Natural History
Seigall et al. J Paediatr Orthop 2018
- instability 3% in patients < 13 years
- instability 100% in patients > 17 years
- not predictive 13-17 years
Non Operative Management
Indications
1. Open growth plates / Juvenile OCD
- > 2 years of growth remaining
- age 12 or less
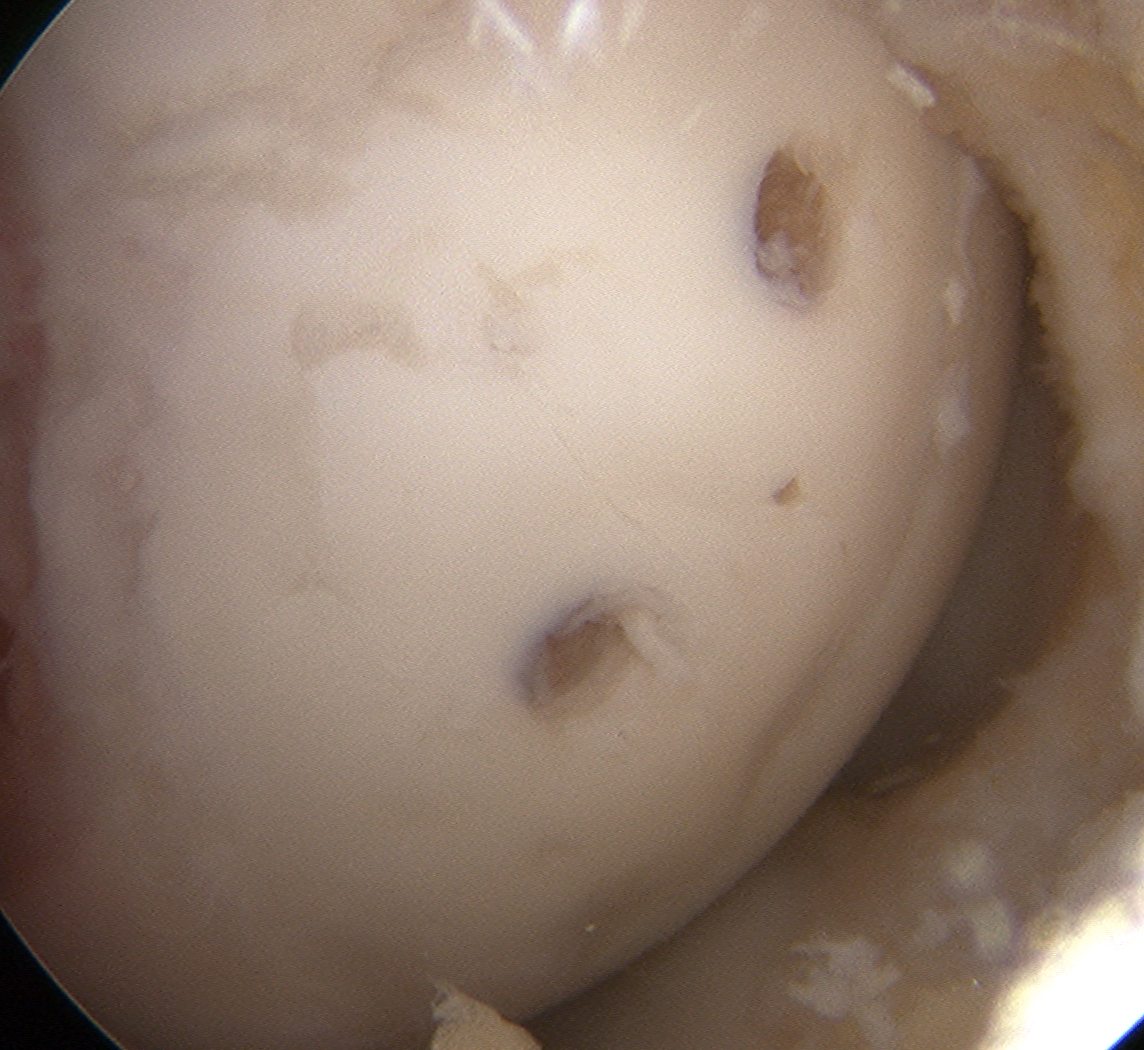
2. Stable lesion / cartilage intact / no fluid on MRI
3. Smaller lesions
Technique
No impact sports
Consider unloader brace first 3 months
After 3 months can swim or bike
Tepolt et al. J Pediatr Orthop 2020
- retrospective study of 333 stable JOCD treated nonoperatively
- treatment successful in 57% at 9 months
- unloader bracing did not improve outcomes and was more often associated with need for surgery
Assessment of healing
Xray
Signs of reossification
MRI
Reduction in size of lesion
Reduction in edema around lesion on T2
Reossification on T1
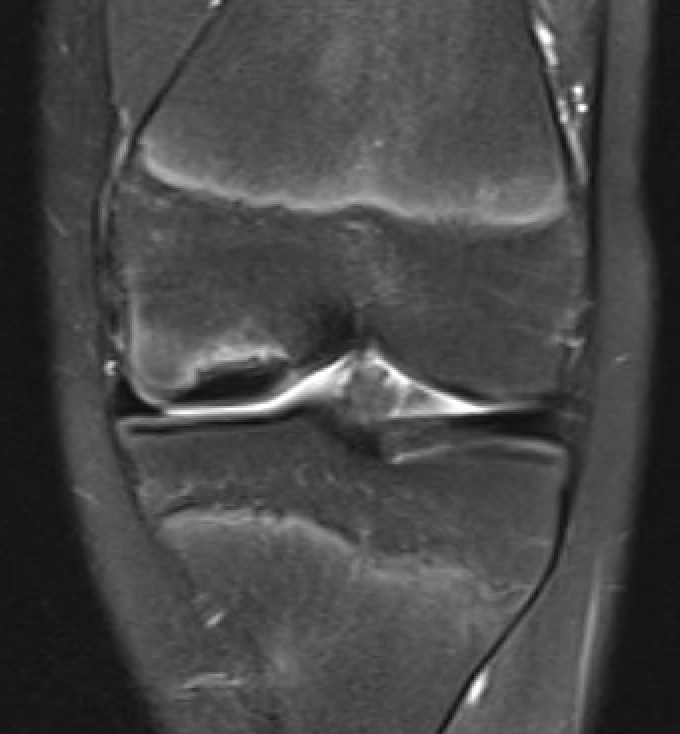

