Epidemiology

Most common long bone fracture
Aetiology
Young patients / sports
Elderly / simple falls
MVA - often compound
Tscherne Soft Tissue Classification
Grade 0
- nil ST injury
Grade 1
- superficial abrasion / contusion
- ST injury from pressure from within
Grade 2
- deep contusion / abrasion
- due to direct trauma
Grade 3
- extensive contusion and crush
- subcutaneous tissue avulsion
- severe muscle injury
Operative v Nonoperative
Acceptable alignment
Lindsey et al. JAAOS 1996
- coronal plane > 5o
- saggital plane > 10o
- rotation > 5o
- shortening > 1 cm
- displacement > 50%
- comminution > 50%
Nonoperative treatment
Advantages cast
- no infection
- no knee pain
- no hardware to remove
Advantage IMN
- faster union
- reduced non union
- reduced malunion
- earlier ROM
- able to weight bear early
Swart et al. Injury 2021
- 334 patients treated nonop
- fractures reduced, and placed in cast
- 70% converted to surgery due to inability to maintain alignment or patient issues
https://pubmed.ncbi.nlm.nih.gov/33046252/
Puno et al. CORR 1986
- IMN nonunion rate 2%, malunion 0%, infection 3%
- cast nonunion rate 10%, malunion 4%, infection 0%
https://pubmed.ncbi.nlm.nih.gov/3769277/
Operative Treatment
Options
1. IM Nail
2. Plate
3. External Fixation
1. IMN Tibia


Reaming
Xia et al. Orthopedics 2014
- meta-analysis of 9 RCT, 1200 patients
- reaming reduced risks of nonunion, reoperation, need for dynamisation and exchange nailing
https://pubmed.ncbi.nlm.nih.gov/24762836/
Infrapatellar Flexed v Suprapatellar Semi-Extended
Gao et al. Medicine 2018
- meta-analysis of 4 RCTs
- suprapatellar approach reduces blood loss, and reduces fluoroscopy time
- suprapatellar appraoch improves postop pain, and has improved knee outcomes scores
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6023710/pdf/medi-97-e10917.pdf
Surgical technique article
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4894781/pdf/bco-27-107.pdf
Vumedi video
- potential techniqual advantages suprapatellar
- easy lateral xrays
- easier to obtain perfect starting point
- better to obtain and maintain the reduction for proximal tibial fractures
Post operative weight bearing
Gross et al. J Orthop Trauma 2016
- RCT weight bear v NWB in 90 fractures (exclude OTA 42C - segmental or severely comminuted)
- no difference in union rates, or complications
- concluded that immediate weight bearing is safe in stable fractures
https://pubmed.ncbi.nlm.nih.gov/27049908/
Segmental shaft fractures



Corey et al J Orthop Trauma 2018
- 95 treated with IMN
- nonunion rate 10%
https://pubmed.ncbi.nlm.nih.gov/29432320/
2. Plate fixation


Risk
- poor skin / blood supply / muscle cover
- excessive soft tissue stripping
Technique
- minimally invasive
- indirect reduction techniques
Results
He et al. Clinics 2014
- meta-analysis of 11 studies
- MIPO plate v IMN
- faster union rates with plate
- no increased infection or reoperation
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3971355/pdf/cln-69-04-234.pdf
3. External fixation
Indications
Contaminated wound
Vascular injury
Damage Control Orthopedics
Segmental bone loss - Ilizarov
Technique
Unilateral
- 4 or 5 mm half pin
- predrill to decrease thermal necrosis
