

Mechanism
FOOSH (fall on outstretched hand)
Axial load with a valgus force
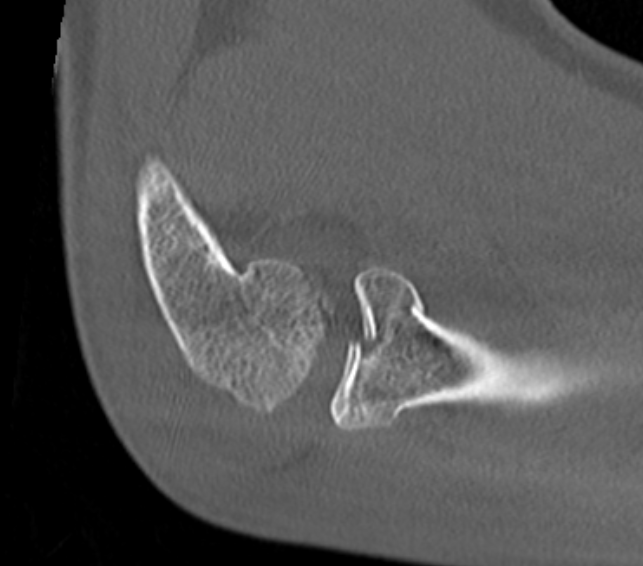
Anatomy
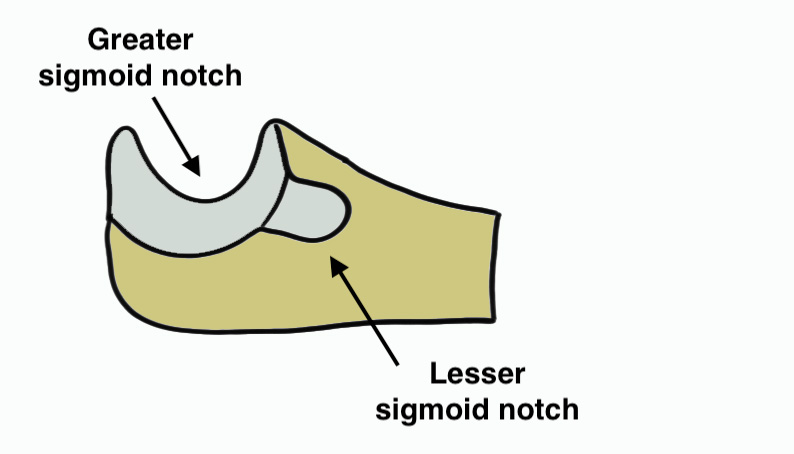
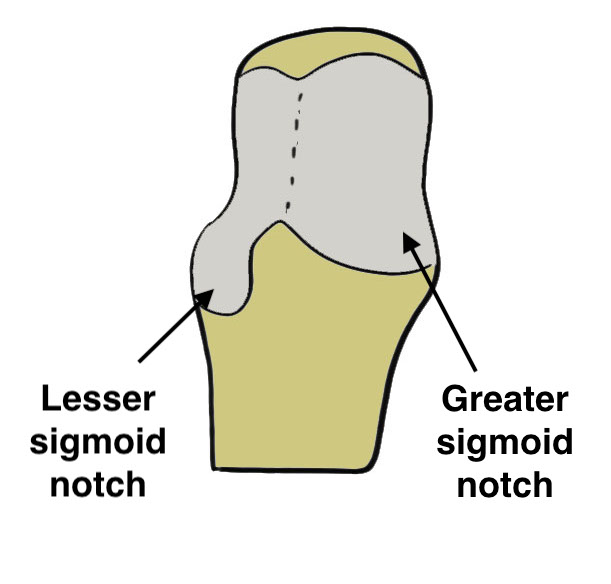
Radial head
| Articulation | Safe zone |
|---|---|
| Superior concave for articulation with capitellum |
Small non articulating portion of rim
|
| Rim articulates with lesser sigmoid notch of ulna |
110 degrees Between radial styloid and lister's tubercle
|
Lesser sigmoid notch articulation
Blood supply poor - single intra-osseous vessel
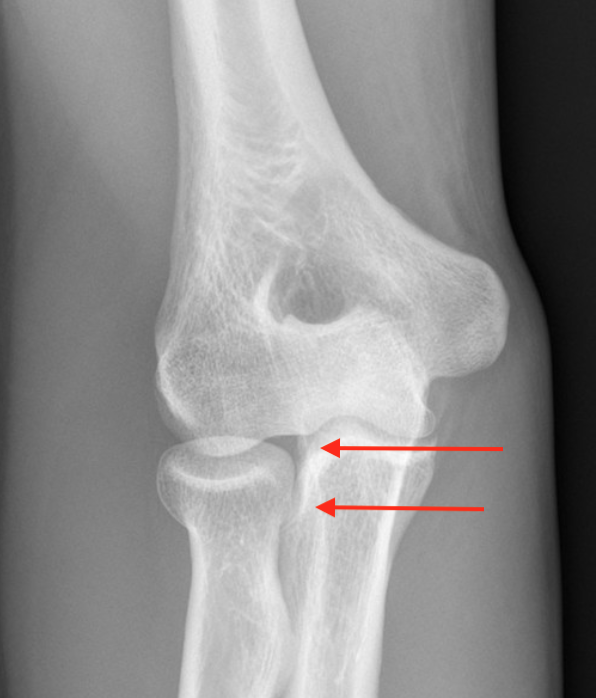
Hotchkiss modification of Mason Classification
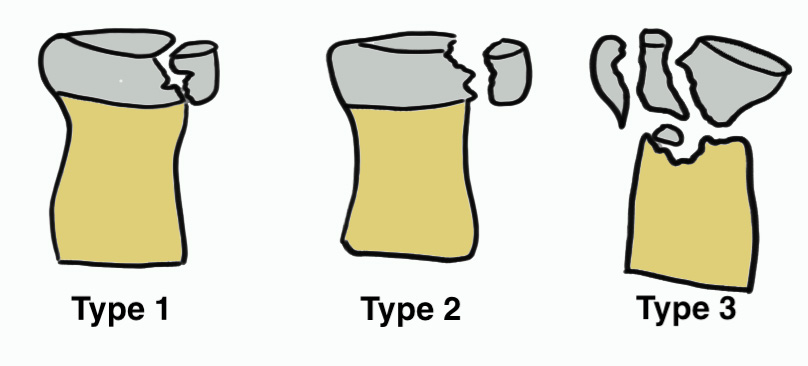
Type 1: Undisplaced fracture / Intra-articular displacement < 2mm/ No mechanical limitation to forearm rotation
If in doubt, inject LA into radiocapitellar joint / soft spot and rotate elbow


Type I radial head fractures
Type 2: Displacement > 2mm / Motion mechanically limited / Reconstructable


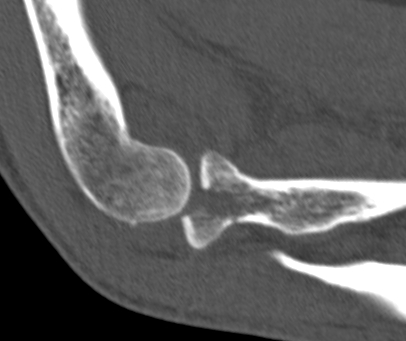
Type 2 radial head fractures
Type 3: Severely comminuted fracture / Non reconstructable