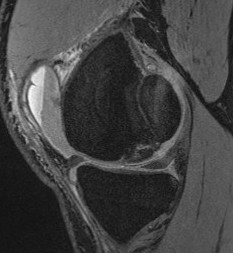
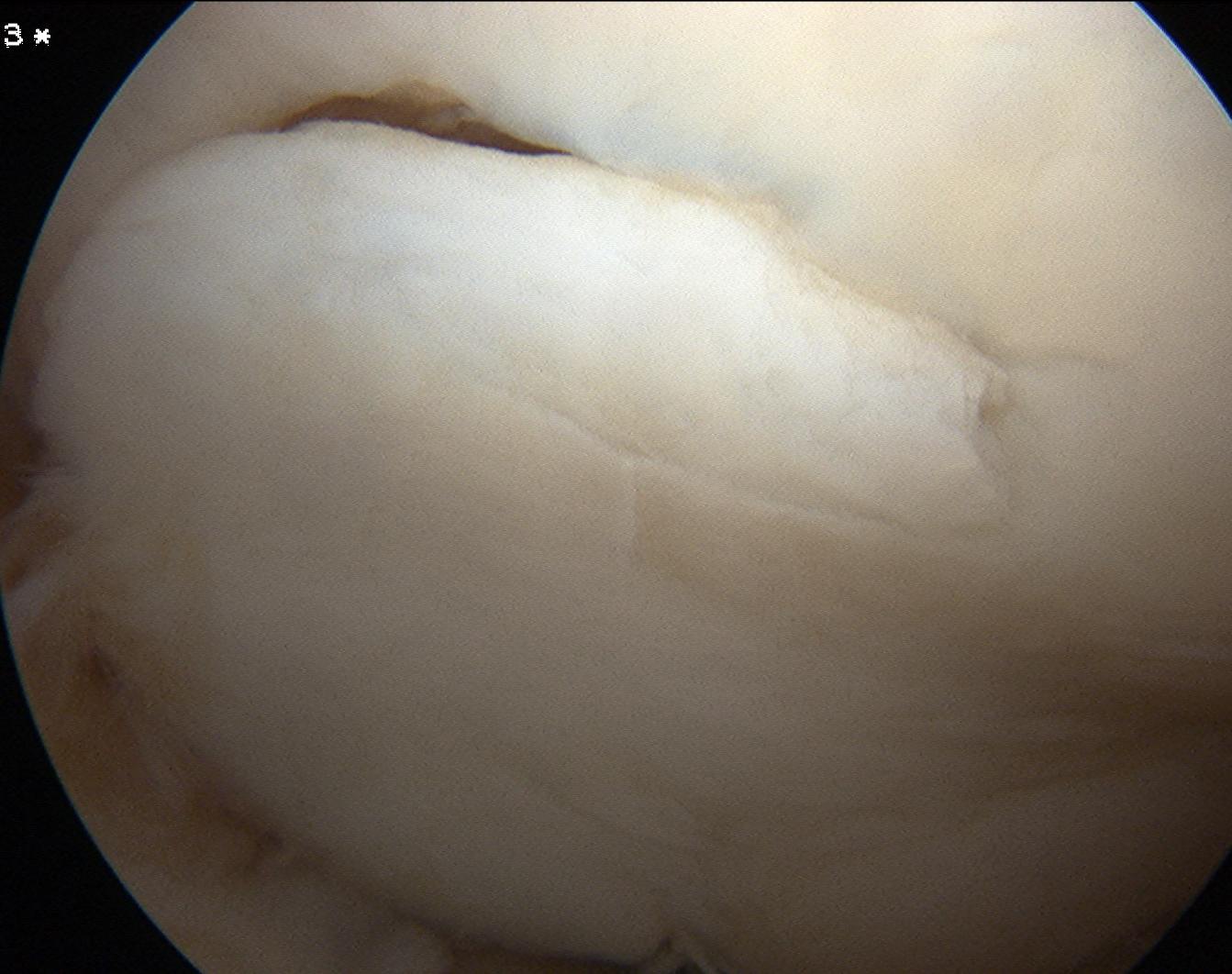
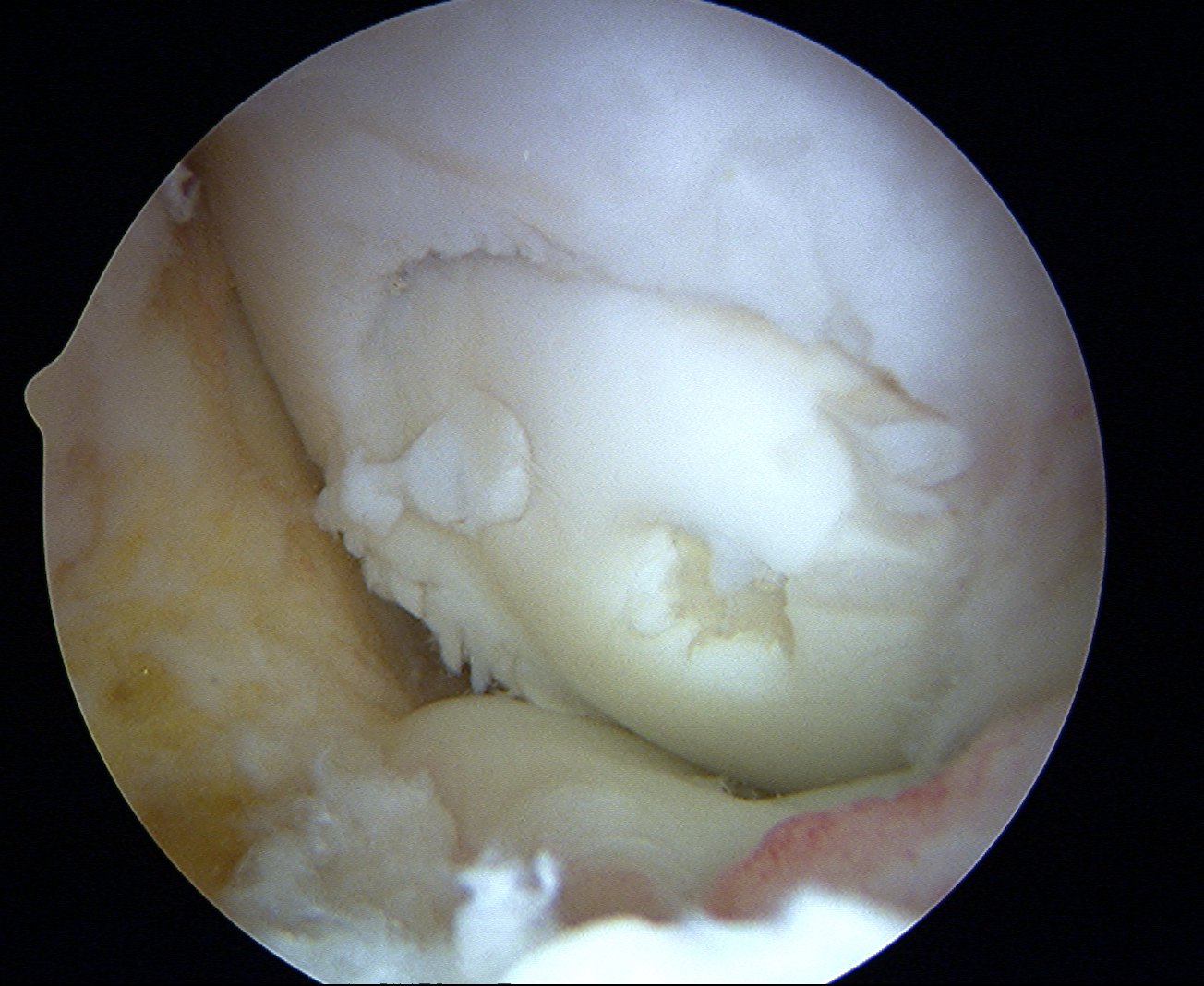
MFC OCD on presentation T2 image 6 months later

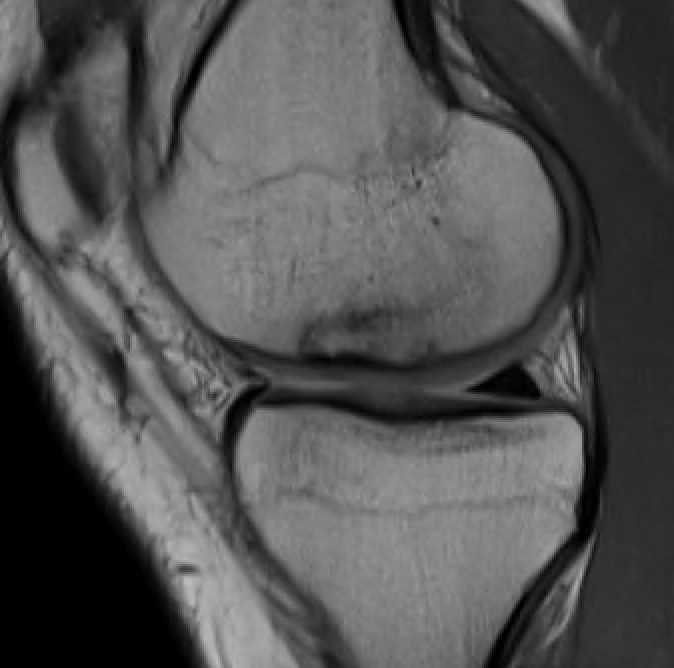
T1 sagittal on presentation T1 sagittal six months later
Results
Overall
Andriolo et al. Cartilage 2019
- systematic review of 27 studies and 908 knees undergoing nonoperative treatment
- mix of adult and juvenile, stable and unstable OCD
- overall healing rate of 61%
- poorer prognosis was larger lesion size, worse OCD stage, skeletal maturity
Krause et al. Am J Sports Med 2013
- stable JOCD treated nonoperatively in 62 patients
- girls mean age 11 and boys mean age 12
- after 6 months, 67% showed no progression towards healing or signs of instability
- after 12 months, 51% showed no progression towards healing
- larger lesions and the presence of cyst like lesions associated with increased failure rates
