Implant Options
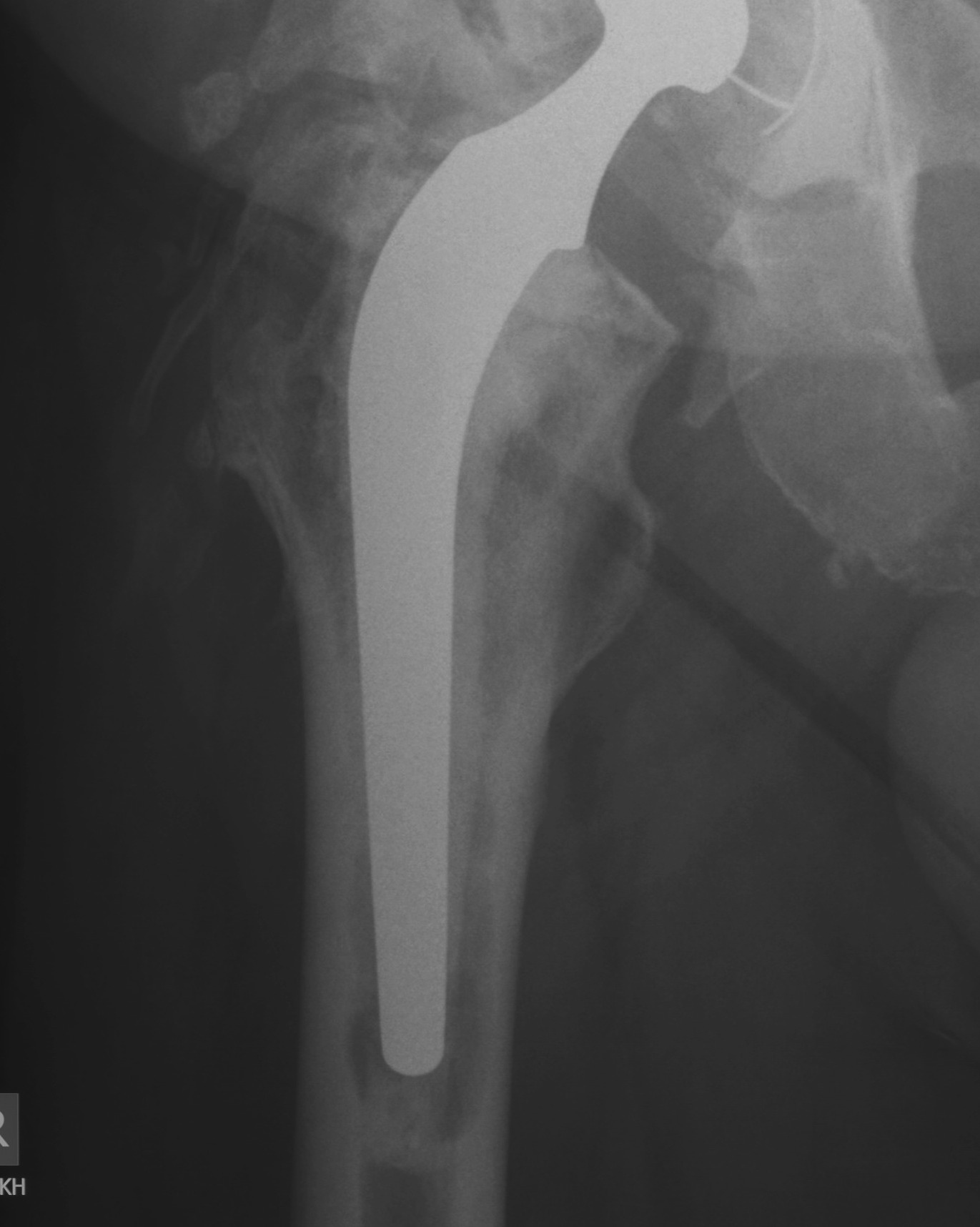
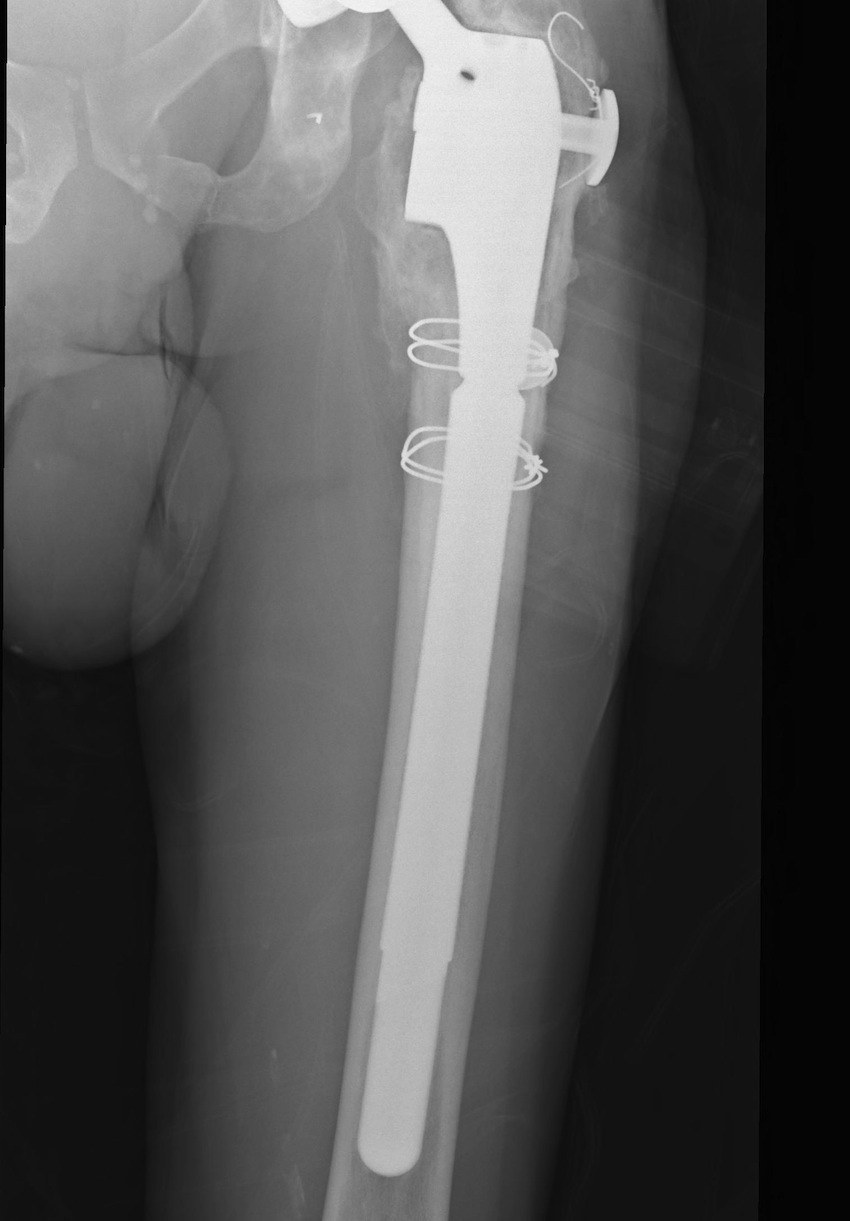
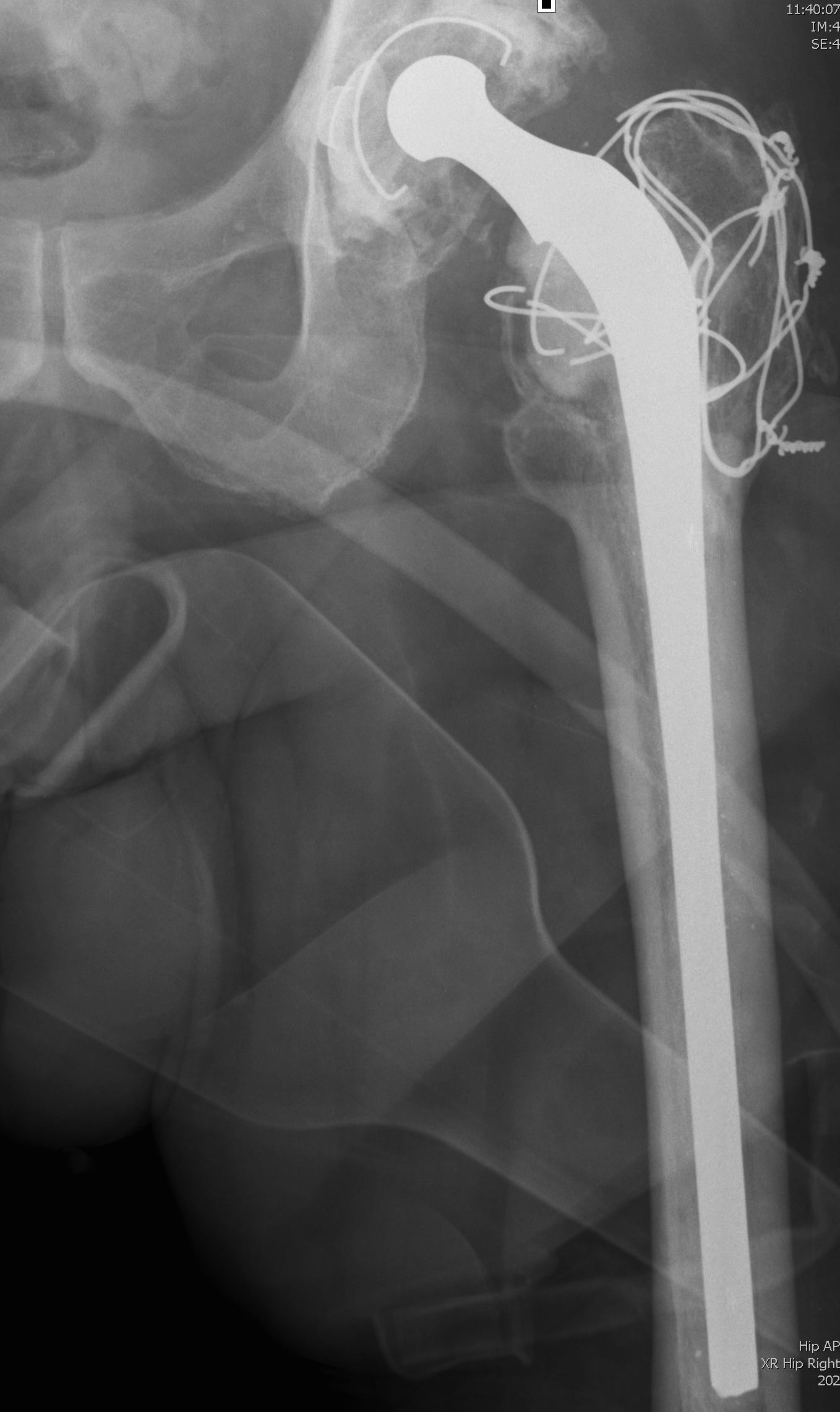
1. Long stem cemented revision femoral stem
Modern cementing techniques
- removal of neocortex
Advantage
- use in all cases
- good with elderly fragile bone
- can use Abx cement (decreases infection rate)
Indications
- Paprosky Types I – IV
- very versatile
Technique
- complete removal / debridement of neocortex
- modern cementing techniques
Howie JBJS Br 2007
- 219 patients, 9 year follow up
- collarless double taper
- 98% 10 year survival
Problems
- ? increased non union with ETO
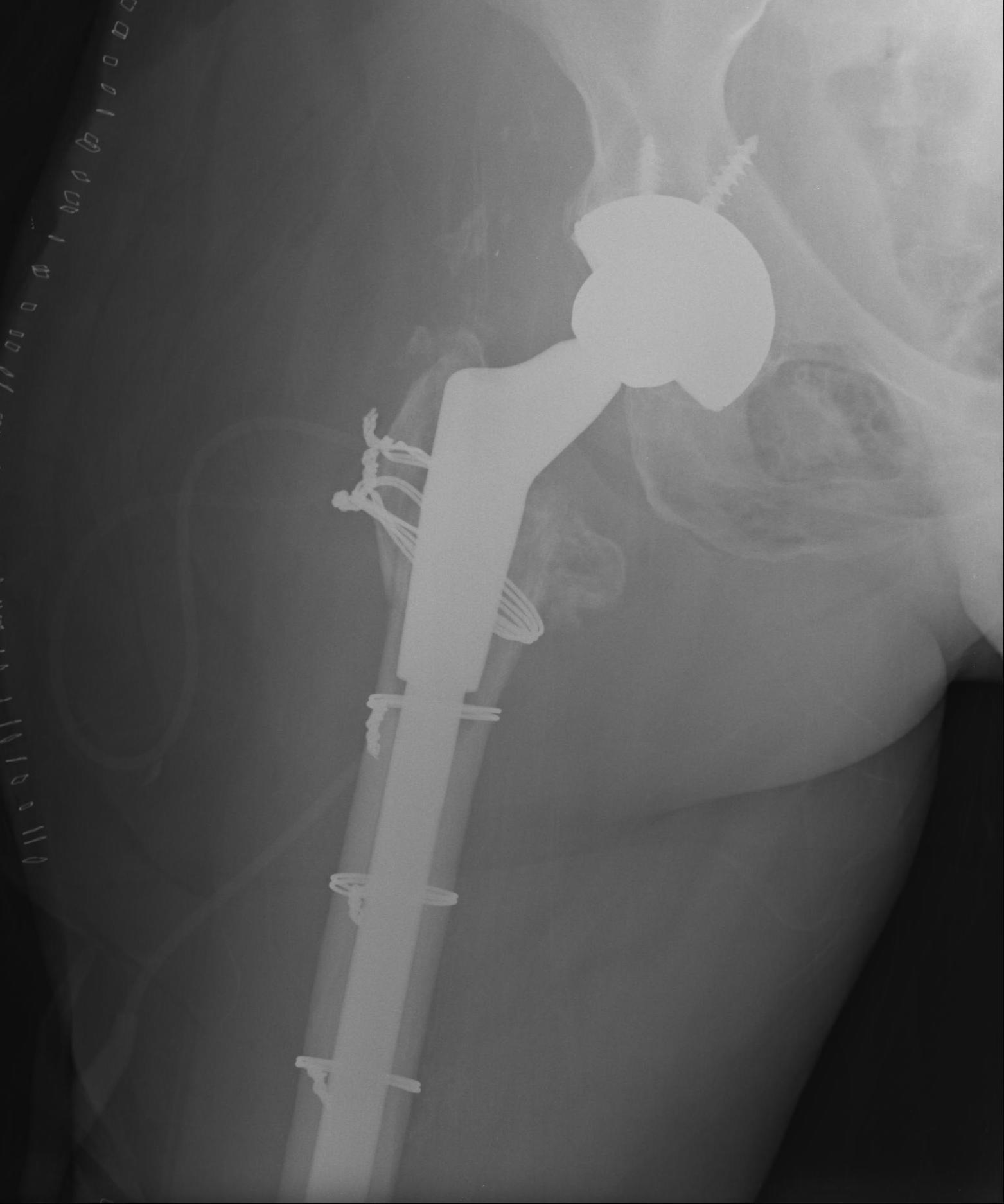
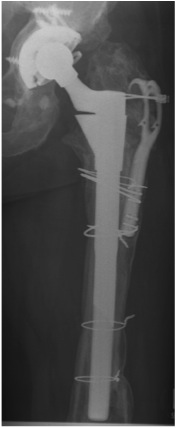
2. Extensively porous coated diaphyseal fitting uncemented stem
Indications
- Paprosky Types I, II, IIIA
Results
