Epidemiology
Young men in 20's and 30's
Aetiology
High energy injuries
- fall from heights
- MVA
Mayfield Classification
Injury progresses from radial to ulna
- usually disruption proximal row either side of lunate
1. Capitate usually displaces dorsally initially
- volar lunate dislocation is end stage
2. Volar capitate dislocations do occur
- dorsal lunate dislocation as end stage
Spontaneous reduction can also occur
Cadaver study
Stage 1 - SL dissociation
Stage 2 - CL dissociation / capitate dislocates
Stage 3 - LT dissociation
Stage 4 - Lunate dislocates
Presentation
Swollen and painful wrist
- +++ clinical suspicion
Volar lunate dislocations
- fingers semiflexed
1/3 have median nerve symptoms
Unusual to have compound wound
- usually palmar
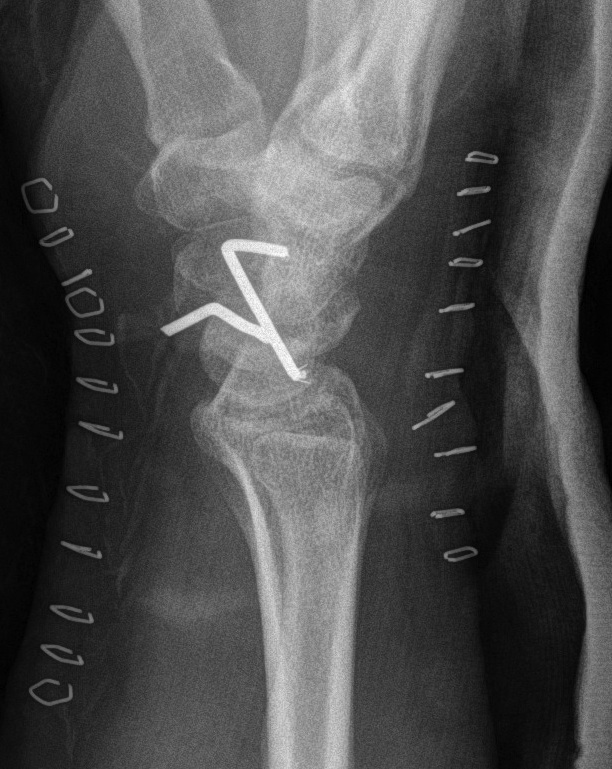
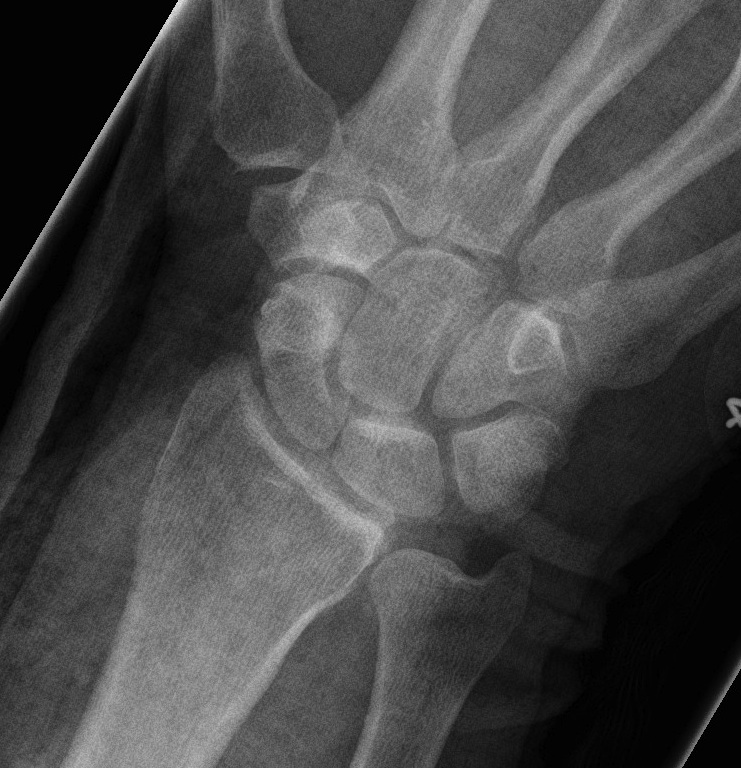
X-ray
Disruption of Gilula's 3 smooth carpal arcs
Progressive Injury
1. Capitate dorsal
- lunate remains with radius
- lunate looks triangular on AP



2. Lunate dislocates
- usually volar
2 main groups of injury
1. Dorsal trans-scaphoid dislocation
- 2/3 of cases


2. Dorsal perilunate dislocation
- 1/3 of cases
Associated Injuries
Scaphoid fracture
Radial styloid fracture
Capitate fracture
Chronic presentations
Missed in 20%
- reasonable ROM
- little pain
May present with CTS
May present with flexor tendon ruptures
Management
A. Acute perilunate dislocation
Initial Reduction
Traction under anaesthesia / conscious sedation
- dorsiflex wrist
- counterpressure on palmar lunate
- gradual wrist flexion with pressure on dorsal capitate