- the presence and size of cyst like lesions >1.3mm was most important predictor of failure


Stable lesion with no cysts Stable lesion with cysts
Lateral femoral condyle
- 43 knees in 37 patients with stable LFC JOCD undergoing nonoperative treatment
- 33% failed to heal at 6 months
- all those with associated discoid meniscus failed
Takigami et al. J Paediatr Orthop 2022
- 44 knees in 37 patients with stable LFC JOCD (average age 9) undergoing nonoperative treatment
- no difference in healing rates between those with normal lateral meniscus and incomplete discoid meniscus
Operative Management
Algorithm
1. Stable lesions
- stable, no cartilage breach, no fluid behind lesion
- anterograde or retrograde drilling
2. Unstable and salvageable lesions
- fluid behind lesion on MRI
- cartilage breach on arthroscopy
- screw fixation

Unstable and unsalvageable OCD
- fragment removal
- cartilage restoration procedure +/- realignment if needed
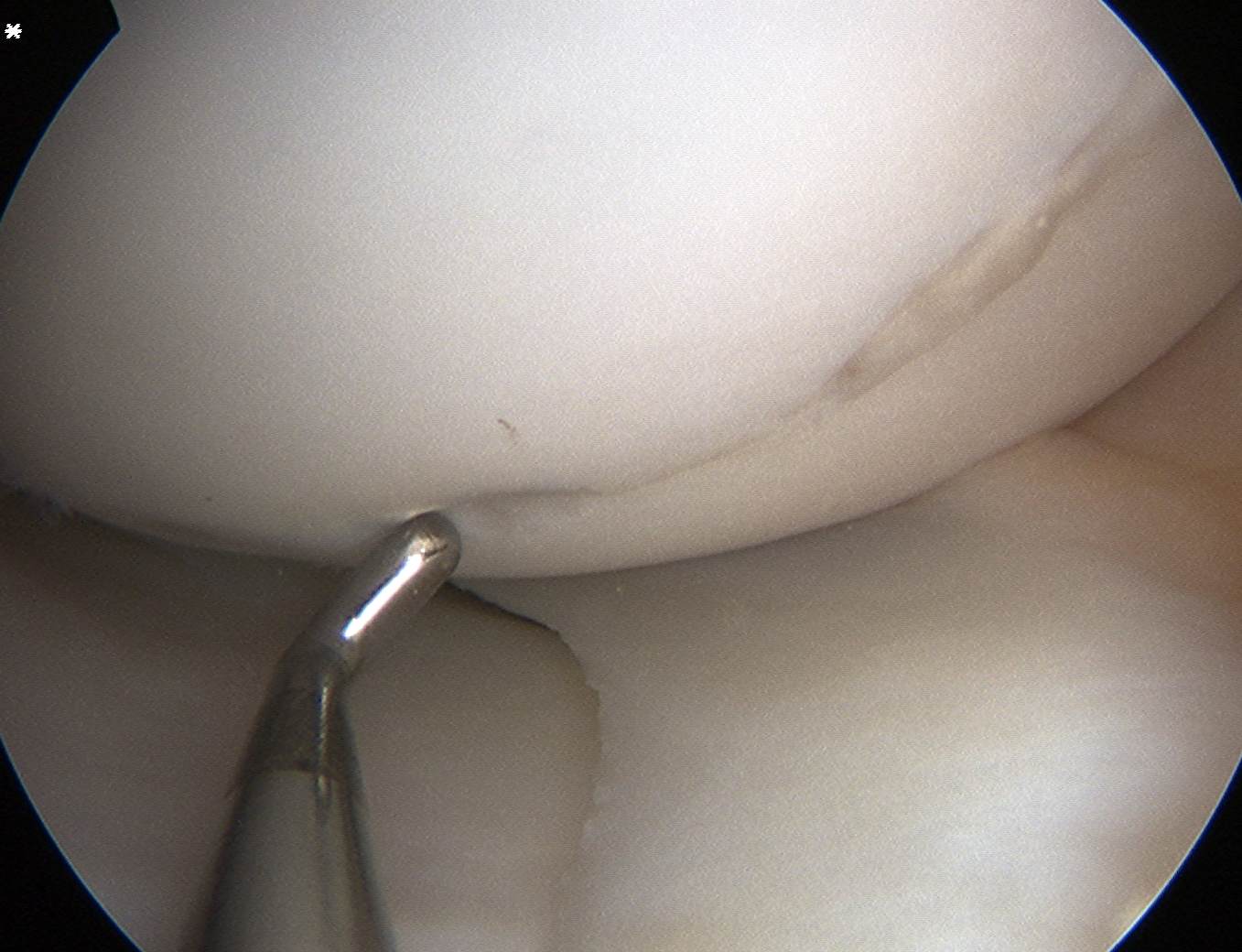
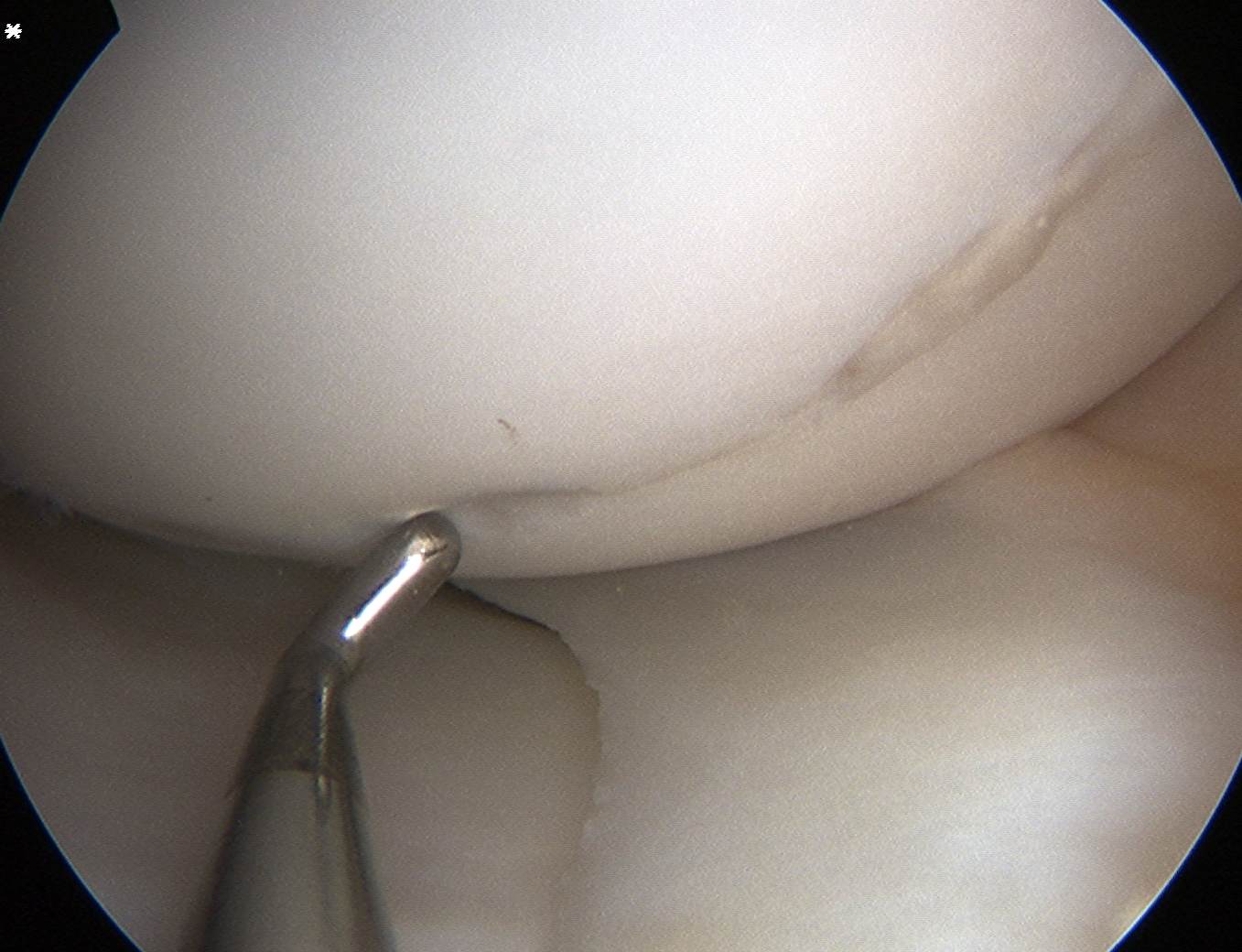
Drilling in situ
Indications
Failure non operative management > 6 months
Stable on MRI - no fluid behind lesion
Cartilage intact on arthroscopy
Concept
Aim to stimulate vascular ingrowth and subchondral healing
Antegrade v retrograde
Antegrade
- easy to do
- damages cartilage
Retrograde
- image intensifier or PCL guide
- more difficult but preserves cartilage
Results
- SR of JOCD treated with retrograde v antegrade drilling
- 86% radiographic healing with retrograde drilling by 5.6 months
- 91% radiographic healing with anterograde drilling by 4.5 months
- no significant difference
Baghdadi et al. Arthrosc Sports Med Rehab 2022
- 139 knees in 131 patients average age 13
- 16% bilateral
- 91% transarticular
- 96% healing rate
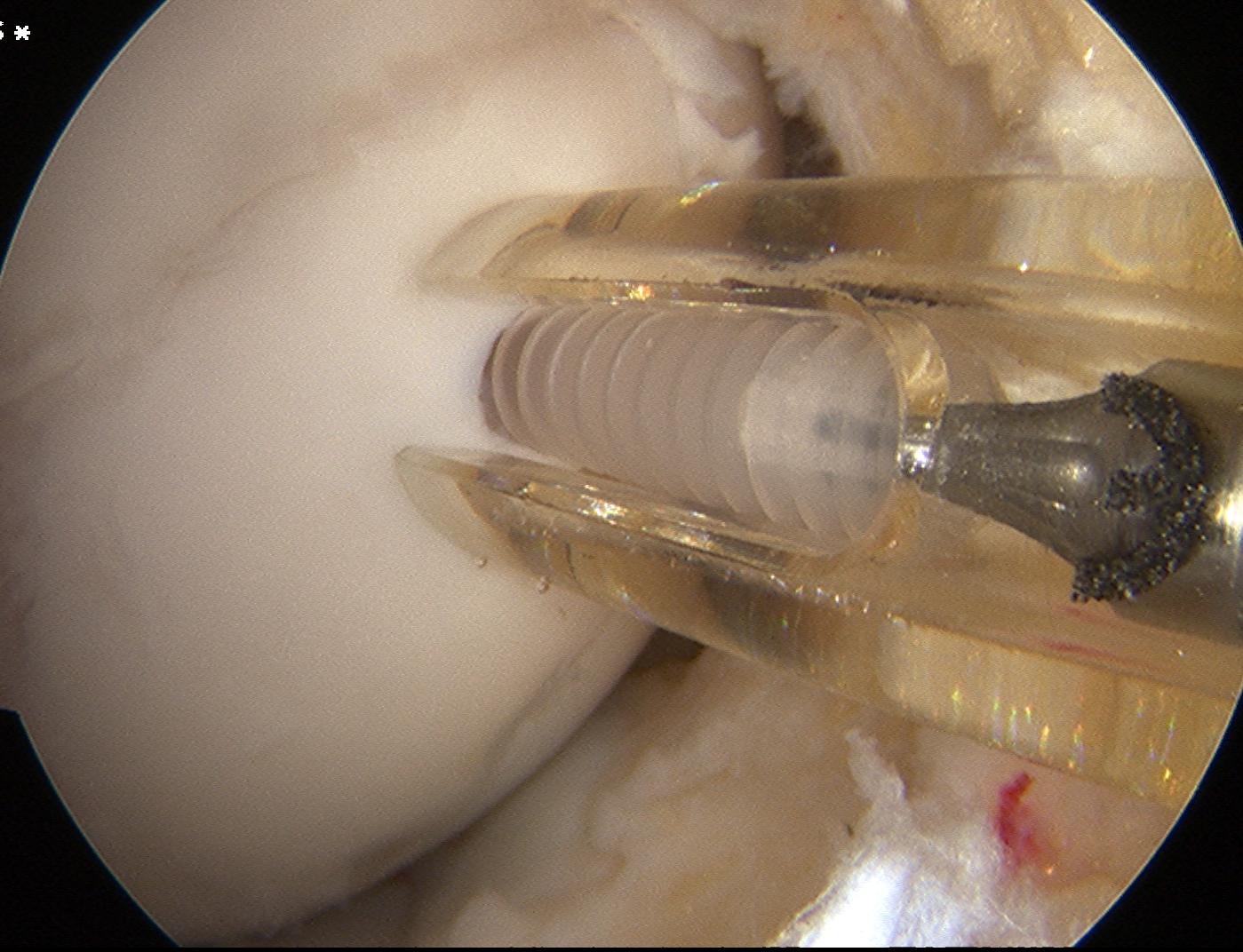
Technique