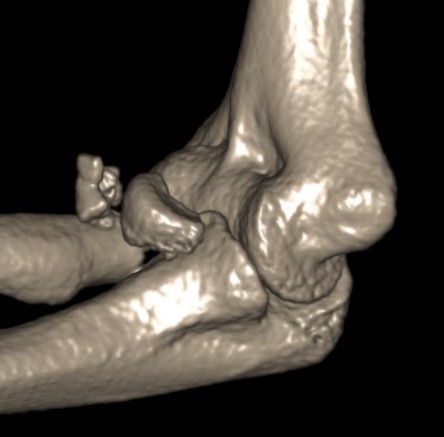
Type 3 radial head fractures
Type 4: Radial head fracture with elbow dislocation


Type 4 radial head fractures
Complicated Radial Head Fracture
1. Associated injuries
- MRI of 42 radial head fractures
- 24/42 (57%) elbows had LCL injury
- 1/42 (2%) had a MCL injury
- 16/42 (38%) had an injury of the capitellum
- 1/42 (2%) had a coronoid fracture
- 2/42 (5%) had loose osteochondral fragments
Conoid fractures
2. Elbow Dislocation
Terrible triad: radial head fracture, coronoid fracture, LCL injury
www.boneschool.com/elbow-dislocation
3. Essex Lopresti
Fracture radial head + disruption interosseous membrane + dorsal dislocation of DRUJ
www.boneschool.com/DRUJ-instability
Nonoperative Management
Indications
Mason 1
No block to rotation
Mason 2
- systematic review ORIF v nonoperative treatment for Mason II
- 11 studies and 319 patients
- ORIF: 90% good or excellent results, 7% reoperation, OA 5%
- nonoperative: 95% good or excellent results, OA 12%
- isolated partial radial head fractures displaced > 2 but < 5 mm
- 30 ORIF versus 30 nonoperative
