Epidemiology
Usually young patients
- 15 - 40
15% compound
Aetiology
High velocity injury
- MBA
- MVA
- pedestrian v car
- fall from height
Emergency Managment
EMST principles
- need for transfusion not uncommon
- hypotension from isolated closed femoral fracture unlikely
Beware
- ipsilateral NOF / pelvic fracture / acetabular fracture
- knee injury / ACL or other ligament injury
- floating knee / ipsilateral tibial fracture
Thorough neurovascular exam
- incidence vascular injury 1%
Thomas splint
- ring against ischium
- velcro around foot
- pneumatic traction
- can only be applied for 12 hours or so


Carbon traction splints

Balanced Traction

Compound wound

Betadine pack
Tetanus
Antibiotics
Winquist Classification
Type 1
- minimal or no comminution

Type 2
- < 50% comminution

Type 3
- 50 - 100% comminution
- inherently unstable
- needs distal locking

Type 4
- segmental comminution
- no contact or inherent stability
Associated injuries
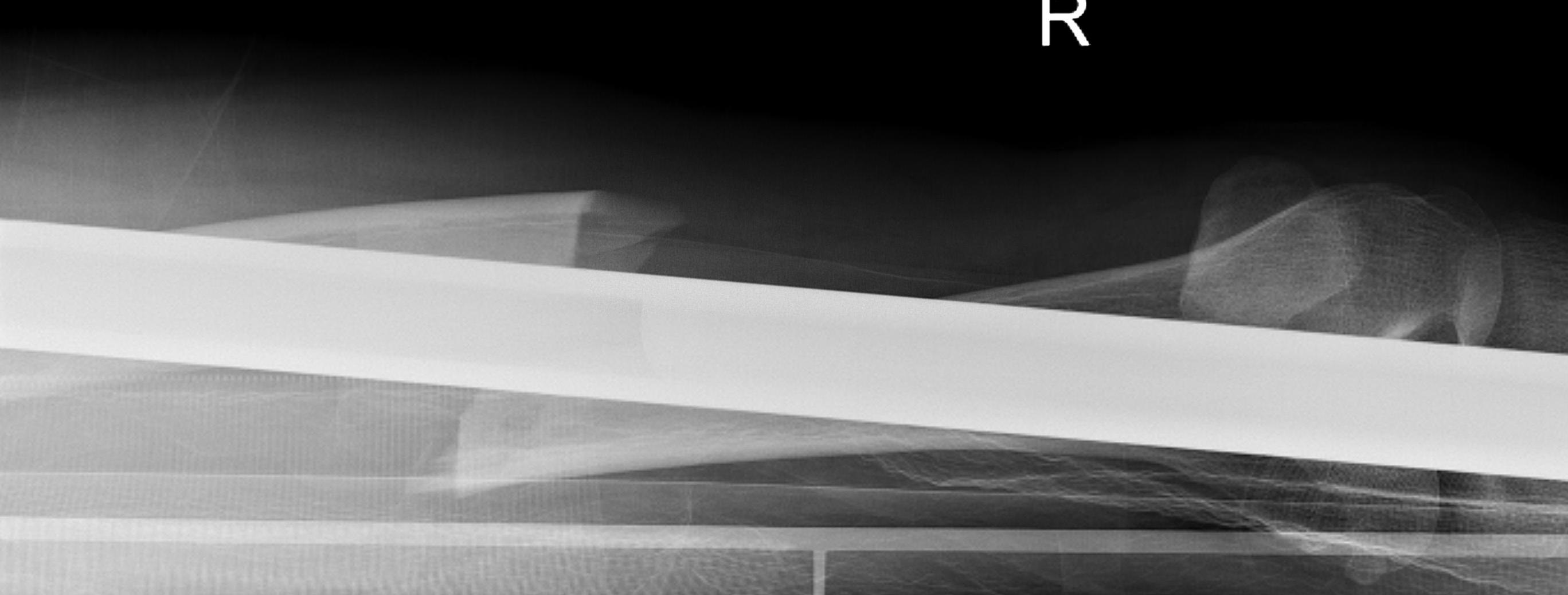
Femoral Shaft Fracture with Neck Fracture
Up to 10% concurrence
- can be missed on plan film
- splints can obscure
Assessment
- carefully review pelvic xrays
- order CT if required
- assess carefully using fluoroscopy during surgery
Knee
Byon et al. Injury 2018
- 87 knee ligament injuries in 429 femoral shaft fractures (20%)
- 20 PCL, 11 ACL, 16 MCL, 8 LCL and 32 multiligament knee injuries
- always assess knee after femoral stabilisation
https://pubmed.ncbi.nlm.nih.gov/29887503/

