

Definition
Tibial spine avulsion at the bony insertion of the ACL on the tibia
- ACL intact
Anatomy
Bony fragment
- ACL tibial insertion attached
- anterior horn of lateral meniscus often attached
The intermeniscal ligament is a block to reduction
Aetiology
Children aged 8 - 14
Tibial eminence ossification is weaker than ACL at this age
Knee hyperextension +/- valgus
Clinical
Swollen knee with haemarthrosis
Lack of full extension due to a mechanical block
Meyers & McKeever classification
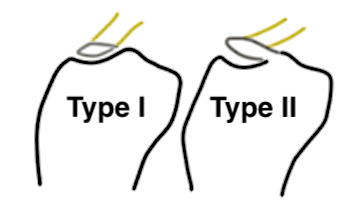
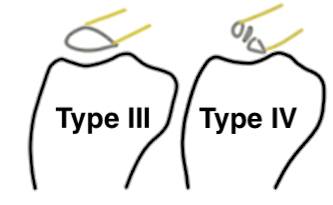
Type I: Undisplaced
Type II: Partially displaced with anterior portion hinged
Type III: Completely Displaced
Zaricznyj Type IV: Comminuted
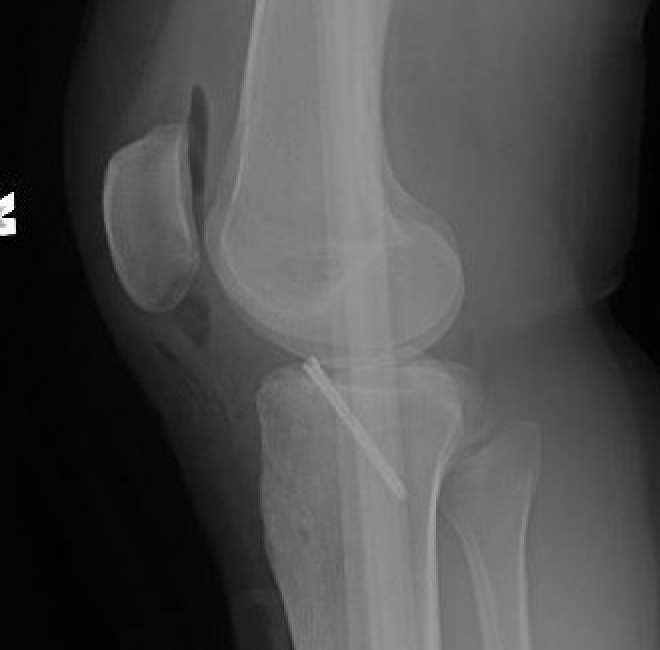
Xray


Xray showing likely Type II with anterior hinging

Type II / III
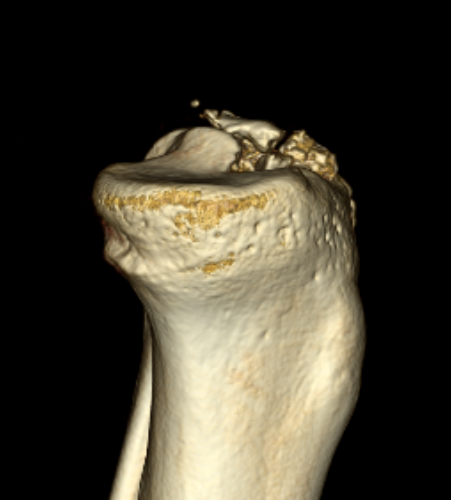
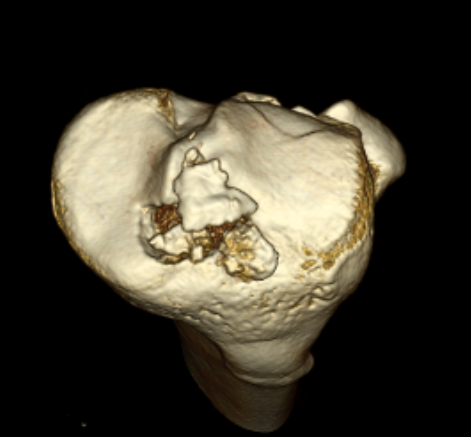
CT
Can help classify and thus guide treatment