- 2 near fracture and 2 far from cortex
- 2 bars / close to skin (2 cm)
Complications
Compartment syndrome
Incidence
Shadgan et al. J Orthop Traumatol 2015
- 1,125 patients with tibial shaft fractures
- 7% rate of acute compartment syndrome
- 64/87 required fasciotomy following surgery fixation
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4559534/pdf/10195_2014_Article_330.pdf
Symptoms / signs
- excessive pain not managed by opiates
- tight compartments
- pain on passive stretch of affected compartment
- parathesia
Compartment pressure monitoring
Normal compartment pressures
- > 30 mm Hg less than DBP
- < 30 mm Hg
Management
2 incision, 4 compartment release
Anterior Knee Pain after IMN
Incidence
Leliveld et al. Eur J Trauma Emerg Surg 2021
- systematic review
- incidence knee pain with infra-patellar approach 38%
- incidence knee pain with supra-patellar approach 10%
https://pubmed.ncbi.nlm.nih.gov/32772136/
Nail Removal
Zhang et al. J Orthop Surg 2017
- 57 patients with significant AKP following tibial IMN
- removal of nail helped
- espeically with < 10 mm between nail tip and tibial plateau
https://pubmed.ncbi.nlm.nih.gov/28193138/
Infection
Incidence
Hendrickx et al. Injury 2020
- systematic review of > 8000 patients
- deep infection 3.2%
https://www.injuryjournal.com/action/showPdf?pii=S0020-1383%2820%2930352-1
Nonunion
Definition
- 9/12 since injury
- 3 consecutive months with no signs union
- when the fracture has not healed in what you would expect to be a normal time period
Incidence
Hendrickx et al. Injury 2020
- systematic review of > 8000 patients
- nonunion after tibial IMN 10%
https://www.injuryjournal.com/action/showPdf?pii=S0020-1383%2820%2930352-1
Risk Factors
1. Injury factors
- displacement
- high energy injuries - comminution, bone loss, segmental fractures
- compound / open injuries
- vascular injuries
2. Patient factors
- malnutrition / smoking / diabetes / alcoholic
- immunosuppression / NSAIDS
- Paget's / renal osteodystrophy
3. Surgeon Factors
- fracture left displaced or distracted
- excessive soft tissue stripping
- infection
- nil reaming
Tian et al. J Orthop Surg Res 2020
- systematic review of 41,000 fractures
- risk factors for non union
- > 60, male
- smoking, BMI > 40, diabetes
- NSAIDS
- open fractures, OA Type C, high energy fractures
https://pubmed.ncbi.nlm.nih.gov/32883313/
Management Nonunion
Types
A. Hypertrophic
- abundant callous
- adequate blood supply, insufficient stability
B. Oligotrophic
- minimal callous
- still have adequate blood supply
- due to inadequate contact between fracture surfaces

C. Atrophic
- no callous
- deficient biology, adequate stability (too adequate)
Surgical Options (After excludIng infection)
Adjuncts - low intensity pulsed ultrasound
Dynamisation
Exchange nailing
Compression plating
Posterolateral bone grafting
External Fixation / Ilizarov technique
Dynamisation
Indications
- well aligned fracture
- mild gap
- no significant bone loss or comminution
- early - 3/12 or < 6/12
Advantages
- simple, day surgery
- minimal risks / complications
Technique
- take out screws furtherest from fracture
Results
Vaughn et al. Orthopedics 2016
- dynamisation effective in 50%
https://pubmed.ncbi.nlm.nih.gov/27575039/