Floating Knee
Ipsilateral femur + tibial fracture


Operative Management Issues
Surgical Timing
Early fixation < 24 hours
- indicated for isolated injuries
- reduce risk of pulmonary complications
Harvin et al. J Trauma Acute Care Surg 2012
- compared early stabilisation (<24 hrs) with delayed (>24 hrs)
- retrospective review of 1,376 patients
- early IMN associated with decreased pulmonary complications such as pneumonia / PE / ARDS
- decreased length hospital stay
https://pubmed.ncbi.nlm.nih.gov/23188236/
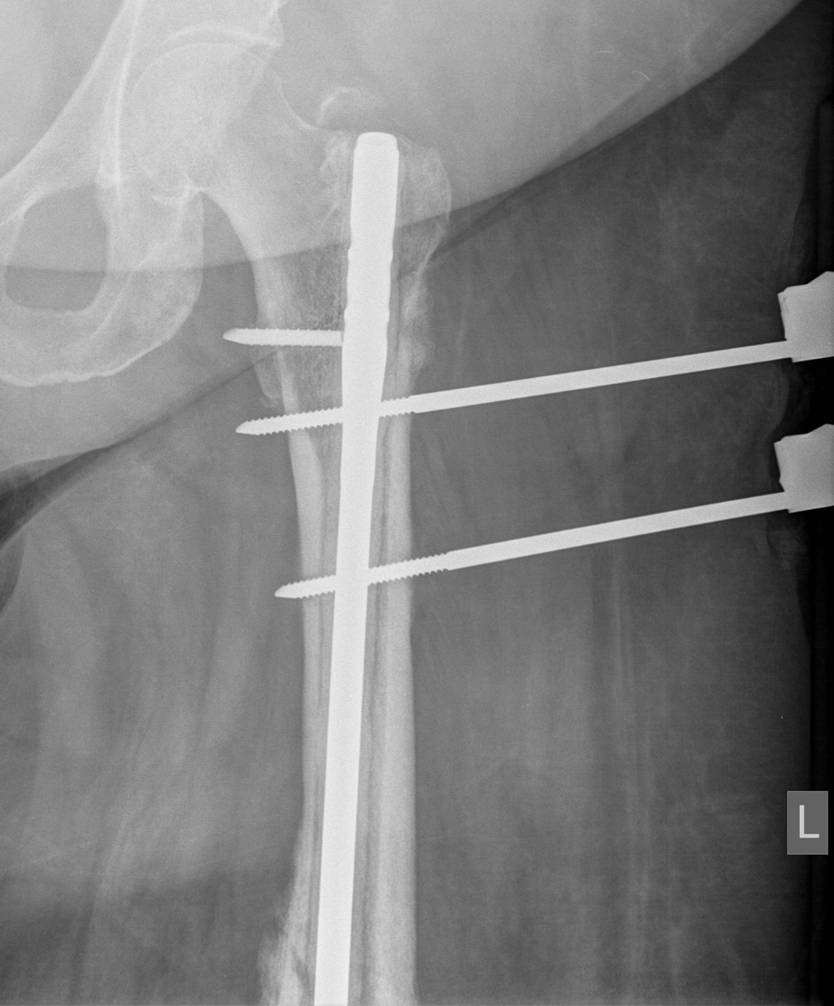
Damage Control Orthopaedics
Concept
- severely injured polytrauma patients
- head / chest / abdominal / pelvic injuries
- patients have elevated cytokines (IL-6) in multitrauma
- avoid second hit of surgery during this period
- second hit may be associated with ARDS and multi-organ failure
Technique
- stabilise femoral fracture with simple external fixator
- allow return to ICU for warming / stabilisation
- delay definitive treatment until inflammatory state reduces
- approximately day 6
Results
Pape et al J Orthop Trauma 2002
- retrospective study of polytrauma patients at risk of multi-organ failure
- patients treated with early IMN femur v DCO (early stabilisation femur external fixation with later IMN)
- significant reduction in incidence of multiorgan failure
- significant reduction ARDS (15% down to 9%)
- no increased rate of local complications (infection, non union)
https://pubmed.ncbi.nlm.nih.gov/12352480/
Surgical Options
1. External fixation
2. IMN
3. Plate
1. External Fixation
Indications
- severely contaminated wound
- Damage Control Orthopaedics
- complex femoral fracture with vascular injury
AO Surgery Technique
- safe zone is lateral
Timing of conversion to IMN
Harwood et al J Orthop Trauma 2006
- two groups
- 81 patients treated with early IMN
- 111 patients treated with external fixation converted to IMN at mean of two weeks
- at time of surgery, pin sites excised, washed, and overdrilled
- no difference in deep infection rates between two groups
https://pubmed.ncbi.nlm.nih.gov/16648699/
2. Antegrade Femoral Nail