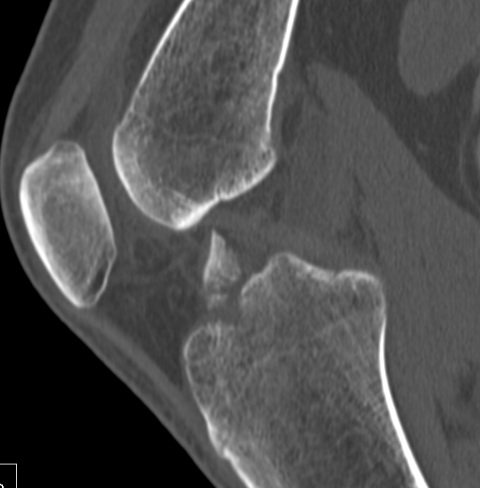
Type II Type III


Type IV
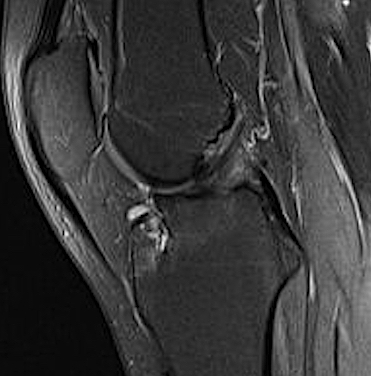
MRI
Rhodes et al J Paediatr Orthop 2018
- 77 patients with ACL tibial avulsion
- meniscal entrapment identified in 40%
- 30% meniscal tear, 70% osteochondral injury
- 32% other ligament injury

Sagittal MRI demonstrating small bony fragment with ACL attached
Nonoperative treatment
Indication
Type I - 6 weeks cast / splint in extension
Type II - attempt closed reduction
Closed reduction and casting
Indication
Type II
Technique
Attempt closed reduction
- anaesthesia / image control
- long leg cast in full extension
- trap fragment under condyles
Block to reduction
- usually intermeniscal ligament
- can be medial or lateral meniscus

Xray demonstrating reduction of fragment with knee in hyperextension and in cast
Operative Management
Indications
Type II that doesn't reduce / blocked by intermeniscal ligament
Type III
Type IV
Options
Open / medial arthrotomy
Arthroscopic repair
Fixation Techniques
1. Physeal sparing screw
Image guided
- directed posterior and obliquely
Advantage
- strong fixation
- may be able to range knee earlier
Disadvantage
- not indicated in comminuted fractures / Type IV
- second surgery to remove screw
- iatrogenic risk to posterior NV structures
2. Suture fixation
Advantage
- comminuted fractures
Disadvantage
- technically challenging
- may tether physis if transphyseal
Techniques
A. All epiphyseal if > 4 years of growth
B. Trans-physeal if < 4 years of growth
Tie over bony bridge or use cortical buttons
Open fixation
Technique
Medial parapatellar arthrotomy
- need to remove portion of fat pad for visualisation
- intermeniscal ligament may block reduction
- remove callus / hematoma
- replace fragment under intermeniscal ligament
- want to impact fragment to tension stretched ACL
- insert screw

