Definition
Primary malignancy arising from remnants of the notochord
Epidemiology
Rare malignant tumour
Middle-aged adults (50-70)
M>F
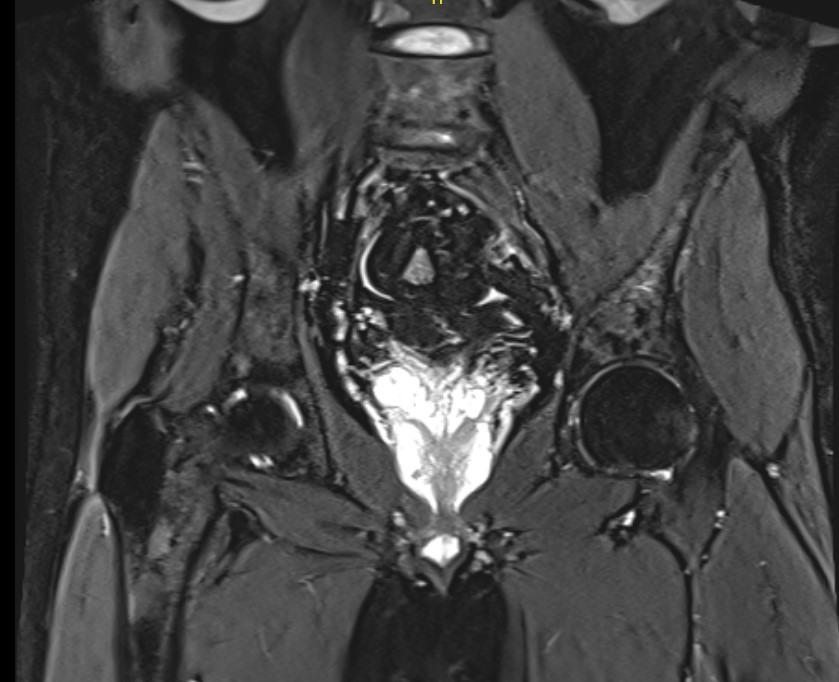
Location
In midline in axial skeleton
Base of skull 35%
Vertebrae 15%
- especially cervical
Sacrum 50%
Clinical
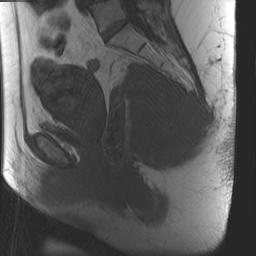
Sacral Tumour
Usually presents late (long History LBP)
- slow-growing
- large potential space to expand into
- often very large on presentation
Perineal pain
Bladder & bowel dysfunction
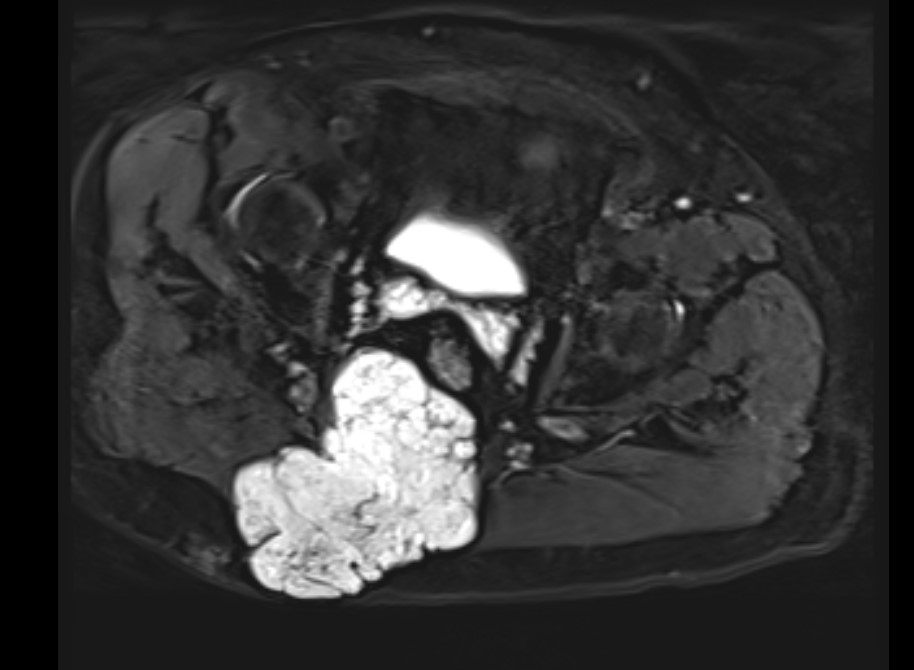
Mass effect
Neurological compression
Usually can feel rectal mass ~ 50%
X-ray

Bony destruction is hallmark + soft tissue mass
- 50% Calcification within mass
Sacrum
- irregular areas of bone destruction
- sacral expansion
- soft tissue mass
CT Scan / MRI
Useful to delineate tumour
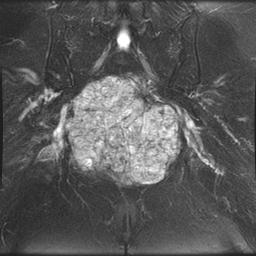
Pathology
Gross
- lobulated bluish / gray
- extensive gelatinous translucent areas which are focally cystic & haemorrhagic
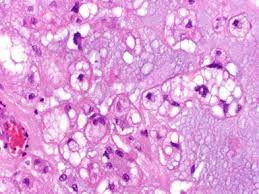
Histology
- lobular framework of Physaliphorous cells
- cells have bubbly pink cytoplasm & Bulls-Eye nucleus
- vascular fibrous septa
- mucinous matrix
- 1/3 significant Chondroid production (can be mistaken for chondrosarcoma)
DDx
GCT / ABC
Chondrosarcoma / OS / Ewing's / Myeloma
Metastasis
Management
Operative
Most important predictor of survival is clear surgical margin
- usually difficult due to location
Sacral Surgery
- leave at least 1 S3 - 100% continent
- leave at least 1 S2 - 50% continent
- above S2 incontinent because pelvic splanchnics removed
Radiotherapy
Indications
- resection not possible
- positive margins
Rarely effective
Prognosis
Metastasis 30-50%
- pulmonary mets may occur (late)
Death usually 2° local infiltration