- 90- 95% 10 year survival
Problems
- fracture
- stress shielding with additional proximal bone loss
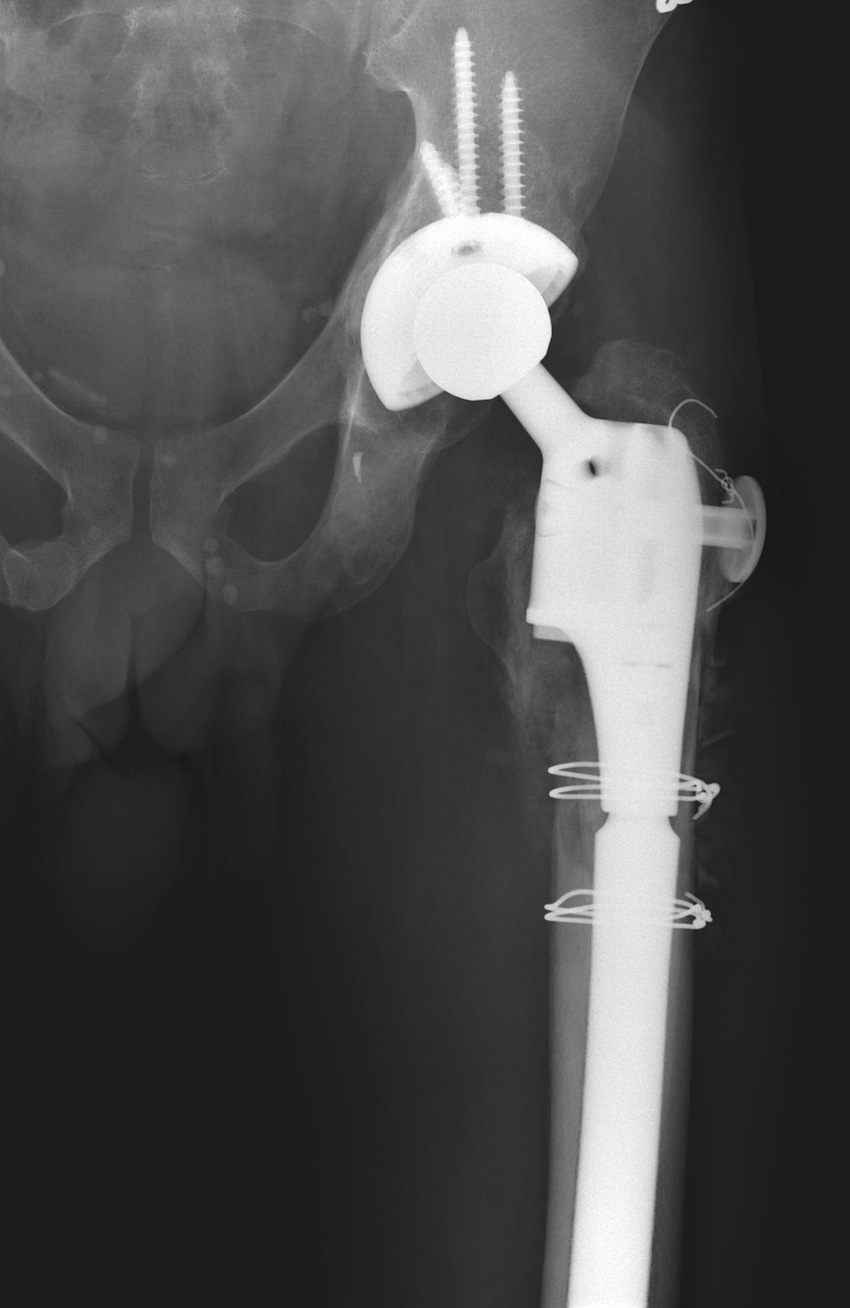
3. Modular diaphyseal fitting, proximal filling uncemented stem

Design
- press fit metaphyseal segment
- slotted diaphyseal segment
- initial stability through distal fixation
Indications
- Paprosky Types I – IIIB
Smith J Athroplasty 1997
- nil revisions at 5 years
- 7% radiographically loose
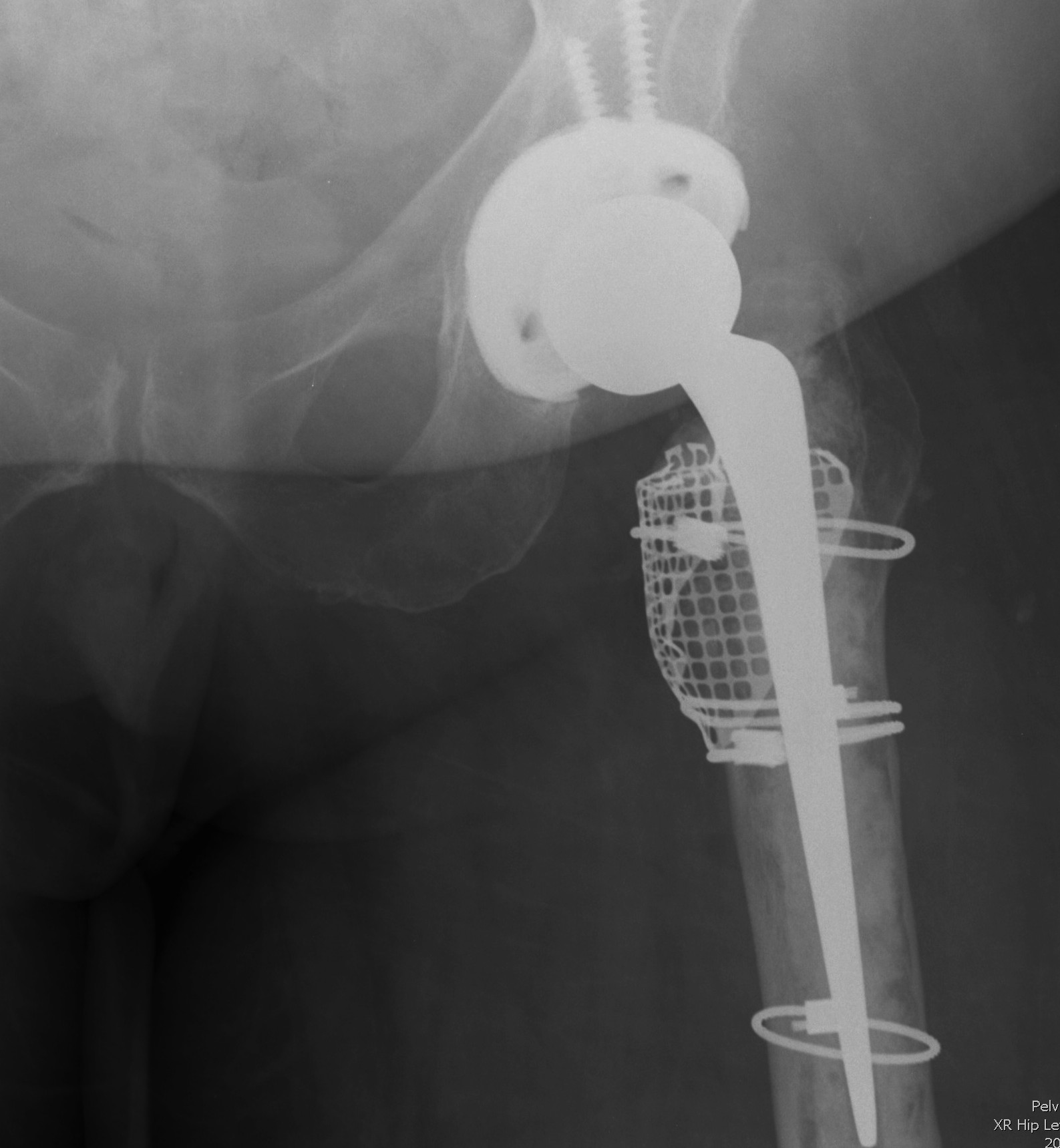
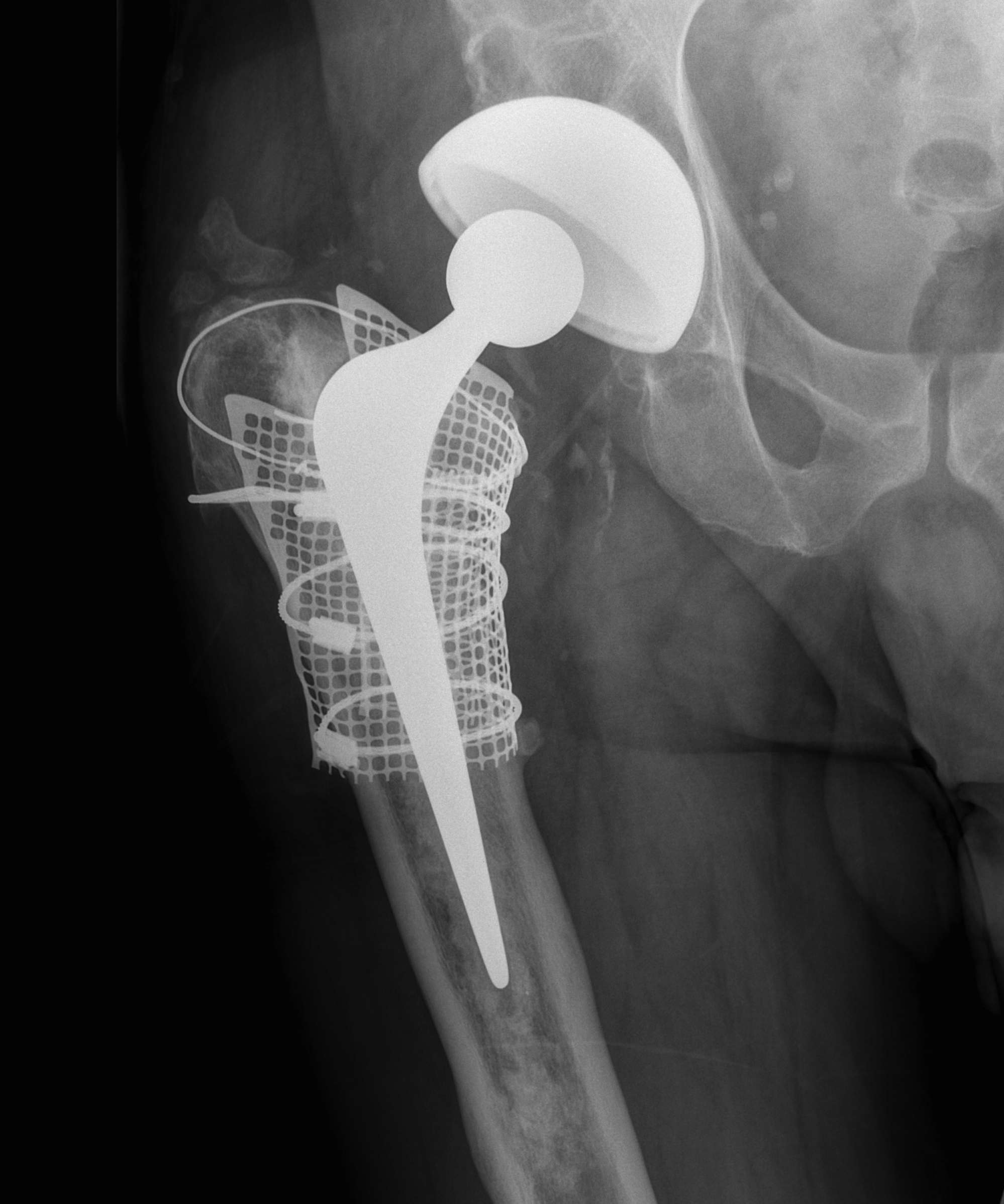
4. Impaction bone grafting
Concept
- morcellised bone graft is osteoconductive, not osteoinduction
- resorption and eventual replacement new bone
- 6 – 12 months
- process is incomplete
Van der Donk Clin Orthop 2002
- 30% complete 6/12
- 90% complete 12/12
Requirements
1. Particulate cancellous autograft 7-10 mm