In a stage 1 lesion there is no cartilage breach
- the MFC / LFC looks normal
- use MRI to identify site of lesion
- i.e. usually adjacent to PCL insertion for MFC OCD
- central LFC for LFC OCD
5 - 10 drill holes
- 20 mm deep
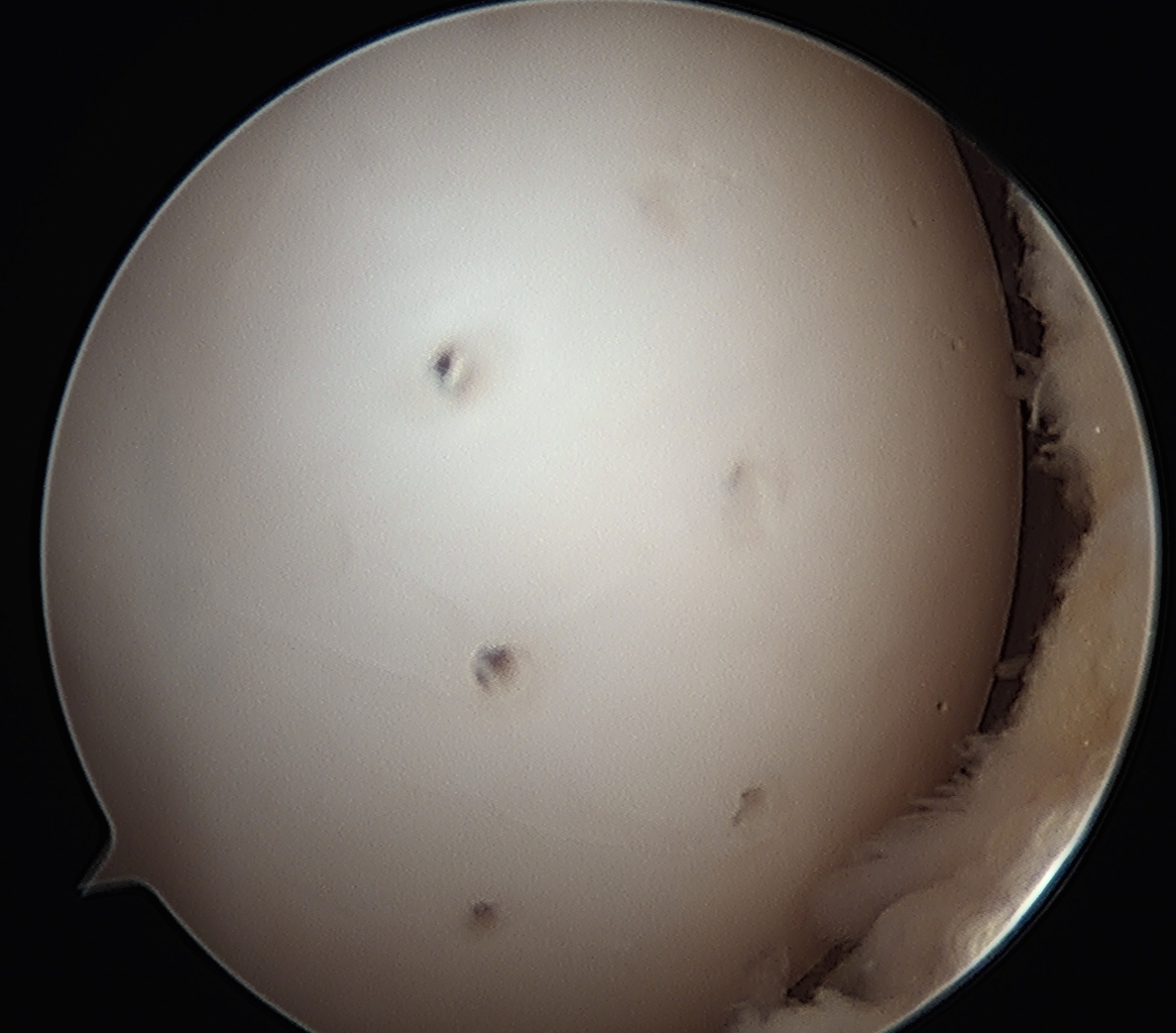
Transarticular drilling of LFC OCD

Transarticular drilling of MFC OCD
Rehabilitation
Crutches and protected weight bearing 4 - 6 weeks
No sports 6 months
MRI 3 and 6 months



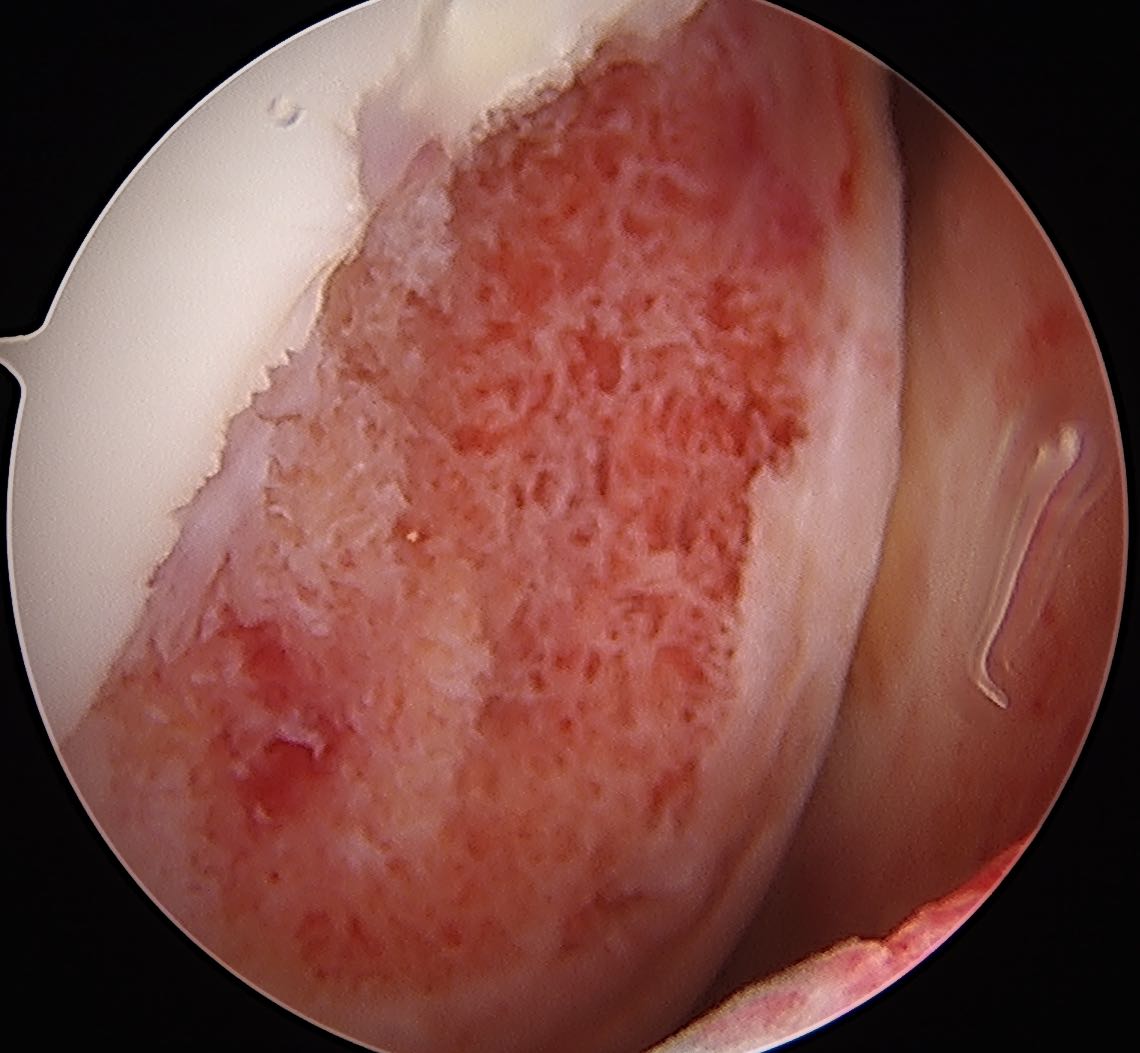
Progression of reossification over 6 months following drilling
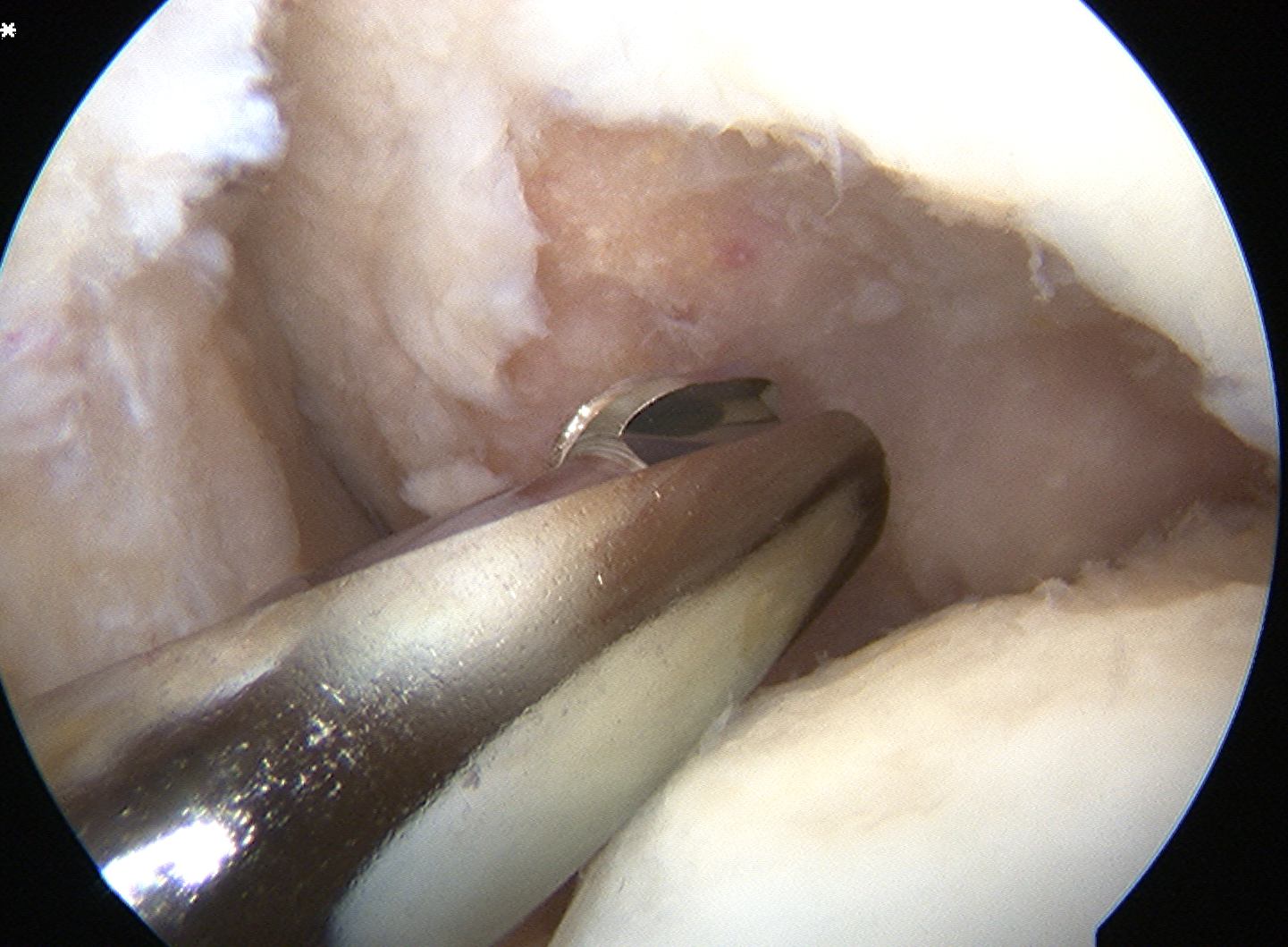
Screw fixation
Indications
Unstable lesion
Salvageable

Options
Open or arthroscopic
Cannulated headless variable pitch compression screws
- metal or bioabsorble
Consider bone graft
Yellin et al. J Paediatr Orthop 2017
- survey of 129 members of the Pediatric Orthopedic Society of North America
- majority use a metal or bioabsorble screw with no bone graft
