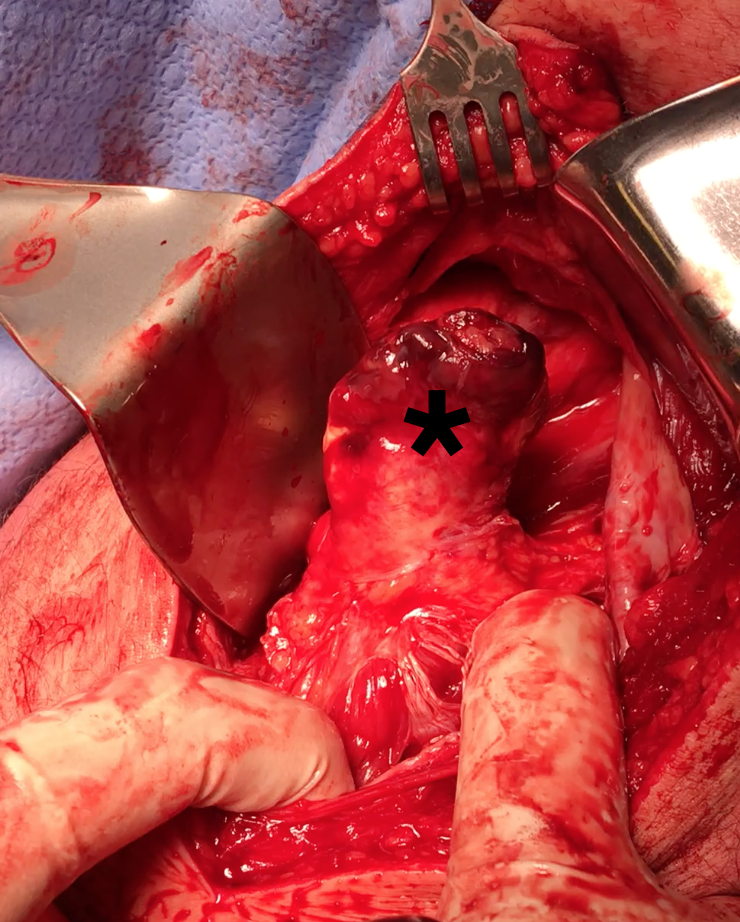
Exposing ischial tuberosity (*) with Cobb retractor
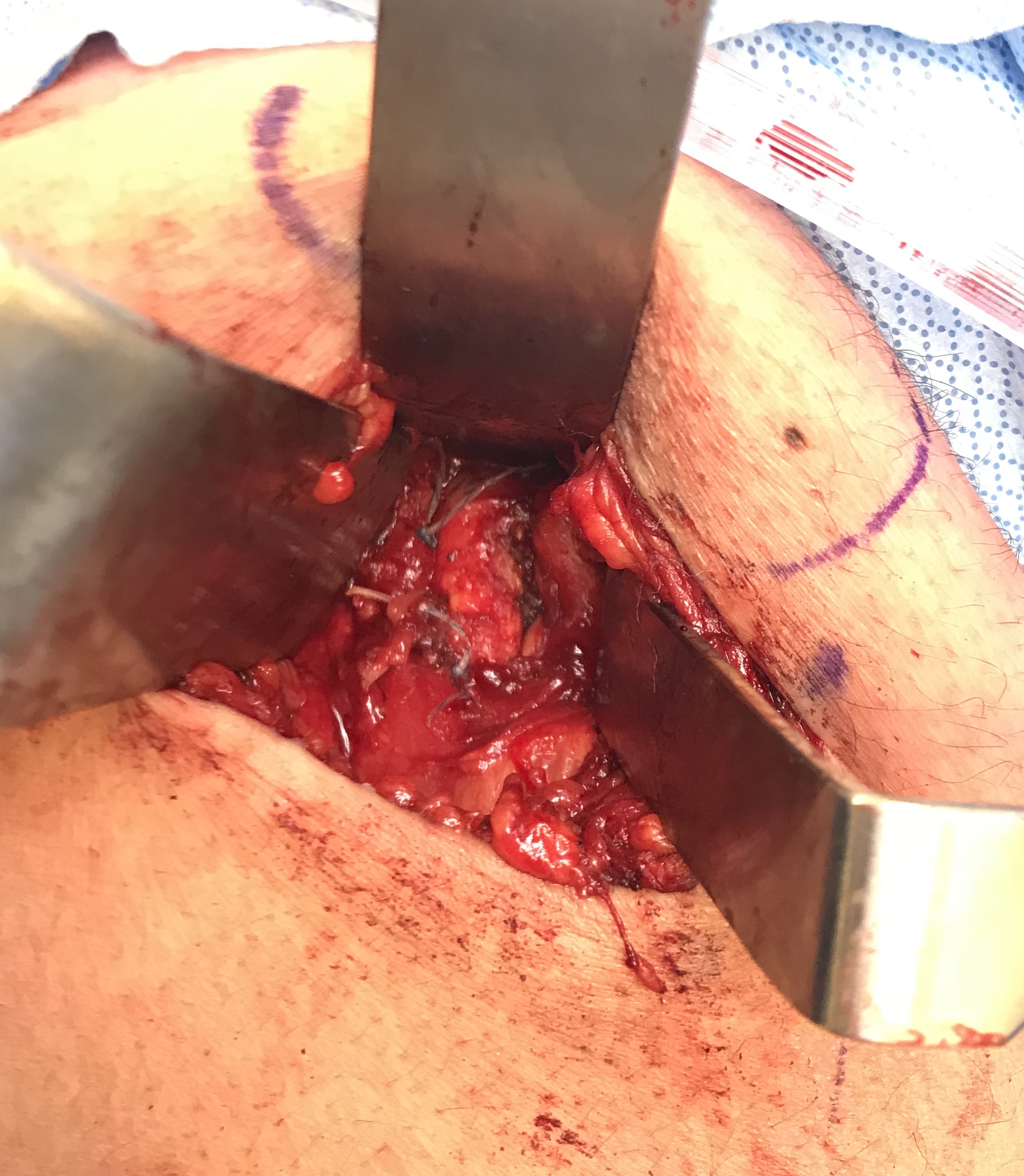

Post suture anchor repair
Post operative rehabilitation
- splint with knee flexed