2. Contained defect
3. Ability to convert uncontained into contained (i.e. mesh)
Issues
- technically demanding
- takes time
- need axial and rotational stability
- avoid stem subsidence > 5 mm
Indications
1. Uncemented distal fixation not possible (< 4cm diaphysis)
2. When reconstruction of proximal bone stock important
- young patient in whom biological solution more desirable
Technique
Templating
- choose stem 2 cortical diameters longer than most distal lytic area
Exposure
- full exposure of proximal femur
- removal stem & cement
Can leave distal plug
- not infected
- > 2 cm past planned tip location
Create contained defect
- reconstitute femoral tube
- create contained defect
- wire mesh & cerclage wire
- prophylactically cerclage wire shaft if diaphysis flimsy
Distal Occlusion
- threaded intramedullary plug inserted on guide rod
- impacters tested to see max depth of insertion before abutment on canal
- morsellised allograft inserted
- impactor & slap hammer slid over guide wire
- graft impacted to predetermined depth
- continued by introducing more chips with larger impacters
- stopped when level is 10 cm from tip of GT
Proximal Impaction
- appropriate proximal impactor equivalent to selected stem used
- used to force chips against walls of canal
- then larger distal impactor used
- alternated till canal filled
- should be firm neo-canal
Trial Reduction
- trial stem inserted
- depth of insertion marked
- proximal impactor driven in another 5 mm
- creates room for cement
Prosthesis
- cemented polished collarless double tapered stem
Post-op
- NWB for ? 3/52
- then gradual inc over next 3/ 12