Arthroscopic suture fixation
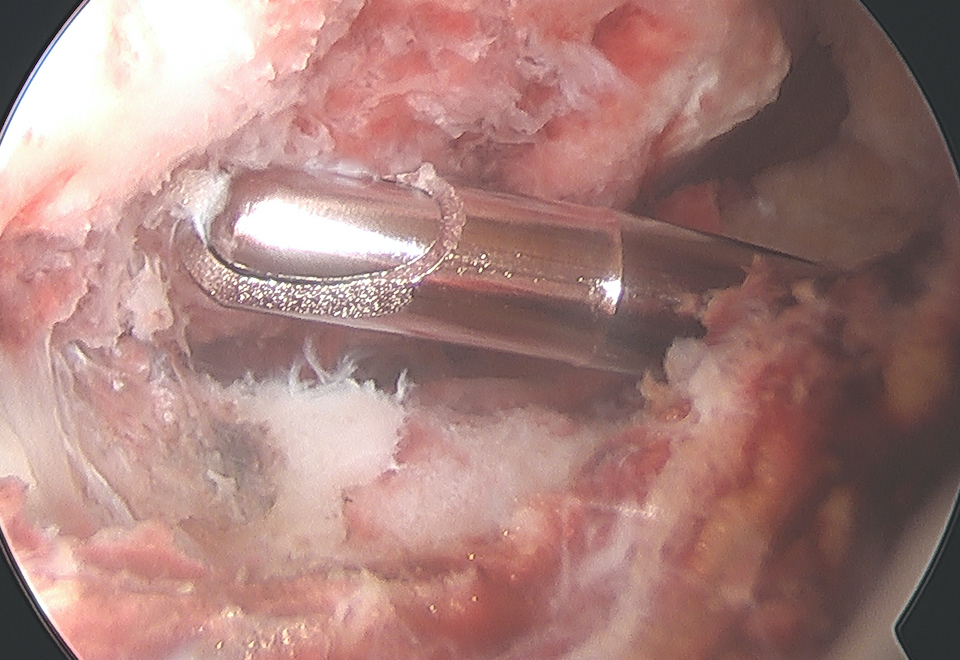
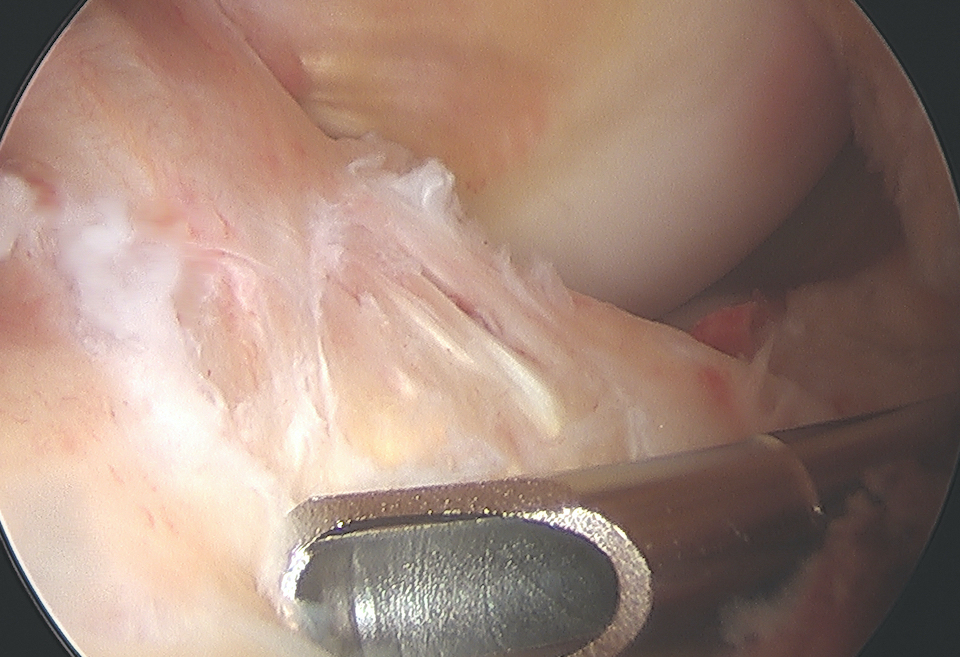