- prevent hip flexion / knee extension
- crutches

Proximal Hamstring Reconstruction
Indication
Weakness / difficulty running
Technique
Identify and release sciatic nerve
Release hamstring
- see if hamstring will reach
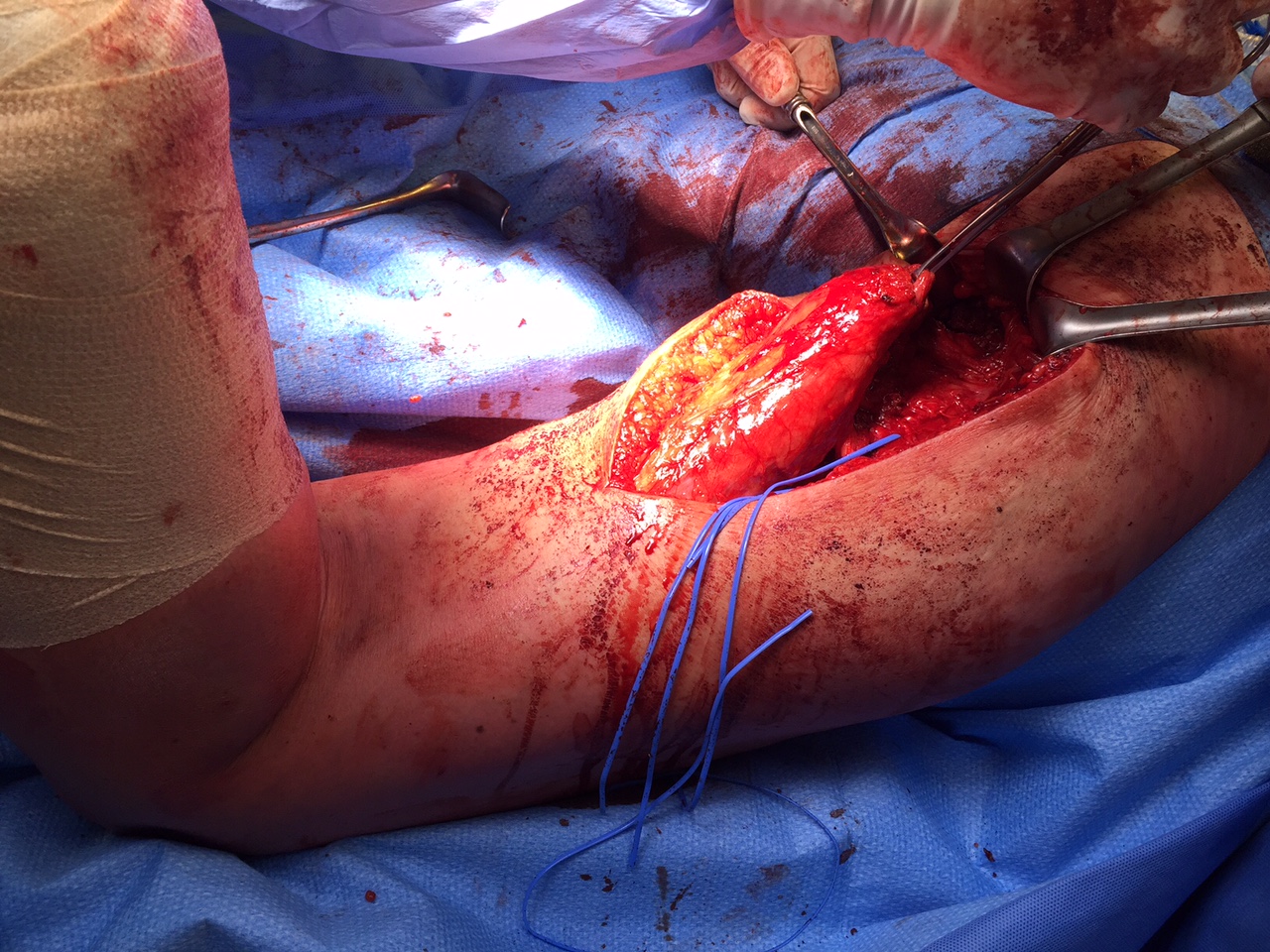