Results
Halliday JBJS Br 2003
- 90.5% 10 year survival
Elting Clin Orthop 1995
- 93% graft incorporation
- stem subsidence in 48%
Elridge JBJS Br 1996
- > 5 mm subsidence in 22%
Management Plan
Assess Metaphyseal & Diaphyseal Bone Stock
Grade Paprosky, then manage appropriately
Paprosky Type 1
Definition
Minimal metaphyseal cancellous bone loss
Intact diaphysis
Options
Simple revision
- can use standard or any revision stems
A. Uncemented
- standard length proximal fit and fill
- need appropriate initial stability
B. Cemented standard length stem
- must remove neocortex
- need good cement interdigitation
Izquierdo JBJS Br 1994
- 90.5% 19 year survival
C. Cement onto old mantle
- clean and dry mantle critical
- thin layer of blood 85% reduction shear strength
Lieberman et al JBJS Br 1993
- 19 cases
- no loosening at 5 years in all

Type 2
Definition
Extensive metaphyseal cancellous bone loss
Diaphysis intact
Options
A. Extensively porous coated diaphyseal fitting implant
Paprosky 90& osteointegrated
B. Long stem cemented revision stem

C. Modular diaphyseal fitting, metaphyseal filling uncemented prosthesis
D. Impaction bone grafting
Type 3A
Definition
Metaphysis non supportive
> 4 cm diaphysis proximal to isthmus


A. Extensively porous coated diaphyseal fitting implant
Paprosky 20/22 91% osseointegrated
B. Long stem cemented revision stem
C. Modular uncemented
D. Impaction bone grafting

Type 3B
Definition
Metaphysis non supportive
< 4cm diaphysis proximal to isthmus
Options
A. Extensively coated diaphyseal fitting
Paprosky 4/8 failed
- i.e. need > 4cm of diaphysis for this to work
B. Long stem cemented revision stem