- ORIF group younger and fragments more displaced
- better outcomes in nonoperative group
- 8 cases of mild HO in operative group, and 2 hardware failures
Operative Management
Indications for surgery
van Riet et al Should Elbow 2020
- mechanical block after hematoma aspiration
- displacement > 5 mm
- comminuted fractures (> 2 parts)
Options
Radial head fixation
Radial head resection
Radial Head Arthroplasty (RHA)
Chaijenkij et al Musculoskeletal Surg 2021
- meta-analysis
- 210 ORIF v 227 radial head arthroplasty v 152 radial head resection
- radial head arthroplasty had highest outcome scores and lowest complication rate
Kumar et al Indian J Orthop 2022
- systematic review of radial head resection v arthroplasty
- 6 comparative studies with 200 patients
- no significant difference in outcomes
- better ROM with excision
Approach options
| Kocher approach | Kaplan approach | Hotchkiss approach | Boyd approach | |
|---|---|---|---|---|
| Interval |
Between anconeus and ECU
|
Interval between EDC and ECRB |
Split EDC |
Elevate Anconeus and ECU Detach supinator from ulna |
| Disadvantage |
May risk injury to LCL |
May risk injury to PIN
|
May risk injury to PIN | May risk injury to PIN |
| Advantage |
May make LCL repair easier
|
Protects LCL | Protects LCL | Protects LCL |
Posterior Interosseous Nerve (PIN)
Gruenberger et al JSES Int 2022
- 45 cadavers with EDC splint
- used lateral epicondyle as landmark
- PIN 70 +/- 10 mm from lateral epicondyle
- PIN 40 - 48 mm from radiocapitellar joint
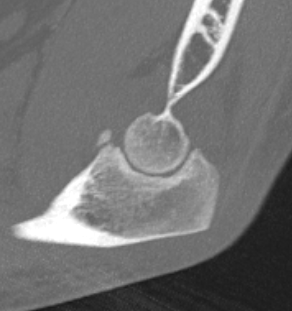
Radial Head Fixation


Indication
Significant fragment displacement
Reconstructable
Technique


Vumedi radial head ORIF video 2
Kocher / Kaplan approach
- dissect muscles off capsule
- divide capsule in line with incision / create anterior and posterior flaps
- pronate forearm to protect PIN
- no Hohmann retractors anteriorly and limit distal dissection
- reduce fracture
Identify safe zone for implants
- posterolateral portion of cartilage / yellow and thinner, non articulating cartilage
- 90o arc between radial styloid and Lister's tubercle
- 2.5 or 3.5 headless compression screws
Complications
PIN injury
Intra-articular screws
Hardware failure
Heterotopic ossification