Reamed v Unreamed IMN
Nonunion rates
Canadian Orthopaedic Trauma Society (COTS) JBJS Am 2003
- multicentred randomised trial
- non union rates reamed v unreamed IMN
- 8 / 107 (7.5%) smaller unreamed femoral nail nonunion
- 2 / 121 (1.7%) larger reamed femoral nail nonunion
https://pubmed.ncbi.nlm.nih.gov/14630836/
Li et al. Medicine 2016
- meta-analysis of 8 RCT and 1078 patients
- reamed nails had shorter times to union
- reamed nails had reduced rates of nonunion and reoperation
- no increased rates of ARDS, mortality or blood loss with reaming
https://pubmed.ncbi.nlm.nih.gov/27442651/
ARDS
Canadian Orthopaedic Trauma Society (COTS) J Orthop Trauma 2006
- multicentred randomised trial reamed v unreamed
- incidence ARDS in multiply injured patients
- 3/63 reamed v 2/46 unreamed developed ARDS
- very low incidence of ARDS in both groups
- not statistically significant
https://pubmed.ncbi.nlm.nih.gov/16825962/
Trochanteric v Piriformis Entry Point
Kumar et al. Injury 2019
- systematic review of 9 studies
- trochanteric entry reduced OR time, fluoroscopy time, reduced abductor weakness, better functional outcome
- similar union rates
https://pubmed.ncbi.nlm.nih.gov/31358301/
3. Femoral Plate
Indications
- associated proximal / distal femoral fracture
- vascular injury
- medulla too narrow for IMN
- paediatric population
- treatment of non union
Issues
- tension side / load bearing
- significant disruption to blood supply required
- plate will break early if union not achieved
Technique
- large fragment plate
- minimum 8 cortices each side of fracture
- need periord of NWB
Results
Giessler et al Orthopedics 1995
- 71 femurs diaphyseal fractures
- 93% union at 16 weeks
- recommended bone grafting at same time
https://pubmed.ncbi.nlm.nih.gov/7479404/
Difficult Scenarios
1. Floating Knee
Single incision at knee
- retrograde femoral nail
- tibial IMN if appropriate
High complication rates including non union / malunion, knee stiffness and hetertopic ossification
https://pubmed.ncbi.nlm.nih.gov/30910244/
https://pubmed.ncbi.nlm.nih.gov/29885963/