C. Modular uncemented, stem with flutes for rotational stability
D. Impaction bone grafting
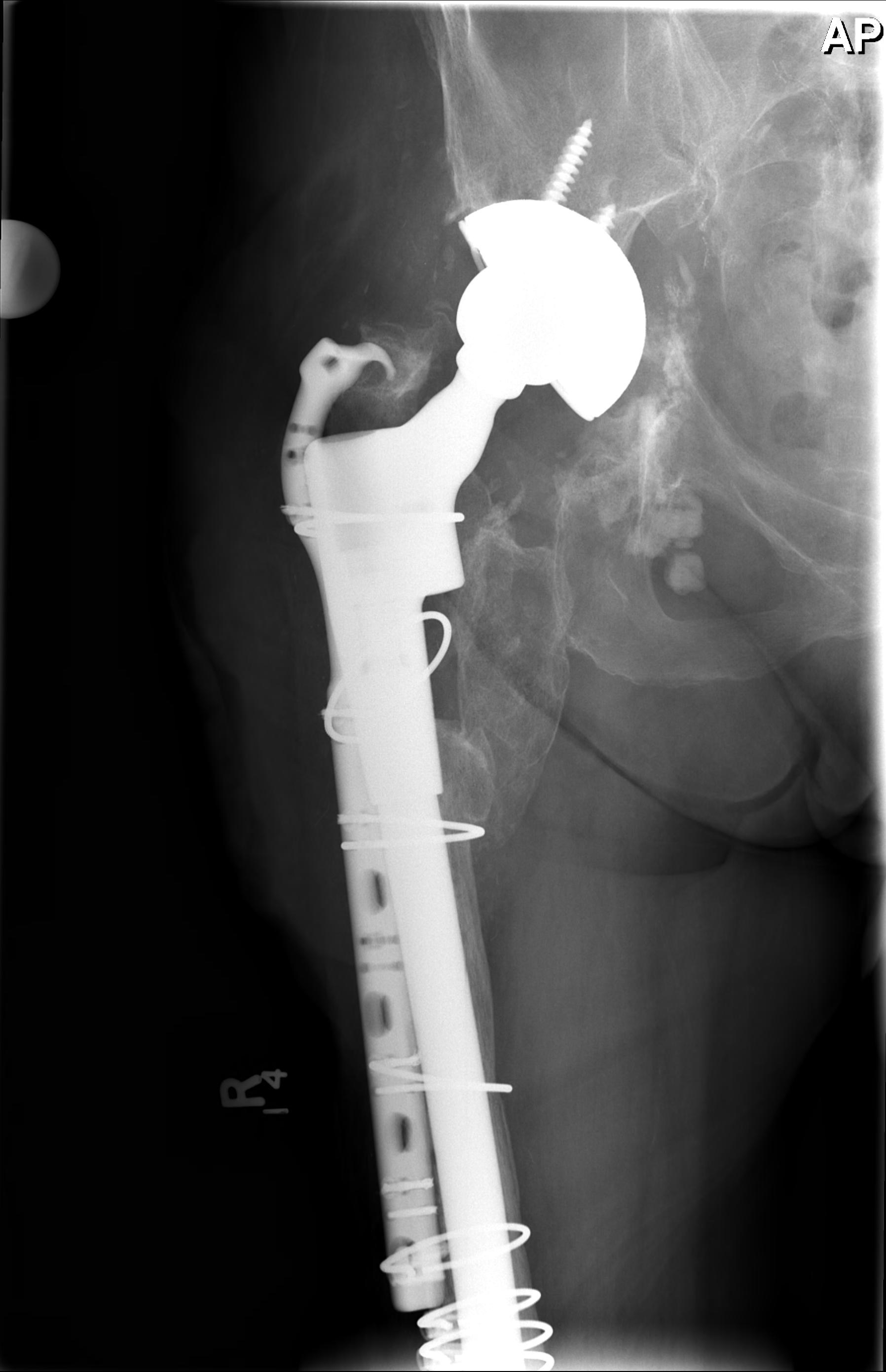
Type 4
Definition
Metaphysis and diaphysis extensively damaged
Isthmus non supportive
Options
A. Long stem cemented revision stem
B. Impaction bone grafting
Management Bone Defects
1. Segmental defects
A. Must bypass any cortical defect by two cortical diameters to reduce fracture risk
B. Cortical Strut onlay grafts
2. Extensive proximal bone loss
A. Calcar replacing
Indications
- proximal segmental defect < 3cm
McLaughlin JBJS Am 1996
- 38 hips 11 years
- 80% survival
- another 10% radiologically loose
- 20% dislocation rate
B. Napkin ring / Calcar graft Allograft
Indications
- circumferential proximal defects < 3cm
Results
- poor
- 40-60% resorption