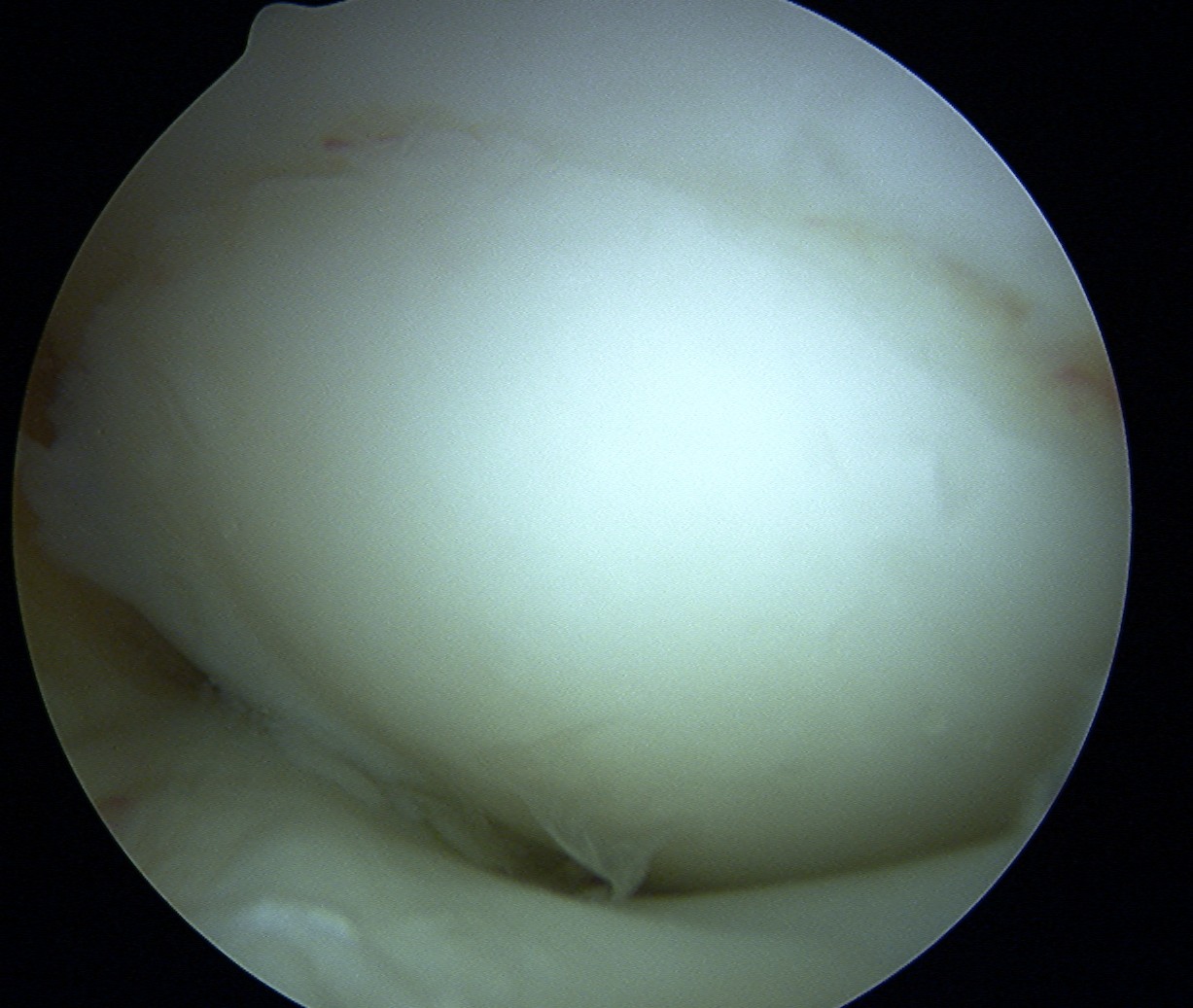
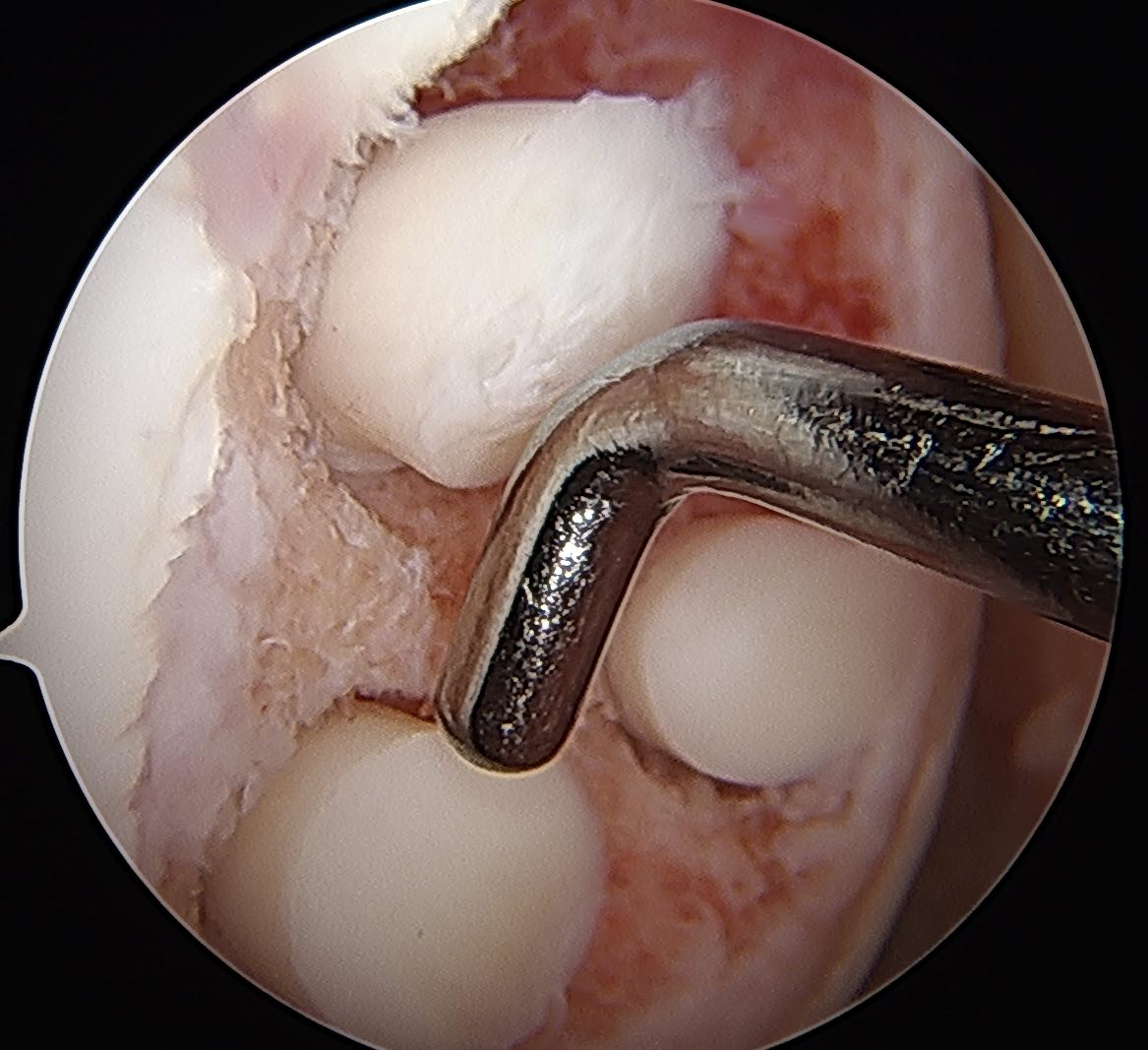
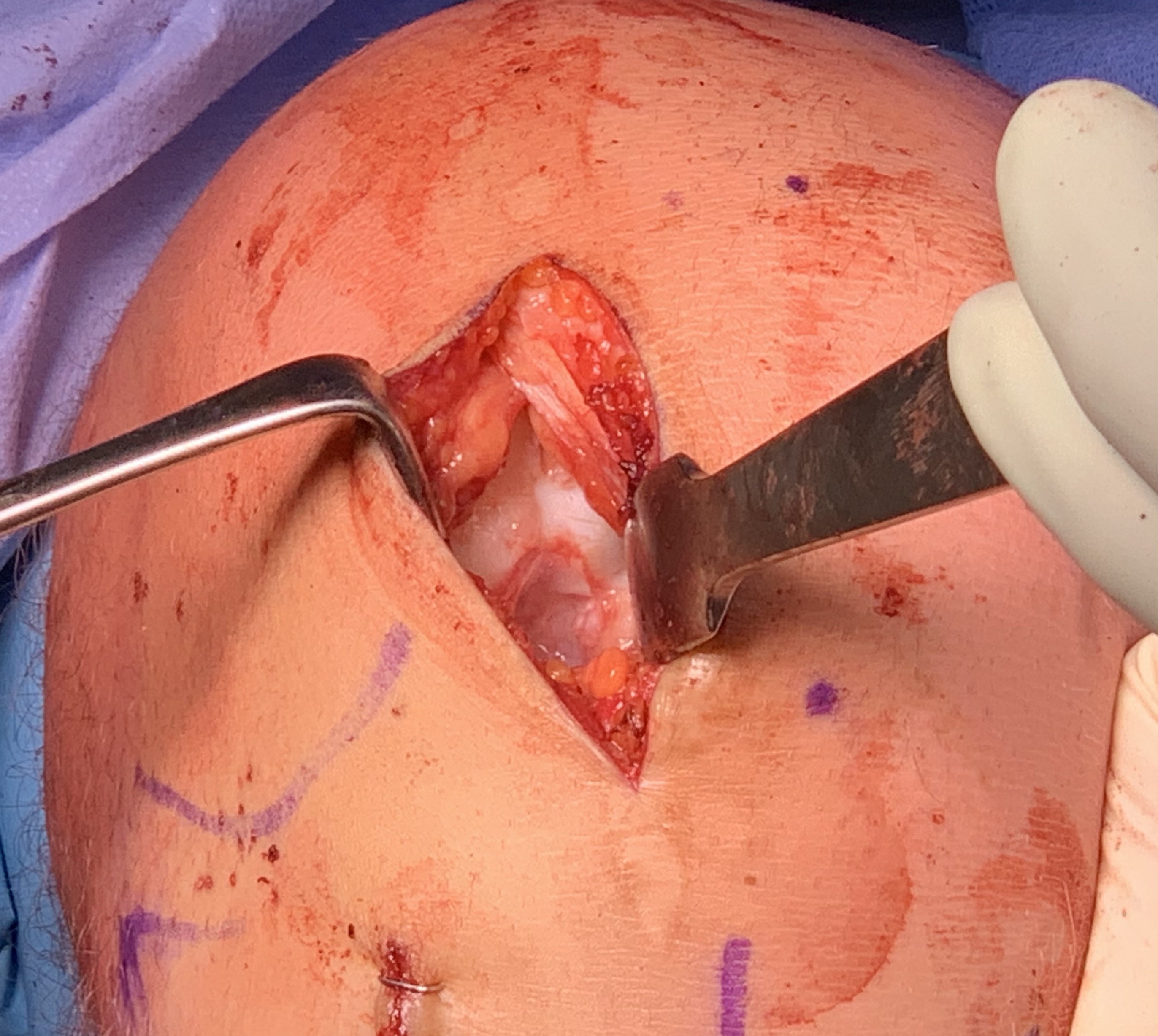
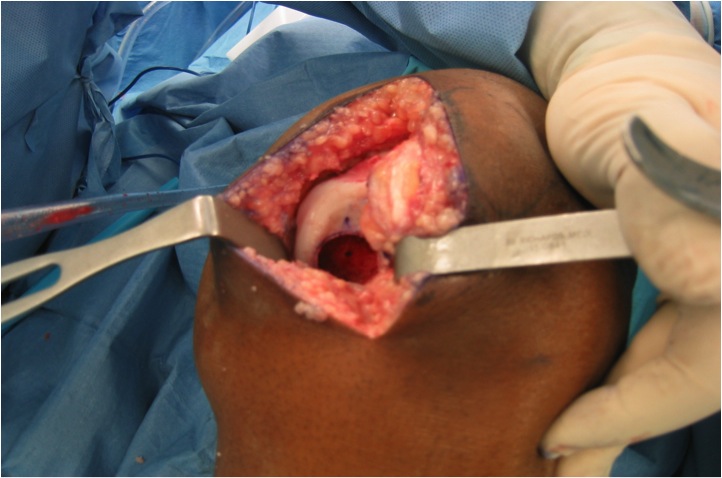
Arthroscopic Screw Fixation in situ
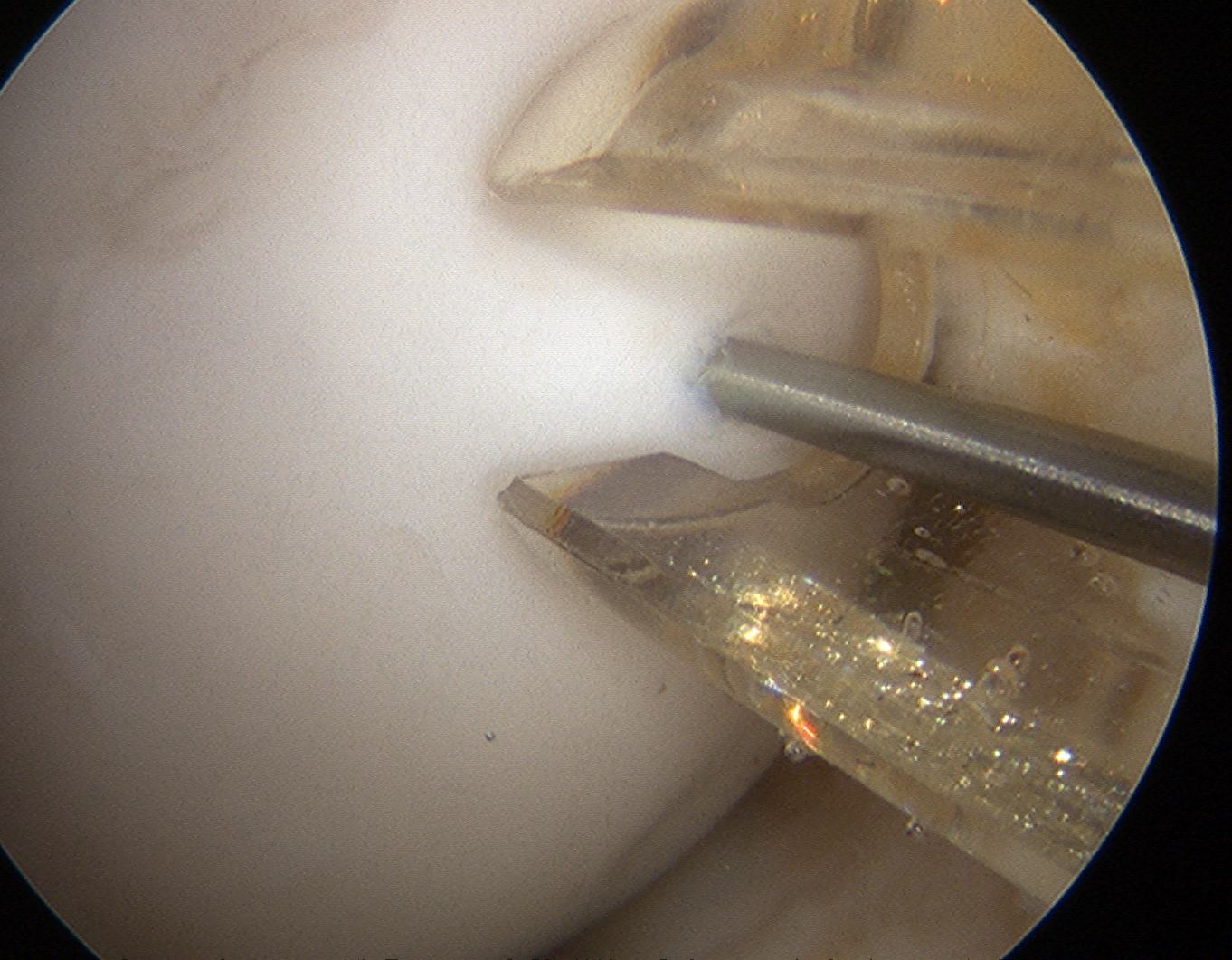
Arthroscopic bone graft and screw fixation
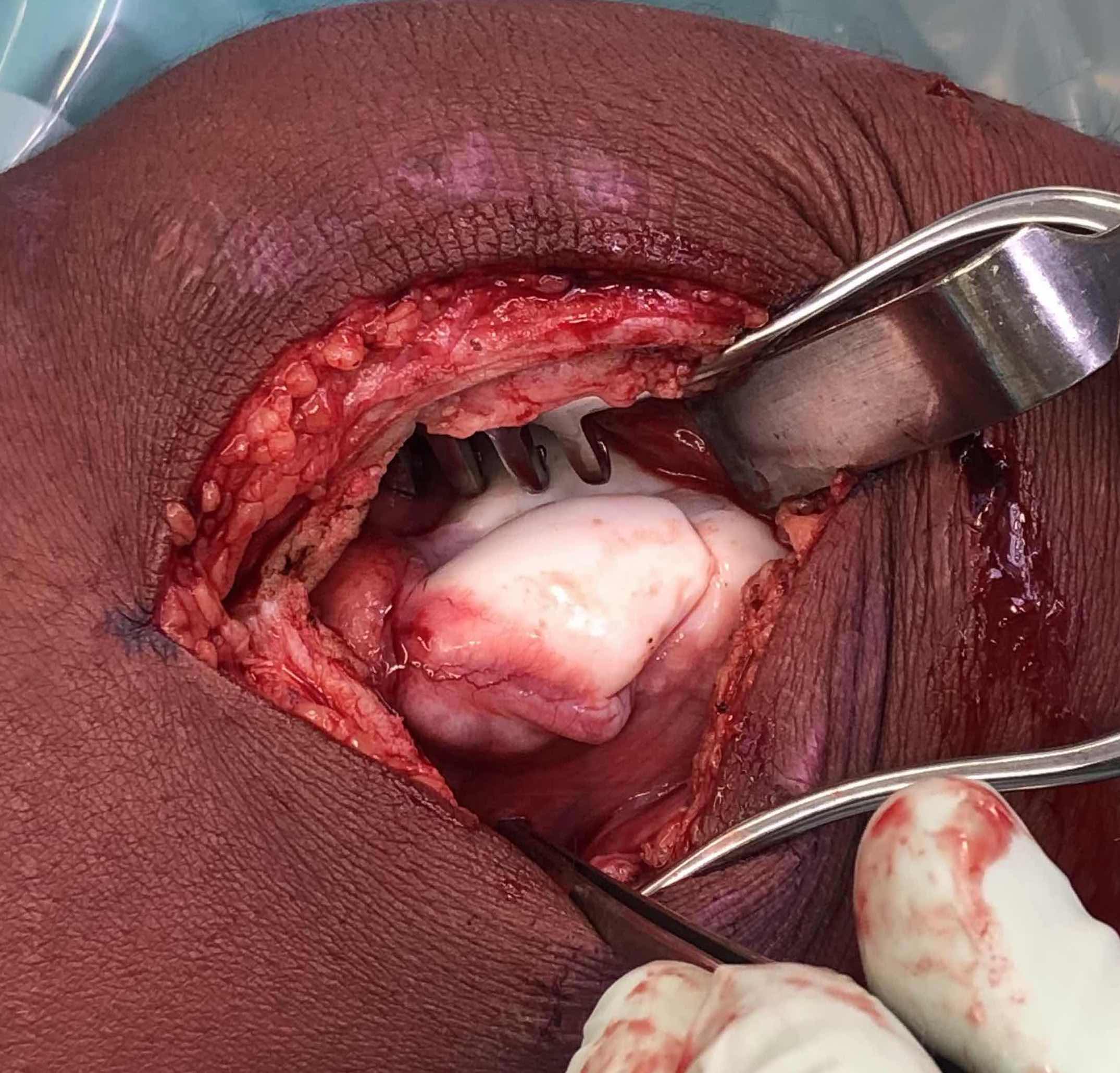
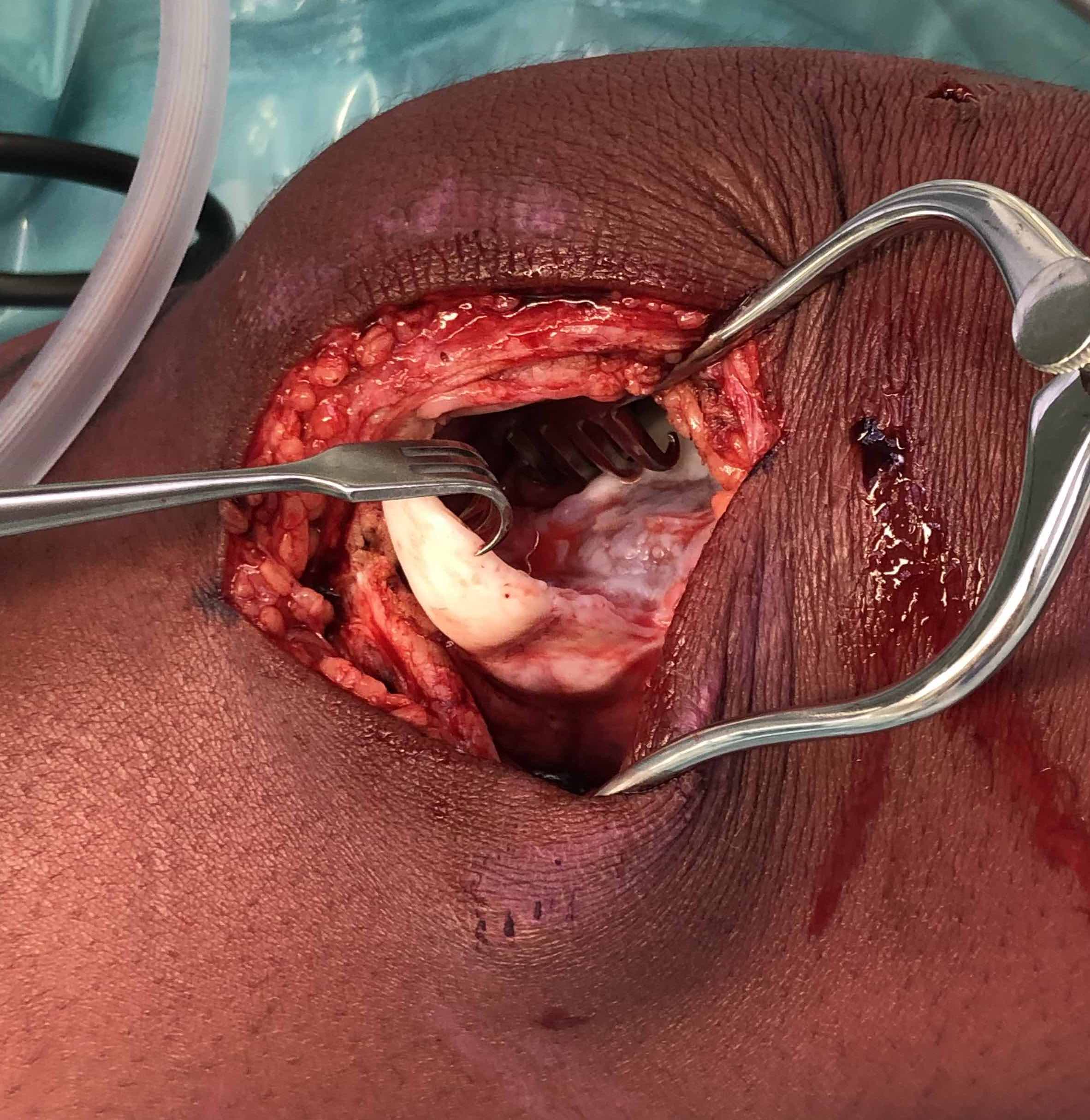
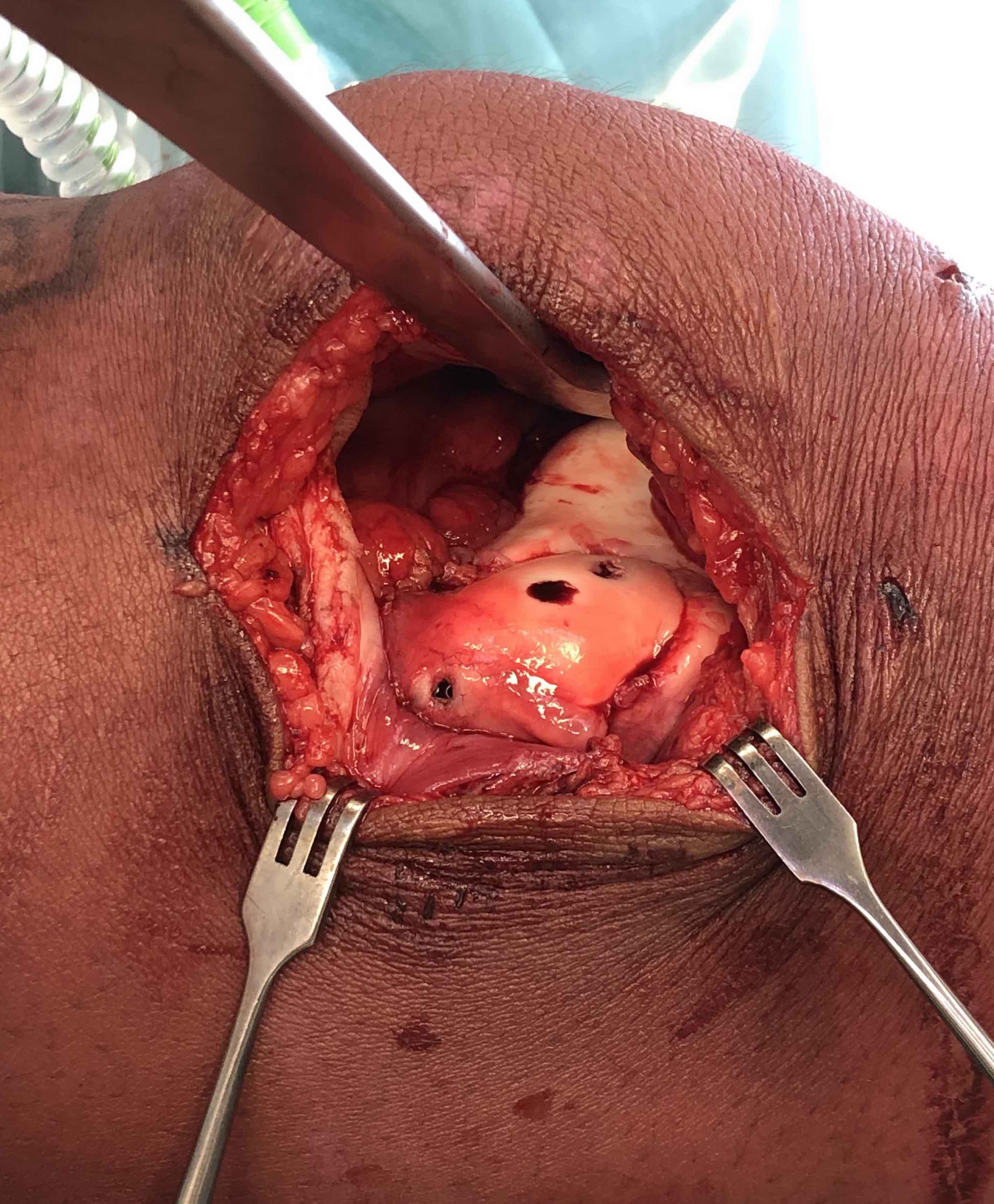
Open bone graft and screw fixation
MFC unstable OCD
LFC unstable OCD
Arthroscopic Mosaicplasty / OATS
Results
Miura et al Am J Sports Med 2007
- 12 unstable OCD treated with mosaicplasty plugs
- complete union on MRI in all cases
- 8 excellent and 3 good outcomes
- no donor site morbidity
Miniaci et al. Arthroscopy 2007
- 20 patients with unstable OCD treated with mosaicplasty
- MRI demonstrated bony healing in all patients at 6 months
- cartilage healing by 9 months
Assessing Union
Xray