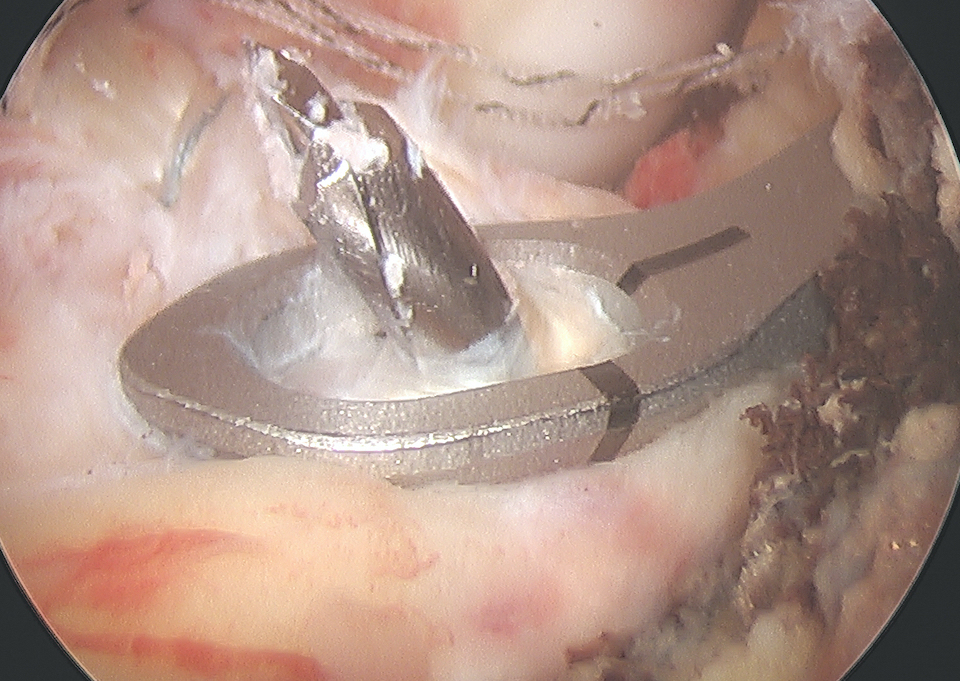
Fragment flipped and insertion debrided Avulsion fragment reduction Passage of two loop sutures with scorpion
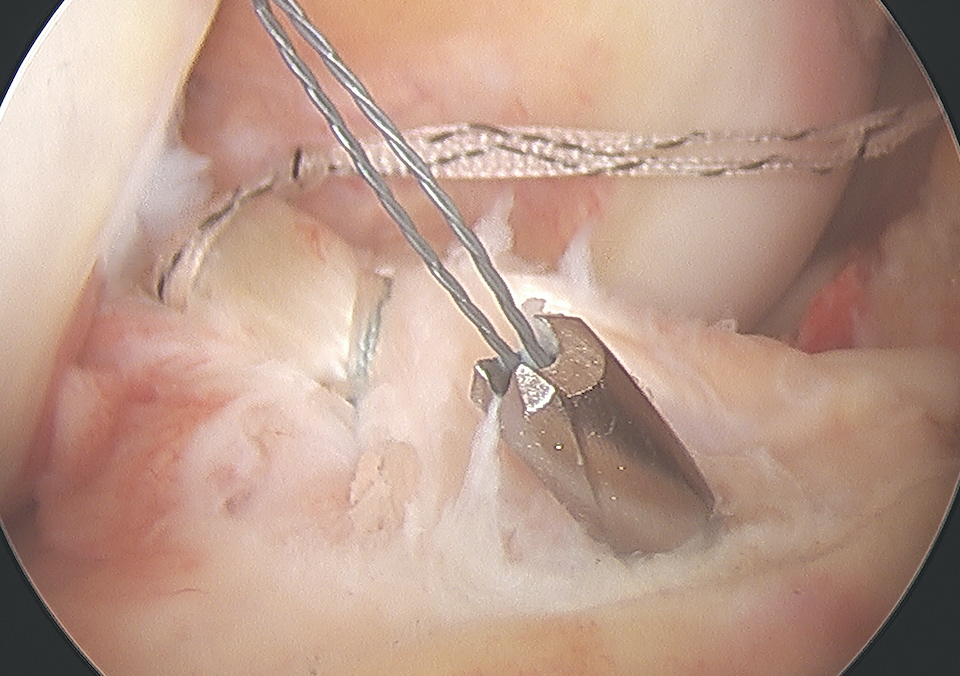
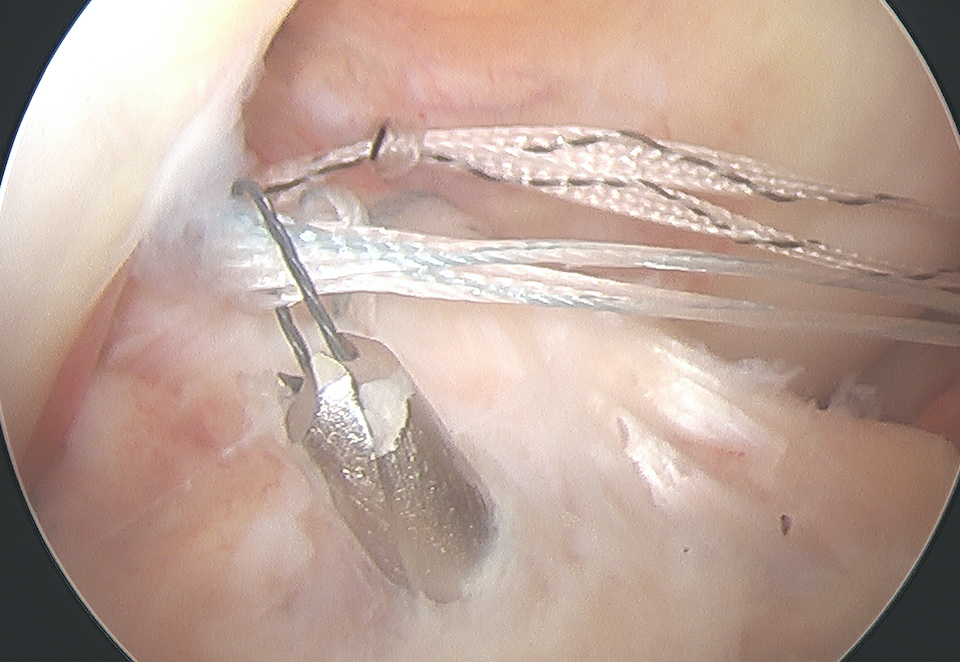
ACL tibial jib with beath pin Beath pin cannulated, loop wire passed Retrieval of sutures
Technique
Clean haematoma, ensure can reduce fragment with probe
- can consider temporary fixation with K wire
- arthroscopic suture passer (i.e. arthrex knee scorpion)
- pass sutures x 2 through ACL above bony fragment
- cannulas can be useful for suture management
Reduce fragment and hold with ACL tibial guide
- medial tibial incision, pass beath pins x 2 (preferable cannulated)
- 1 cm between tunnels
- beath pins exit through bony fragment
- retrieve sutures
- reduced fragment, knee in full extension
- tie over bony bridge or over cortical button
Technical note
1. Passing sutures anterior to the bony fragment rather than through may help anatomical reduction
2. Companies make cannulated beath pins, allowing suture loops to be passed up the pins
Post operative
- TWB for 4 - 6 weeks
- 0-90 degrees for 4 - 6 weeks