C. Proximal Femoral Replacement / Tumour prosthesis
Results disappointing
- however design may be improving
Malkani JBJS Br 1995
- 33 hips 11 years
- poor function (50% severe limp or unable to walk)
- 64% 12 years survival
- 22% dislocation
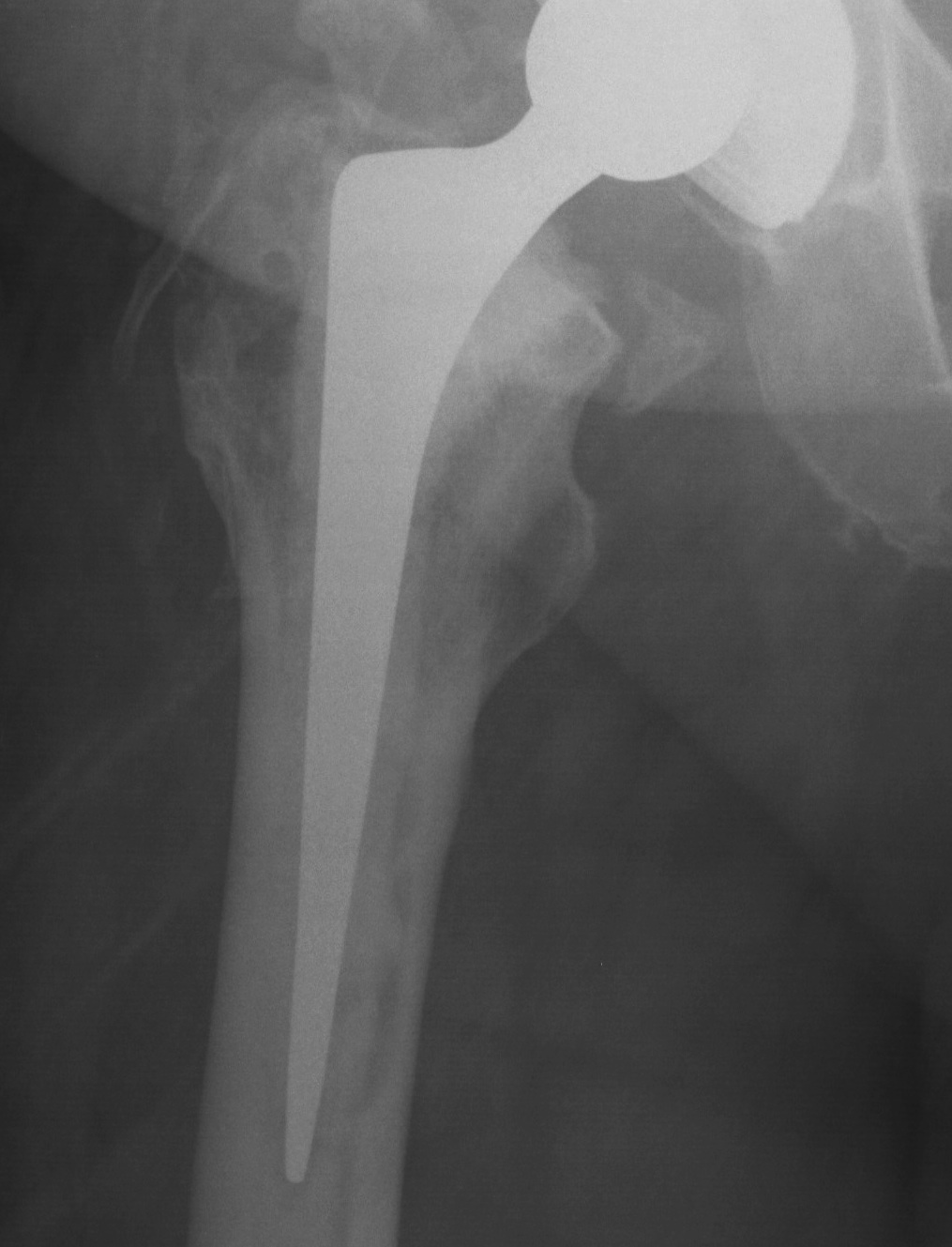
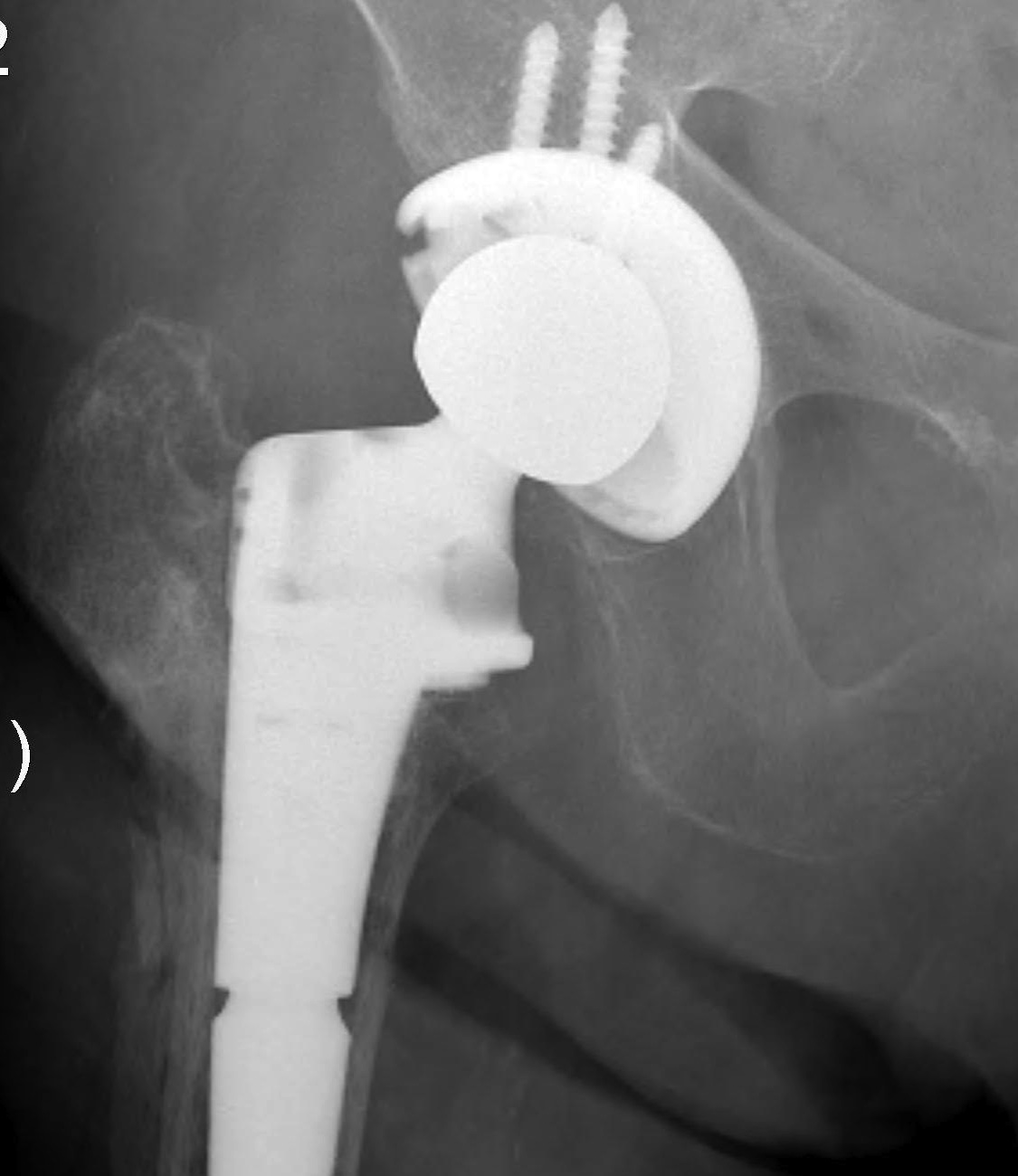
D. Bulk Structural Proximal Femoral Allograft
Indications
- proximal defect > 3 cm
Technique
- desired stem cemented into allograft
- press fit distally into host femur
- step cut graft host junction
- secure cerclage wire and onlay cortical strut
- proximal host bone wrapped around allograft with ABD preservation
- very important – abductor mechanism must be secured and protected
Gross 1998
- 200 patients, 5 years follow up
- 12.5% revision
- revised for infection, dislocation, graft-host non union