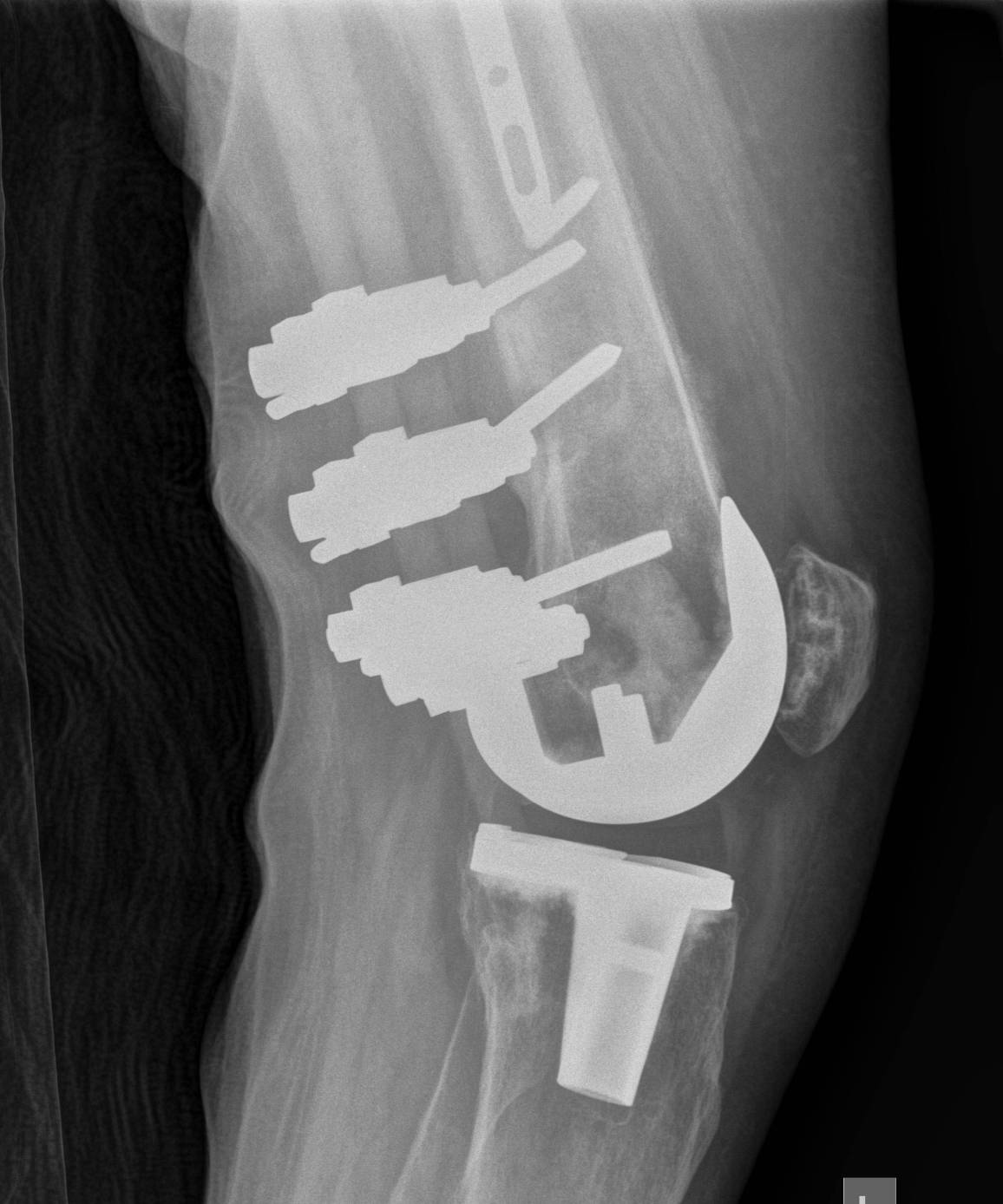
2. NOF (Neck of Femur) + Femoral shaft fracture
Must pay attention first to meticulous NOF ORIF
Options
1. Pin and Plate NOF / Retrograde Nail
2. Pin and Plate NOF / Plate femur
3. Reconstruction Nail
- difficult to anatomically reduce NOF
- increased incidence NOF non union
Difficult scenario
- antegrade IMN in place before diagnosis of NOF fracture
- if undisplaced, can place screws anterior to nail
- if displaced must remove nail
Results
Ostrum et al. CORR 2014
- 95 cases treated with proximal screws / sliding hip screws inserted first
- retrograde IMN second
- 98% union rate femoral neck
- 91% union rate femoral shaft
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4117883/pdf/11999_2013_Article_3271.pdf
Vumedi video
3. Dislocated Hip + Femoral shaft fracture
1. Simple dislocation
- may be able to reduce hip with proximal steinman pin
- then IMN femur / retrograde or antegrade
- or plate femur
2. Dislocation with Pipkin fracture
- may need anterior approach to ORIF femoral head fracture
- may be best to plate / retrograde nail femur
3. Dislocation with posterior acetabular fracture
- may need posterior approach to acetabulum
- consider plating femur / distal femoral or tibial steinman pin
- delayed ORIF posterior wall
4. Distal femoral condylar fracture + shaft fracture
Options
1. Screws anterior and posterior to retrograde nail
2. Distal Locking plate
5. Bilateral Femur Fractures
Lane et al. Orthopedics 2015
- 72 patients
- high rate of complications
- mortality rate 6.9%
- increased risk of DVT and pulmonary complications
https://pubmed.ncbi.nlm.nih.gov/26186320/
Stavlas et al. Injury 2009
- systematic review 197 patients
- treated with bilateral reamed IMN
- fat embolism 4.1%
- ARDS 14%
- PE 7%
- suggest damage control orthopaedics
https://pubmed.ncbi.nlm.nih.gov/19775688/
6. Segmental bone defects / critical bone defects
Management
- temporary fixation with nail / plate / ext fix
- cement spacer
- delayed Masquelet technique / induced membrane technique at 6 - 8 weeks
Morwood et al. J Orthop Trauma 2019
- 65 femurs with critical bone loss
- increased union, time to weight bearing with IMN v plate
- fewer grafting procedures and reoperations with IMN
https://pubmed.ncbi.nlm.nih.gov/31403558/
Trochanteric Entry Antegrade Femoral Nail Surgical Technique
Vumedi Video
https://www.vumedi.com/video/pearls-femoral-im-nailing/
Smith and Nephew Trigen TAN FAN
https://www.smith-nephew.com/global/assets/pdf/products/surgical/trigen_tan_fan.pdf
Position
- GA, IV ABx, transexamic acid
- traction table
- patient legs adducted, torso adducted
- allows access to GT
- flex and abduct other hip for image intensifier / fluoroscopy access
Entry
- incision proximal to GT
- split abductors in line
- palpate tip of GT
- check entry point on AP xray view
- check entry point on lateral xray view (junction anterior 1/3 posterior 2/3)
- entry with awl or 3.2 mm guide wire
- ensure wire doesn't penetrate medial cortex
- use proximal reamer for thickened proximal portion of nail
Pass guide wire
- ball tipped
- femoral fractures difficult to reduce with traction
- use reduction tool to reduce in AP and lateral views to pass guidewire
- if having difficulty +++, can perform miniopen incision to pass guide wire
- measure guide wire to determine nail length
Note typical deformity of proximal fragment which needs to be corrected
- flexed by psoas
- abducted by G medius
- externally rotated
Ream
- tight fit best
- nails come in 8.5, 10, 11 and 12 mm
- need to ream 1 - 2 mm larger than nail
Pass nail
- attach to proximal locking jig
- ensure drill passes through jig into proximal nail holes
- insert nail
- visualise with flurosocopy at fracture site
- ensure nail doesn't get caught on one cortex
- excessive hammering in this position can cause fracture
Locking
Proximal
- usually proximal locking first
- screw should purchase cortex of lesser trochanter