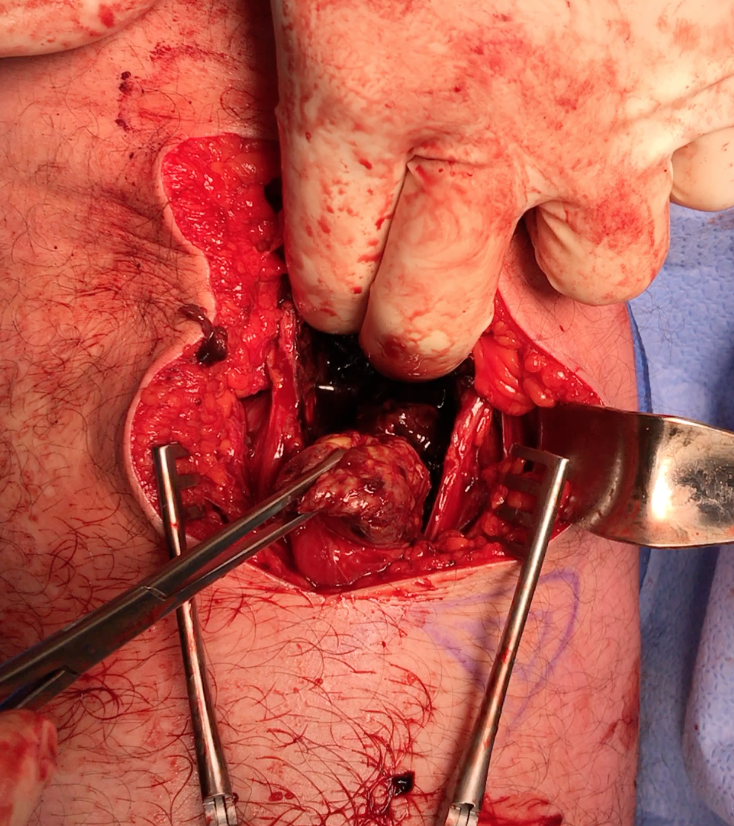
Sciatic nerve with blue vessiloops
Prepare allograft
- tendo achilles
- 9 x 20 mm bone block
- drill to 10 x 25 mm tunnel using ACL instruments
- ensure that beath pin does not advance