Exchange nailing
Contraindications
1. Bone defect
- less likely to heal if > 50% cortex missing for > 2cm
- combine with posterolateral bone graft
2. Presence of infection
- much less likely to succeed
Technique
Remove old nail
- no preoperative ABx
- ream +++
- insert at least 1mm larger nail
- routinely send reamings for culture
Results
Tsang et al. Bone Joint J 2016
- 102 tibial non unions
- overall union rate 63% with single exchange nail
- union rate in setting of infected nonunion 35% (11/31)
- risk factors failure atrophic nonunion / bone gap > 5mm / infection
https://pubmed.ncbi.nlm.nih.gov/27037437/
Issues
1. Fibular Osteotomy
2. Dynamic v static locking
Abadie et al. J Orthop Trauma 2016
- exchange nailing for tibial nonunion
- fibular osteotomy associated with faster union by 3 months
- no difference static v dynamic locking
https://pubmed.ncbi.nlm.nih.gov/27437613/
Compression plating
Binod et al. Arch Orthop Trauma Surg 2016
- 35 tibial atrophic nonunion
- Judet's osteoperiosteal decortication and buttress bone plating
- 100% union
https://pubmed.ncbi.nlm.nih.gov/27317343/
Cancellous Bone grafting
Indications
- bone defect < 2cm
Options
- iliac crest
- reamer / irrigator / aspirator
Approaches
Anterolateral approach
- poor skin healing
- limited amount of bone graft
Posterolateral approach
- middle and distal thirds tibia
- patient prone or lateral
- incision medial to fibula
- between FHL and peroneal tendons
- elevate FHL and soleus taken off tibia
- debridement non union
- tissue sent for MCS
- recanalise medullary canal for blood supply
- create troughs in bone segment cortex with burr
- longitudinal troughs in cortex with burr to bleeding bone
- pack in BG, overlapping cortical bone by at least 1 cm
- apply bone graft
- close fascia over BG and drain
Posteromedial approach
- proximal tibia
Results
Foster et al. Injury 2017
- posterolateral bone grafting in 59 patients with distal 2/3 tibial nonunion
- 75% union rate
https://pubmed.ncbi.nlm.nih.gov/28736122/
Le Baron et al. Orthop Traumatol Surg Res 2019
- compared iliac crest bone graft v reamer/irrigator/aspirator (RIA)
- aseptic nonunion with bone defect < 2cm
- 90% union in both groups
- reduced operative time / analgesia requirements / inpatient stay with RIA
https://pubmed.ncbi.nlm.nih.gov/30885818/
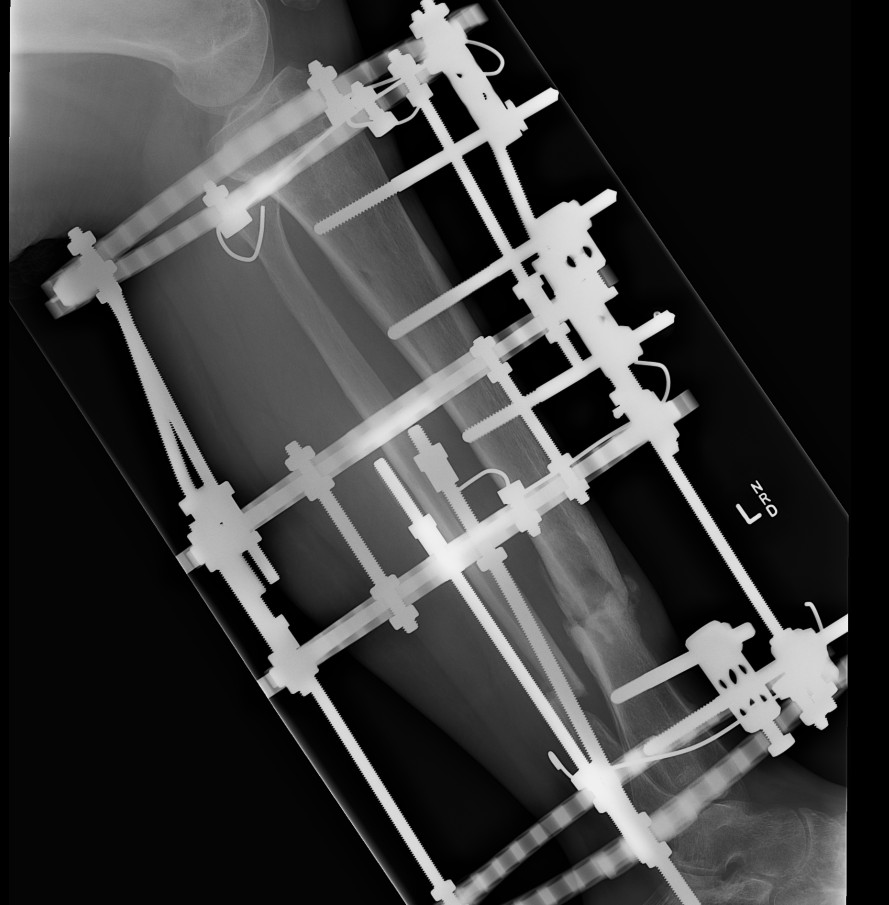
Ilizarov
Indication
- infection
- malunion
- acute shortening for skin loss
- bone transport for large segmental defects
Advantage
- allows compression
- allows immediate weight bearing
Adjuncts
Low intensity pulsed ultrasound
Hannemann et al. Arch Orthop Trauma Surg 2014
- may accelerate time to union in fractures treated without surgery
https://pubmed.ncbi.nlm.nih.gov/24895156/
Bone Morphogenic Protein
Govender et al JBJS Am 2002
- RCT of patients with open tibial fractures treated with IMN
- +/- addition of BMP 2 on absorbable collagen sponge at time of wound closure
- BMP group increased union rate and faster union
- BMP group had faster wound healing and fewer infections
https://pubmed.ncbi.nlm.nih.gov/12473698/
Mangement of Infected Nonunion
Options
Antiobiotic covered nail
Masquelet Technique
Coversion to external fixation
IM Abx covered rod
Technique