Some reossification and evidence of union
MRI


Reossification and evidence of bony bridging
CT


Evidence of bony union on CT
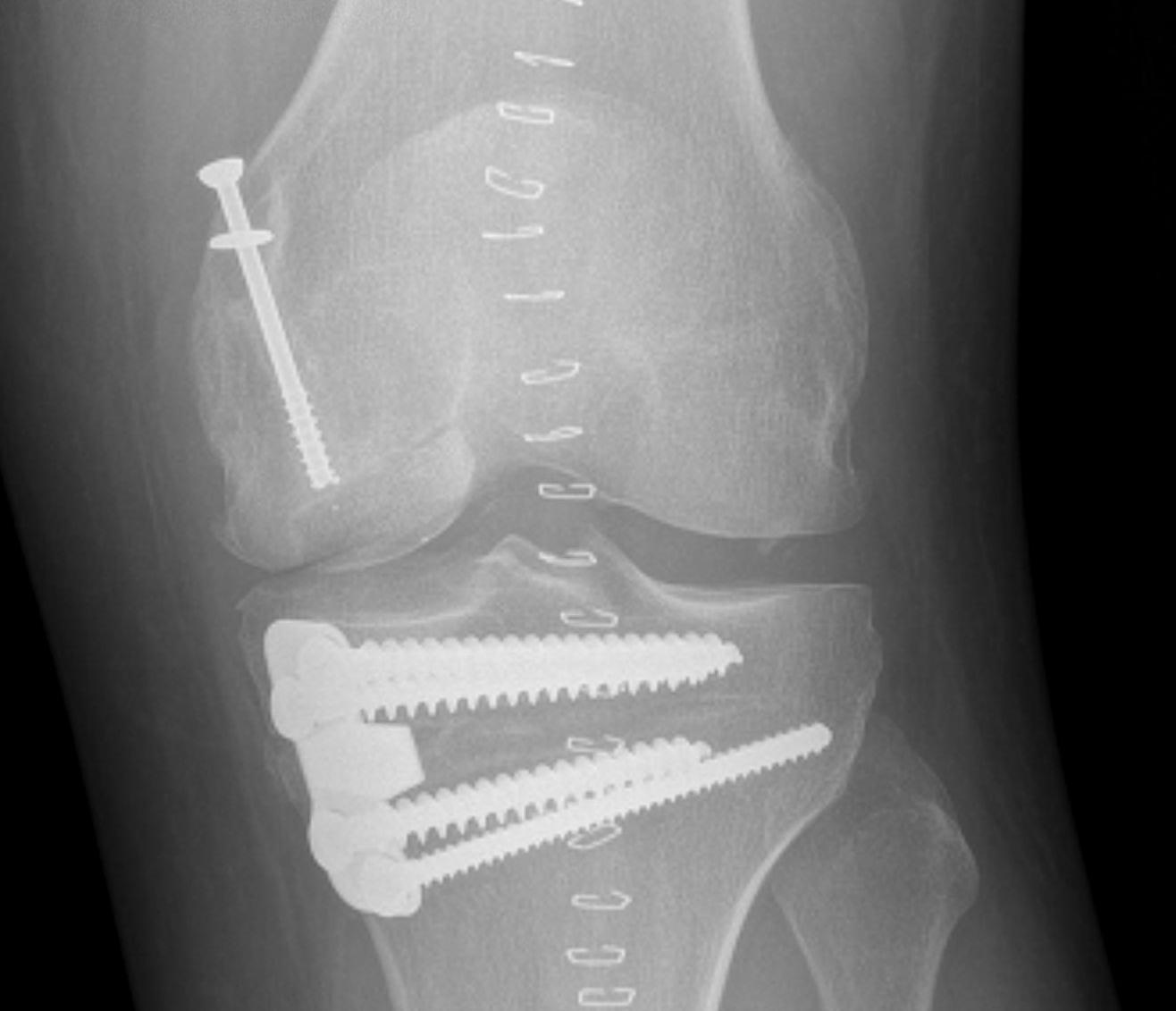
Results
- 87 patients undergoing screw fixation for unstable OCD
- 76% union rate at 2 years
- no difference between open or closed growth plates
- increased nonunion for LFC OCD
- retrograde drilling and bioabsorble pins in 40 patients mean age 13
- 84% union stage 3
- metal compression screws in 22 patients mean age 22
- union seen in 82%
Risk factors for non union
Fragmentation of piece
Thin bony fragment
Unsalvageable OCD / failed OCD fixation



Failure of fixation Chronic displaced fragment Fragmented OCD Fully detached OCD
Issue
Important to address osteochondral defect
- OCD fixation: OA 7% at 10 years, 25% at 20 years, 50% at 30 years
- fragment excision: OA 17% at 10 years, 40% at 20 years, 70% at 30 years
Options
Microfracture
Usually inappropriate for osteochondral defects
Mosaicplasty +/- osteotomy
Defect often too large for 4.5 mosaicplasty plugs
Number required to fill defect often results in donor site morbidity
Autologous chondrocyte implantation (ACI) +/- osteotomy
- 55 patients with 61 unsalvageable OCD treated with ACI
- average 19 year follow up
- 61% reached pre-injury level function
- 85% 15 year survival
Autologous Matrix Induced Chondrogenesis (AMIC) +/- osteotomy
Microfracture base +/- bone graft
Application of collagen patch - secured with sutures or Tisseal fibrin glue


Bertho et al. Orthop Traumatol Surg Res 2018
- 13 patients with large osteochondral defects treated with AMIC and bone grafting
- 11/13 had satisfactory outcomes
Osteochondral Allograft +/- osteotomy


- 135 patients with 149 knees
- osteochondral allograft for unsalvageable OCD
- 93% 10 year survival (based on revision allograft, or arthroplasty)