Distal
- straighten out other leg / lower so can obtain lateral II
- perfect circle technique
- distal locking performed


Rehabilitation
Arazi et al. J Trauma 2001
- 24 patients with comminuted femoral fractures allowed to weight bear in first 2 weeks
- all full weight bearing without aids by second month
- 100% union
- 2 slightly bent locking screws
https://pubmed.ncbi.nlm.nih.gov/11303169/
Complications of Femoral Nail
Nerve Palsy
Kao et al. 1993 J Orthop Trauma
- 15% incidence pudenal nerve palsy
- usually transient
- related to longer traction times
https://pubmed.ncbi.nlm.nih.gov/8433201/
Malrotation
Incidence
Unknown
> 100 may be prevalent in up to 40% of patients
Probably not relevant unless > 300
May be associated with anterior knee pain and/or hip pain
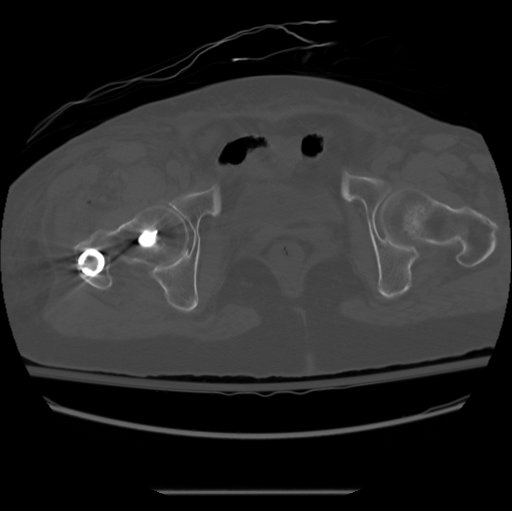
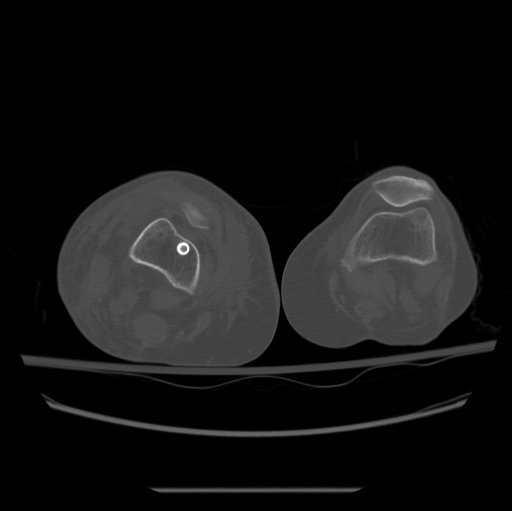
Diagnosis
A. Clinical
- difficult
- probably best to assess internal and external rotation of the hip
- when swelling goes down can assess internal and external rotation of the foot
B. CT
- axial cuts of the femoral neck and the femoral condyles
Prevention
A. Match cortices on the proximal and distal fragment
B. Both patellas pointing anterior
- match lesser trochanter position of both hips
Treatment
A. Early
- remove distal locking screws but leave in wires
- correct rotation based upon CT measurement
- insert new distal locking screws at the predetermined angle from previous screws
B. Late
- may need osteotomy
Vergano 2020 Summary article
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7944689/pdf/ACTA-91-03.pdf
Distal femoral breach
Causes
- insufficient curvature of femoral nail
- abnormal femoral curvature
- posterior starting point on the greater trochanter