AVN
Non union
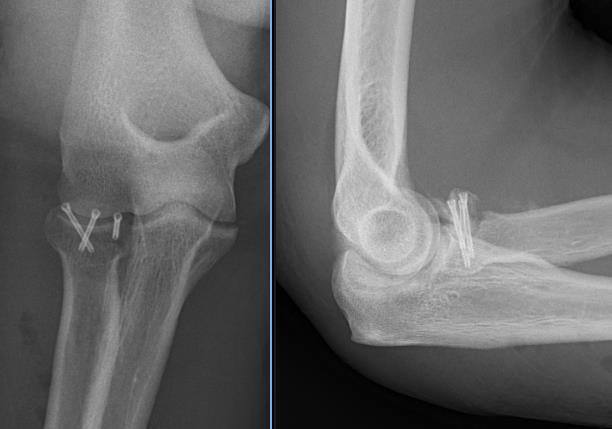
Radial head fragment nonunion
Results
Outcomes
- 56 patients with ORIF radial head
- 30 Mason 2, 26 Mason 3
- 13/14 patients with comminuted Mason 3 with > 3 fragments had poor outcome
- 15/15 patients with simple Mason 2 had good outcomes
- best results with 3 or fewer fragments
Arthroscopic versus open ORIF radial head
- systematic review of arthroscopic versus open ORIF radial head
- reduced stiffness and HO with arthroscopic fixation
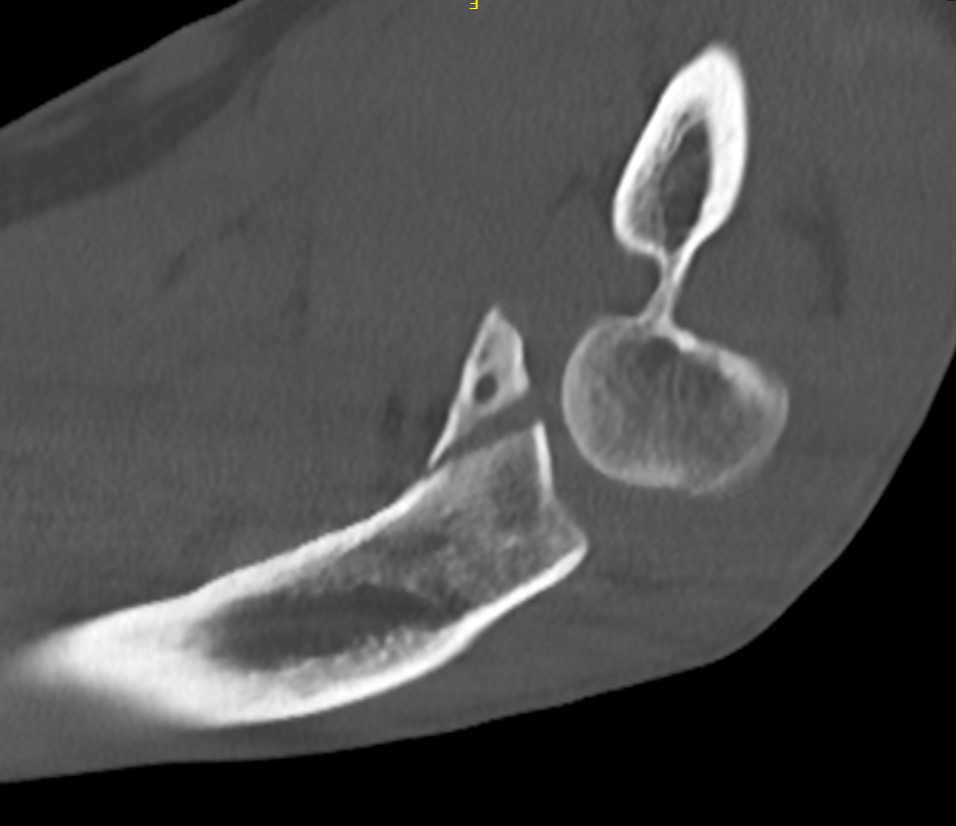
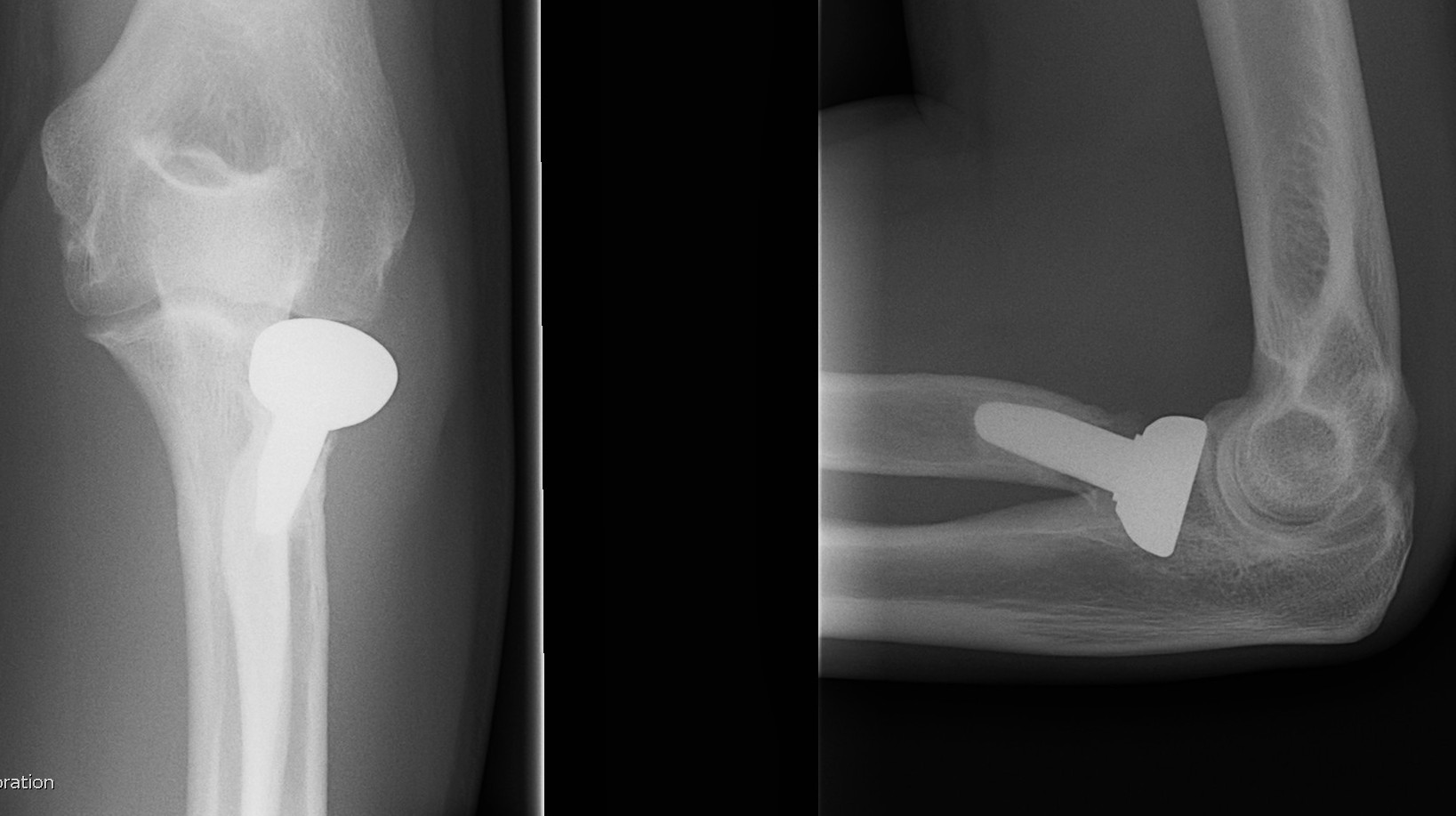
Radial Head Arthroplasty (RHA)
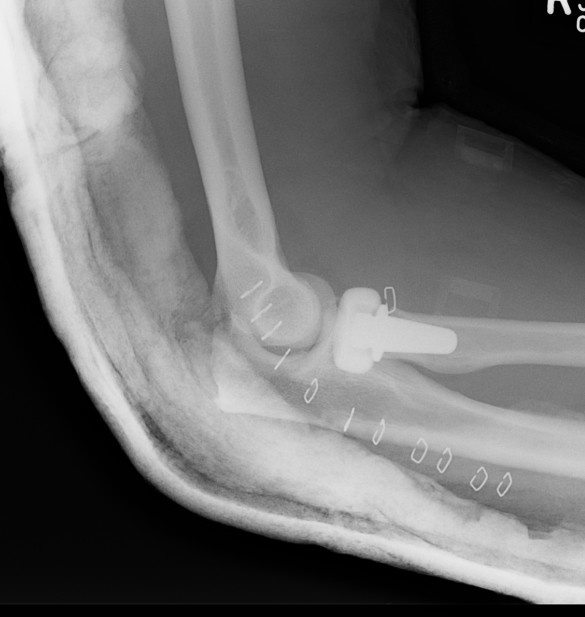
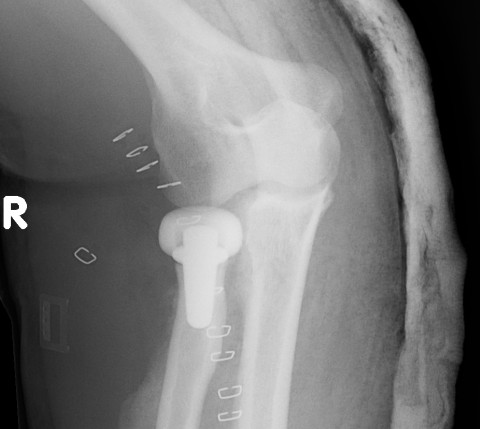
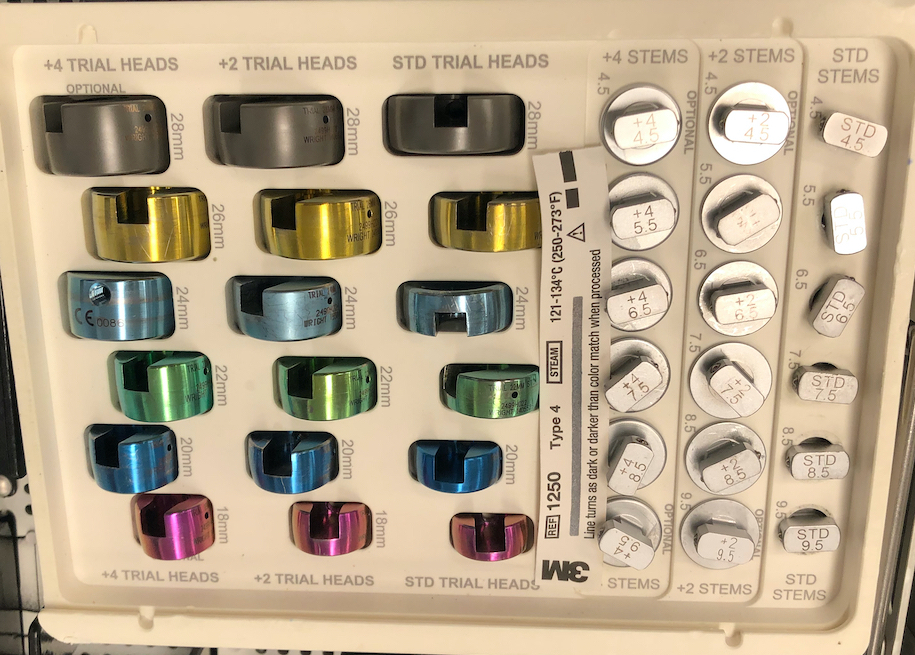
Design
Cobalt chrome / pyrocarbon / titanium
Modular - various head diameter / thickness + various stem sizes + collars to build up radial neck if required
Fixation - press fit v loose fit
Technique Modular Titanium Radial Head Arthroplasty
AO Surgery Reference Radial head arthroplasty
Vumedi Evolve Radial Head arthroplasty

Lateral approach to elbow / Kaplans or Kocher
