Definition
Infection of bone 2° blood-borne bacteria
Epidemiology
Most common children
- peak 10 years
True haematogenous OM rare in adults
- usually involves spine
M: F 2:1
Site
Most common femur & tibia
- initially affects metaphysis
- distal femur
- proximal and distal tibia
Pathogenesis
1. Infants
Blood Supply
- metaphyseal blood vessels penetrate physis
- blood vessels expand into large venous lakes at epiphysis surface
- transphyseal blood vessels persist to 1 year
- then physis becomes a barrier
Infection
- infection frequently occurs at epiphysis & in joint
- i.e. hip joint
- joint damage / growth disturbance
- profuse involucrum common
- usually resolves completely due to rich periosteal BS
2. Children
Blood Supply
Nutrient artery supplies majority of metaphysis
- branch of nutrient artery reaches physis at right angle
- turn down in acute loops
- enter large venous lakes
Peripheral metaphysis / epiphysis have separate blood supply
Aetiology
A. Area of relative stasis near physis
- low oxygen tension
B. High amount of blood flow near physis
C. Trauma
- haematoma and oedema
Infection
Secondary thrombosis of nutrient artery
- periosteum lifts / cortex devascularised
A. Periosteum lays down involucrum
- periosteal new bone
- forms over cortex surrounding infected area
B. Cortical death / sequestrum
- entire cortex avascular
- inner 1/2 because of nutrient artery thrombosis
- outer 1/2 because of periosteal lifting
Epiphyseal involvement & joint infection rare
- growth disturbance rare
- increased blood flow to metaphysis may cause growth stimulation
3. Adults
Blood supply
After physeal closure, blood vessels again connect metaphysis and epiphysis
Infection
May occur in subarticular region & involve joint
Periosteal fibrosis / adhesion makes detachment by pus difficult
- prevents formation of subperiosteal abscess & preserves BS outer cortex
- thus large sequestra not formed
- hence infection spreads along shaft of bone
Aetiology
Secondary to bacteraemia
- history recent infection in 25%
Neonates
- E Coli
- Strep pyogenes
- Group B Strep
- S aureus
Children
- S aureus
- Hemophilus 18/12 - 3 years (unless immunised)
Adults
- S aureus
- G neg
Consider
- Gonnococcus (young adults)
- Salmonella (sickle cell)
- Pseudomonas (foot puncture)
- Fungal
Clinical Features
Child
- usually delayed presentation
- history of trauma
- complaining of limb pain
- become febrile / unwell
- tender metaphysis
- may be red / swollen
Neonate
- mildly febrile / unwell
- refusal to move limb
- red / swollen limb common
Bloods
ESR / CRP raised
WCC may be increased
Early blood culture before antibiotics
X-ray
Bony changes at 10 days
1. First feature is periosteal new bone
- later involucrum
2. Brodies abscess
- osteolytic metaphyseal lesion
- well defined cavity in cancellous bone
3. Garre's osteomyelitis
- sclerosis and thickening of cortical bone
- partial obliteration of medullary cavity
- often diaphyseal
- consider anaerobe Propionibacterium acnes

Bone Scan
Positive all 3 phases in 24 - 72 hours
- sensitivity & specificity 90%
US
Identify fluid in joint space which may be septic arthritis
CT
Sequestrum
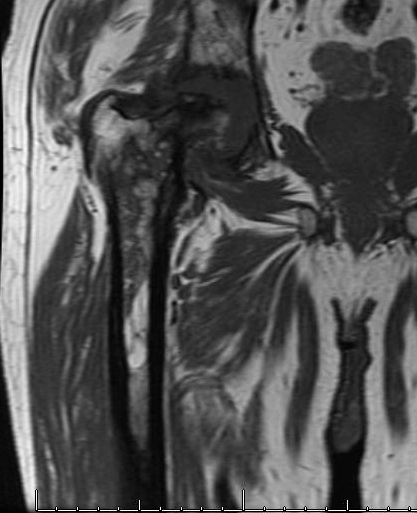
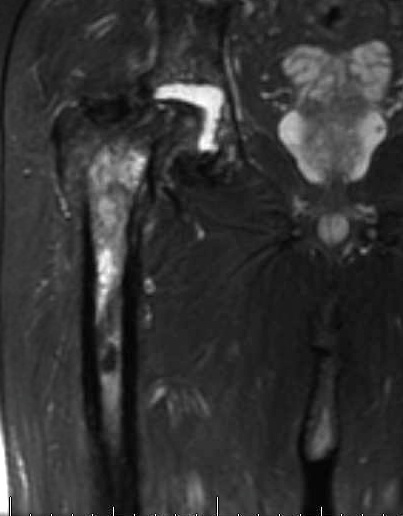
MRI
Increased signal on TI
Abscess
- high signal rim with low signal in middle
- rim / ring enhancement with gadolinium
Aspiration / Biopsy
Subperiosteal / intra-osseous
- positive culture in 60 - 90%
Management
Principles
1. Antibiotics most effective before pus forms
- don't delay administration
- low threshold
- i.e. child with leg pain and likely early OM
2. Antibiotics can't sterilise avascular tissues or pus
- these should be removed surgically
Antibiotics
80% will settle with antibiotics
Options
Flucloxacillin 25 - 50 mg/kg/dose q6h
Cephalothin 25 - 50 mg/kg/dose q6h
May be better to use broad spectrum
Route & Duration
Intravenous until child well, afebrile & non tender
- minimum 72 hours
- then convert to oral
- 24 weeks
- cease when CRP normal and child clinically well
Results
Peltola et al Pediatrics 1997
- 50 cases with change to oral at 4 days
- average duration 23 days
- effective treatment in all cases
Peltola et al Pediatr Infective Disease Journal 2010
- repeated same study
- same findings
Surgery
Indications
1. Abscess
2. Sequestrum
3. Severely ill patient
4. Poor response to antibiotics ~24hrs
5. Diagnosis in doubt
Procedure
- tourniquet
- incision over maximum tenderness
- release of pus in ST & under periosteum
- drill-holes in cortex if no subperiosteal pus found
- close skin over drain
Complications
Septic arthritis
- < 12/12 old (blood vessels cross physis)
- intra-articular metaphysis i.e. hip
Septicaemia
Premature physeal arrest
Pathological fracture
Chronic OM
Prognosis
Recurrence 4%