Non union

Incidence
- uncommon
- 1 - 2% with reamed nails
- increased with unreamed nails
Definition
- not united (3/4 cortices) after 6 months
- no progressive union for 3 months
Options
1. Dynamisation / removal of distal locking screws
2. Exchange nailing +/- bone graft
3. Remove nail / plate + bone graft
4. Augmentation with plating and bone grafting
5. External Fixation
1. Dynamisation
Indication
- stable fractures
- non comminuted / non segmental
- evidence of fracture gapping from over traction or bone resorption
Huang et al. Injury 2012
- 39 patients
- union rate 83% when dynamisation performed 10 - 24 weeks
- union rate 33% when dynamisation performed after 24 weeks
https://pubmed.ncbi.nlm.nih.gov/22841533/
Vaughn et al. World J Orthop 2018
- systematic review of exchange nail v dynamisation
- union rate dynamisation 66%
- exchange nail union rate 85%
- dynamisation good for delayed union
- exhange nail best for nonunion
https://pubmed.ncbi.nlm.nih.gov/30079298/
2. Exchange nailing
Technique
- remove old nail
- ream up to larger size
- insert new larger nail
Swanson et al. J Orthop Trauma 2015
- 50 cases
- removal of nail, ream
- insertion of different manufacturer nail at least 2 mm bigger
- static locking
- early dynamisation if signs slow healing
- union in 100% at mean 7 months
https://pubmed.ncbi.nlm.nih.gov/24978947/
Tsang et al. Injury 2015
- risk factors for failure of exchange nail
- infection
- cigarette smoking
- may require repeat procedure
- technique eventually successful in 91%
https://pubmed.ncbi.nlm.nih.gov/26489394/
3. Removal Nail / Plating / Bone Graft
Maimaitiyiming et al. Injury 2015
- 14 patients nonunion
- bone grafting and double plating
- union in 100% at mean of 5 months
https://pubmed.ncbi.nlm.nih.gov/25712702/
4. Augment nail with Plate + Bone Graft
Medlock et al. Strategies Traumatic Limb Reconstruction 2018
- systematic review of augmentive plating v exchange nailing
- union rate 99.8% with augmentive plating
- 74% with exchange nail
https://pubmed.ncbi.nlm.nih.gov/30426320/
Infected Non union

Management
1. Open debridement
- antibiotic beads
2. Removal of nail
- ream and irrigate
- antibiotic nail / cover IMN with antibiotic cement
- IV antibiotics
- definitive nail / external fixator
Pradhan et al. Injury 2017
- infection nonunion femoral shaft 21 patients
- infection eliminated in 100%
- union in 16/21, others required further surgery to obtain union
- 2 broken nails due to noncompliance with weightbearing
https://pubmed.ncbi.nlm.nih.gov/28802424/


Refracture
No evidence increased risk if nail removed > 1 year