- secure with 7 x 20 mm screw, bone typically very strong
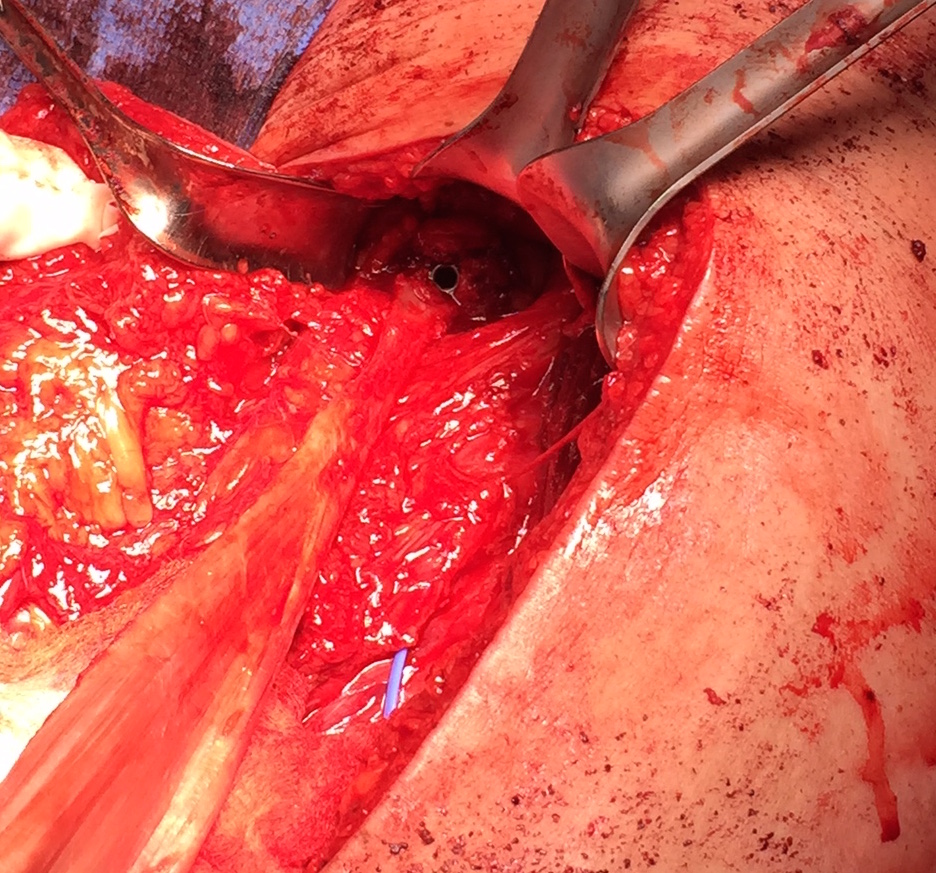
Ischial tuberosity exposed, then achilles bone block secured with screw
Pulvetaft weave tendon through the strongest, thickest part of the stump