- remove IMN, ream and irrigate
- make Abx rod
- use chest tube with guide wire in it
- pour PMMA with Abx (3G vanco, 3G Fluclox)
- cut off plastic sleeve
- insert rod
- treat infection with 6/52 of appropriate Abx
- return at 6/52 for definitive management of non union (exchange nail / ilizarov)
Masquelet technique
See below for treatment of segmental bone defect
Use of first stage with antibiotic cement can help eradicate infection
Ilizarov Technique
Technique
- remove metal work / IMN
- take multiple cultures
- ream / rrrigate +++
- apply Ilizarov
- manage non union
Option 1
- fibular osteotomy
- acute compression over next 10 days
- wait bear as tolerated
- watch for union
Option 2
- excise dead bone / non union
- acutely shorten and compress distally
- proximal corticotomy and bone transport
Results
Yin et al PLoS One 2015
- systematic review infected nonunion of the tibia
- 97.5% union rate
https://pubmed.ncbi.nlm.nih.gov/26529606/
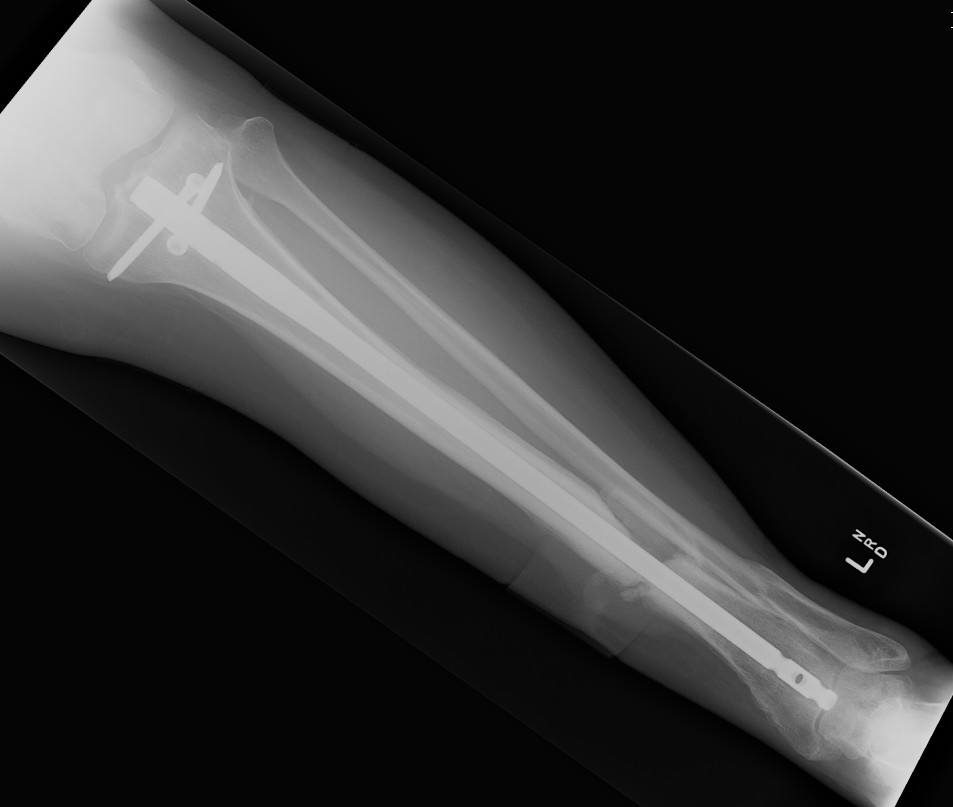
Case
12 months of persistant sinus drainage
- nail removed
- Ilizarov applied with fibular osteotomy and acute compression of non union
- 6/52 IV Abx


Segmental Bone Defects
Causes
- acute trauma
- resection of dead / contaminated bone
- resection infected bone
- resection infected non union
Options
1. Acute shortening < 1 cm
2. Autologous non-vascularised BG 1 - 3 cm
3. Masquelet
4. Bone transport distraction osteogenesis < 10 cm
5. Free vascularised fibula transfer < 12 cm
6. Bulk structural Allograft
7. Amputation
Acute shortening
Advantage
- allows healing to begin immediately
- improves stability
- relaxes soft tissues
- may allow primary closure
Disadvantage
- create LLD
- can address at later stage
Autologous bone grafting
As above for non union
Masquelet technique
Technique
- induced membrane technique
- two stage tecnique
- first stage is insertion of PMMA spacer in bone defect
- maintain stability i.e. external fixation
- induces a foreign body reaction with a thick vascularized membrane
- at 6 - 8 weeks perform second stage
- the membrane is opened and bone grafted
- stabilise with plate / nail / external fixation
Results
Morelli et al. Injury 2016
- systematic review
- union rate 90%
- eradication of infection 91%
https://pubmed.ncbi.nlm.nih.gov/28040090/
JBJS Surgical Technique
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6687485/pdf/jbjsest-9-e22.pdf
Bone Transport Distraction Osteogenesis
Technique
- proximal metaphyseal corticotomy
- 5 day latency period
- 1 mm/day distraction
- bridge diaphyseal segment
- bone graft docking site at second OT
- await consolidation (2 x transport times)
Free Vascularised Fibula Graft
Technique
- fibula segment 4cm longer than defect
- allows overlap 2 cm each end
- must leave 5 cm fibula distally, 7 cm fibula proximally
- vascular anastomosis performed
- secured with screws and protected by external fixator
Issues
- technically demanding
- bone needs to hypertrophy
- risk of fracture / non union
- donor site morbidity
Results
Feltri et al. Arch Orthop Trauma Surg 2021
- systematic review
- union rate 80%
- 40% rate of complications (fracture, nonunion, delayed union, infection, thrombosis)
https://pubmed.ncbi.nlm.nih.gov/34110477/