Definitive
Poor results with non operative management
- require anatomical repair of proximal row
- wait 3-5 days for swelling to settle
1. No scaphoid fracture
Reduce lunate
- closed reduction
- open reduction
Dorsal approach
- longitudinal incision
- 3/4 extensor compartment
- mobilise EPL laterally
- open dorsal between DRC and DIC ligaments
- joysticks in scaphoid and lunate
- reduce DISI deformity
- K wires SC / SL / LT (areas of ligament rupture)
- repair SL ligament back onto scaphoid with anchors / transosseous sutures
- ORIF any capitate fractures
- repair LT ligament + augment with capsule
+/- Volar approach
- difficulties reducing lunate
- perform CTD
- repair rent in volar capsule / Space of Poirier



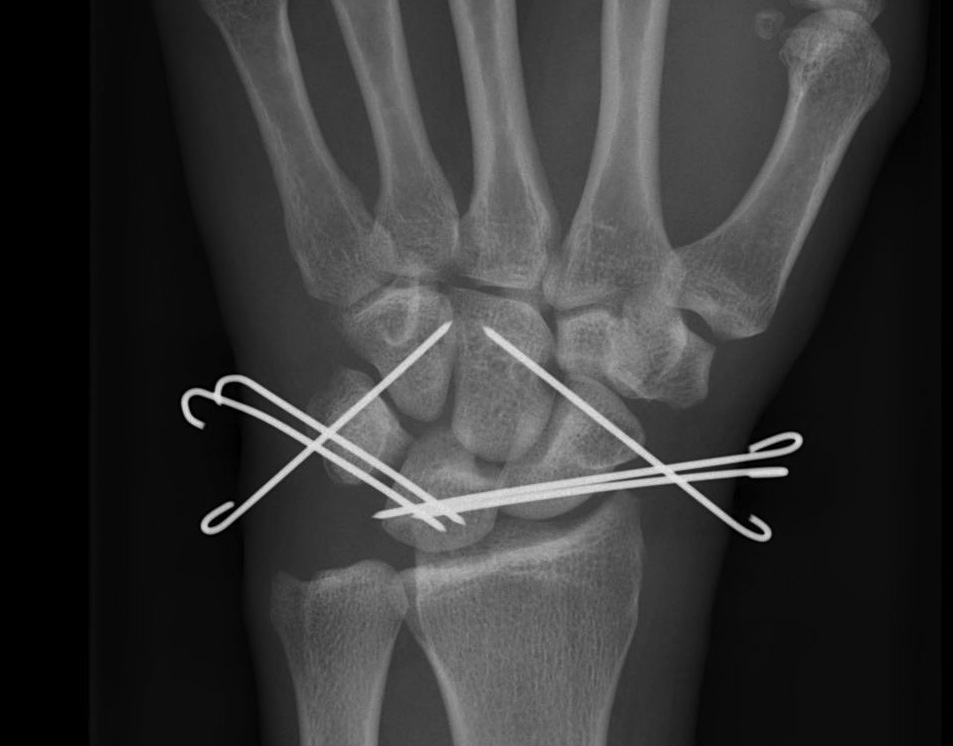

Recent trends
- add SL screw
- add Blatt capsulodesis
- repair rent in volar capsule
- make wrist as stiff as possible to prevent late OA
2. Trans Scaphoid Perilunate

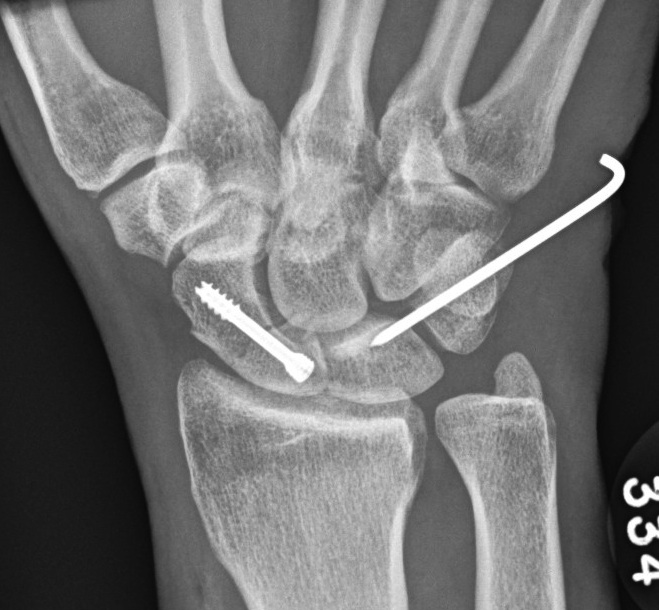
Dorsal approach
- ORIF scaphoid fracture
- repair LT ligament
- K wires LT and TC (SL ligament is intact)
- ORIF capitate
+/- Volar approach
- CTD
- repair rent in capsule
Post op
Aim is for a stable but stiff wrist
- 8 weeks in cast, then removal of K wires
- begin ROM
Results
80% strength
Reduced ROM
- usually 100o F/E
Chronic unreduced perilunate dislocations
> 6 months
Attempt open reduction
Salvage
Options
- scaphoidectomy + 4 corner fusion
- PRC
- wrist arthrodesis