Suture bridge surgical technique video
Arthroscopic cortical button physeal sparing


Outcomes / Complications
Operative v Non operative
Likely that surgery limits ongoing instability
Gans et al Am J Sports Med 2014
- systematic review of 580 pediatric and adolescent patients
- no difference in outcomes between open and arthroscopic techniques
- no difference in outcomes between screw and suture fixation techniques
- reduced laxity and stiffness after surgical treatment of Type I and II fractures
Stability
Residual instability common despite surgery due to ACL stretching before injury
- 6 patients average age 12 two years after arthroscopic fixation
- abnormal Lachmans in 5/6
- abnormal pivot shift in 2/6
- all had excellent functional outcomes
Quinlan et al Arthros Sports Med Rehab 2021
- 66 patients average age 11 with mean follow up 6 years
- surgical fixation of Type II and III
- 92% reported knee as normal
- 9% limited by instability and pain
- 7% subsequent ACL rupture
Stiffness
Stiffness can be a problem in the surgical group
- a combination of surgery and prolonged immobilization
Edmonds et al J Paediatr Orthop 2015
- 57 surgical patients, 19 treated with casting
- mean age of 12
- arthrofibrosis 12% in surgical group, 0% in casting
- casting group 17% incidence second surgery for instability / loose bodies / impingement
Nonunion
Rare
Typically in setting of nonoperative treatment of completely displaced fractures (Type III)
Malunion
Nonoperative treatment
- anterior fragment remains displaced
- may cause impingement and loss of extension
- may be associated with residual laxity

Xray and MRI demonstrating residual anterior elevation of fragment causing impingement
Growth plate disturbance
Associated with transphyseal drilling with > 4 years growth remaining