- open capsule
- divide annular ligaments
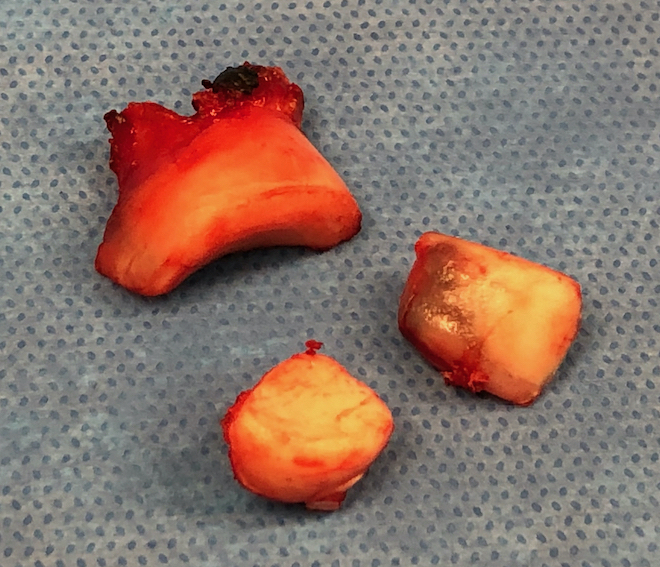
- excise radial head fragments
- use fragments to estimate diameter and thickness of radial head
- if in doubt, downsize
- deliver radial neck
- do not place Hohman retractor anteriorly to protect PIN
- ensure neck cut flat to avoid maltracking
- want 60% contact of radial neck with prosthesis
- insert trial broaches into neck
- insert trial head diameter and neck length
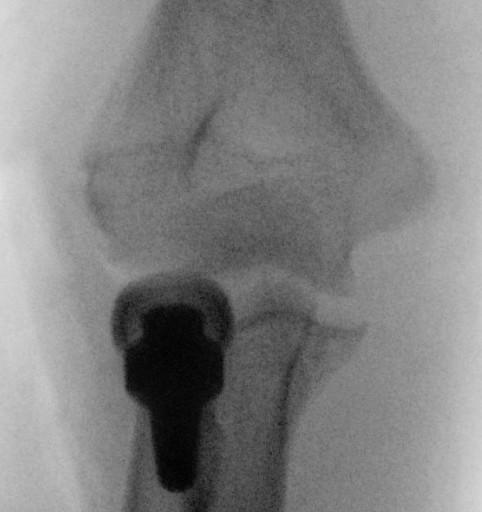
- check no overstuffing on xray
- insert prosthesis
- repair annular ligament
- inspect +/- repair LCL
Overstuffing
| Lesser sigmoid notch | Symmetry of ulnohumeral joint |
|---|---|
|
Radial head shoulder articulate with lesser notch
|
Ensure no gapping of lateral ulnohumeral joint |
 |
 |
 |
 |
- cadaveric study
- increased medial ulno-humeral joint line gapping with overlengthening of 6 or 8 mm
- increased lateral ulno-humeral joint line gapping with overlengthening of 2 mm
Results
- systematic review of radial head arthroplasty
- 30 articles with 727 patients
- 8% revision rate
- Mayo Elbow Performance Score: 85% good or excellent
- no evidence of superiority of bipolar / monopolar / fixation technique
- systematic review of minimum 8 year outcomes of RHA
- 10 studies with 432 elbows
- 86% minimal or no pain
- 9% loosening
- 27% degenerative change
- 3% RHA revision rate
- 15% removal of implants
Complications
Stiffness
Over lengthening / over stuffing
Heterotopic ossification
Pain - malposition / loosening / infection / radiocapitellar OA
Instability - associated Coronoid / LCL / MCL injuries

Heterotopic ossification
Radial arthroplasty malposition


Infection
Radial Head Resection
Indication
Elderly patient
Coronoid intact
Contra-indication
Elbow dislocation
LCL / MCL / Interosseous membrane disrupted
Complications
Proximal radius migration
DRUJ instability and pain
Valgus instability elbow
Arthritis (deceased SA, increased contact stresses)
Results
- 26 patients < 40 treated with radial head resection
- minimum 15 year follow up
- 81% no elbow pain
- good or excellent results 92%
- all had xray evidence of arthritic change
- increased valgus / carrying angle in all
