Bone Healing
Bone healing requires 3 things
- osteoconduction - scaffold / matrix
- osteoinduction - growth factors
- osteogenesis - cells to produce osteoid
Osteoconduction
Definition
- property of a matrix that supports the attachment of bone forming cells for subsequent bone formation
Substances
1. Autograft
2. Allograft
3. Calcium phosphate
Osteoinduction
Definition
- process that supports the mitogenesis of undifferentiated mesenchymal cells
- osteoprogenitor cells to become osteoblasts
Substances
1. Autograft
2. BMP
- part of transforming growth factor (TGF) familty
- at least 15 types
- stimulate differentiation of mesenchymal cells
Osteogenetic properties
Definition
- generation of bone from bone forming cells
- require presence of osteogenetic cells / osteoblasts
Substances
1. Autograft
2. Autologous bone marrow
Autograft
Sources
Cancellous
- iliac crest
- proximal tibia
- distal radius
- PSIS
Structural
- iliac crest
- fibular / vascularised graft
Properties
- osteoconduction
- osteoinductive
- osteogenic
Autologous Bone Marrow Aspirate
Properties
- osteogenesis
- osteoinductive factors
Results
Hernigou et al JBJS Am 2005
- injected 20 mls into non infected NU site
- union in 53 of 60
- positive correlation of volume of mineralised callous and concentration of colony forming units
Allograft
Structural
Options
A. Fresh
- inadequate time for disease screening
- HIV / HCV / HBV testing mandatory on donors
B. Frozen
- stored at -60o
C. Freeze-drying
- destroys all osteogenic cells
- limited osteoinductive properties
D. Irradiated
- for sterility
- gamma irradiation (affects mechanical properties)
- ethylene oxide (affects osteoinductive properties)
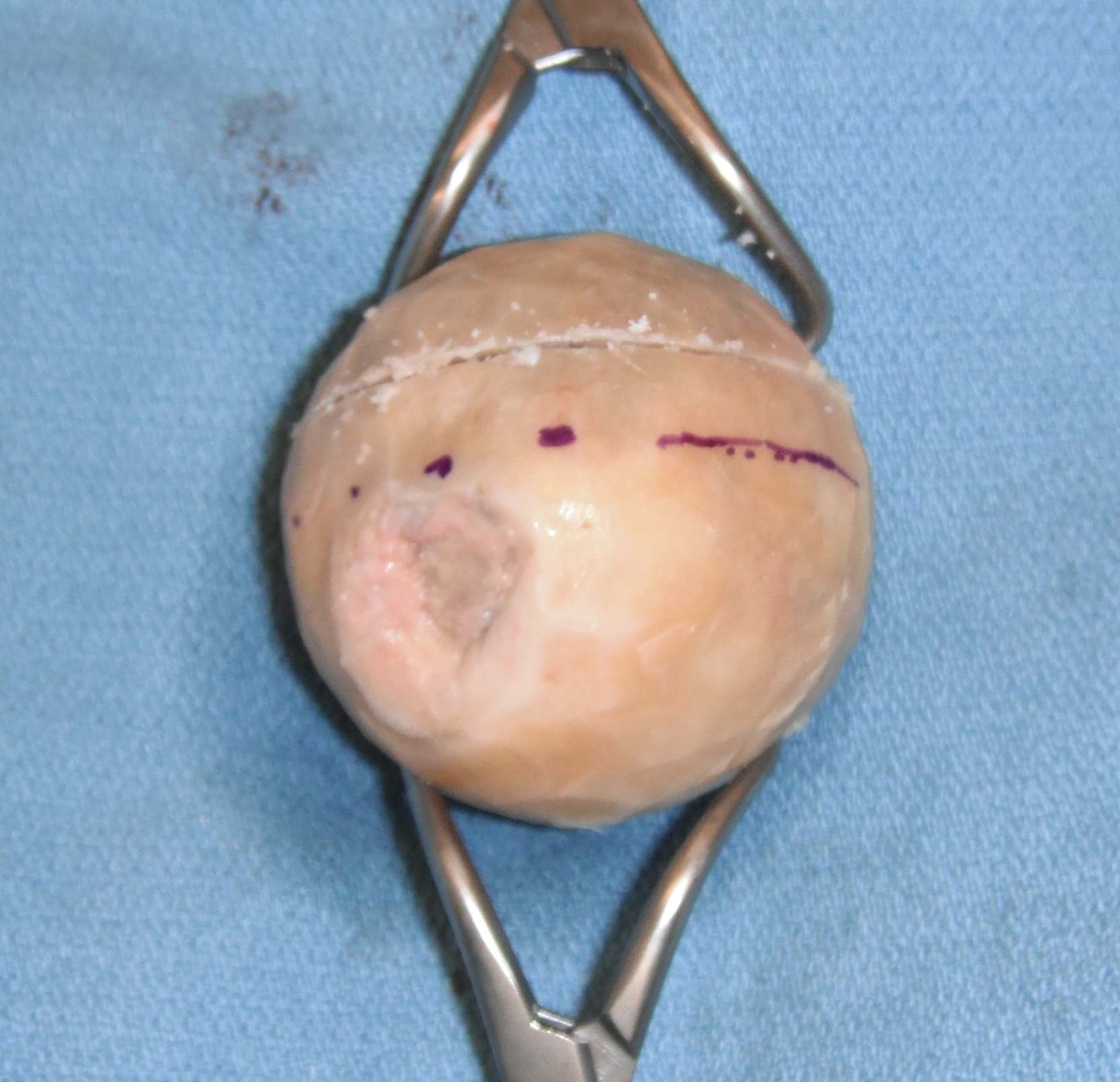
Properties
Osteoconductive
Types
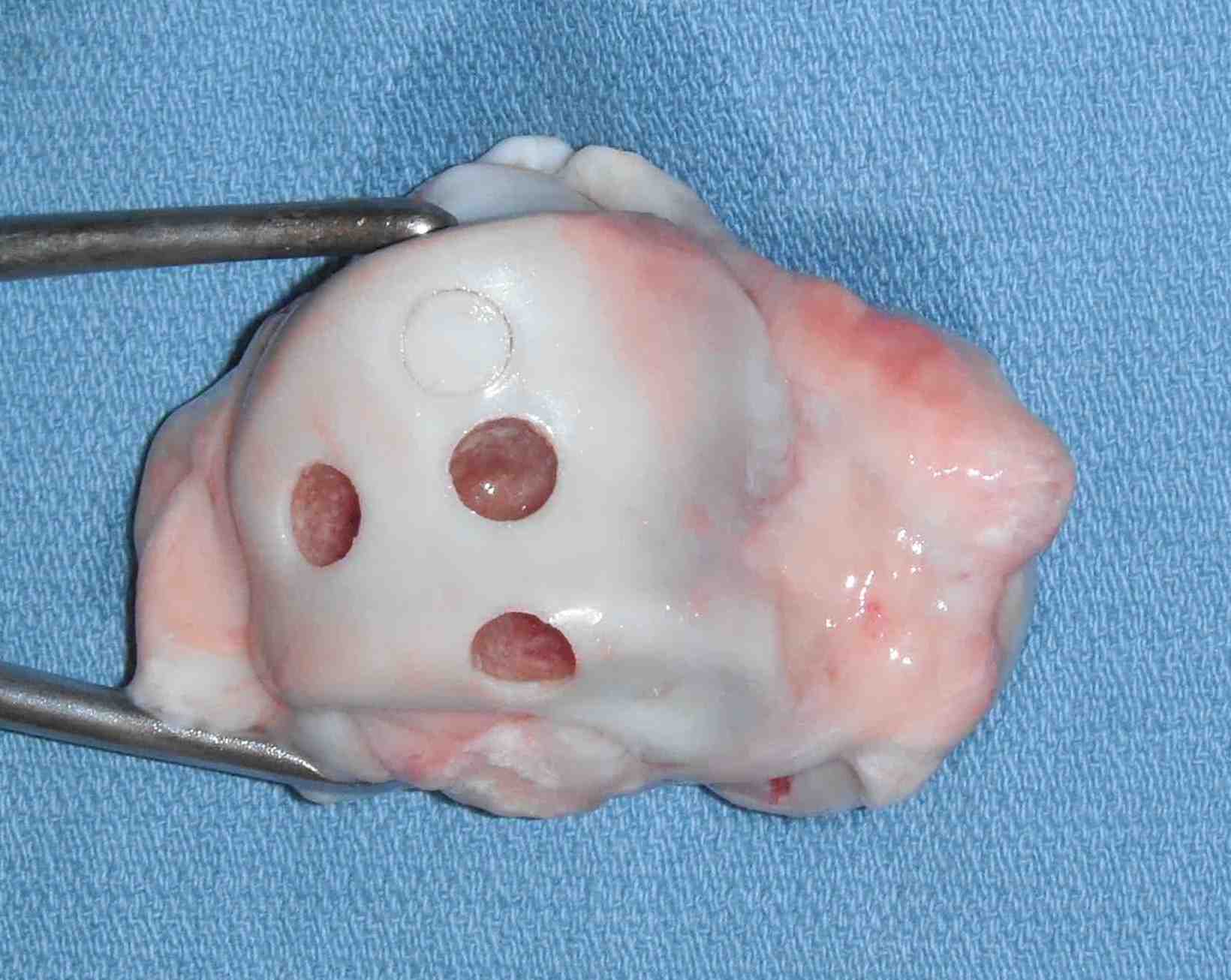
Cortical strut grafts
- used in periprosthetic THR fractures
- creeping substitution via intra-membranous bone formation

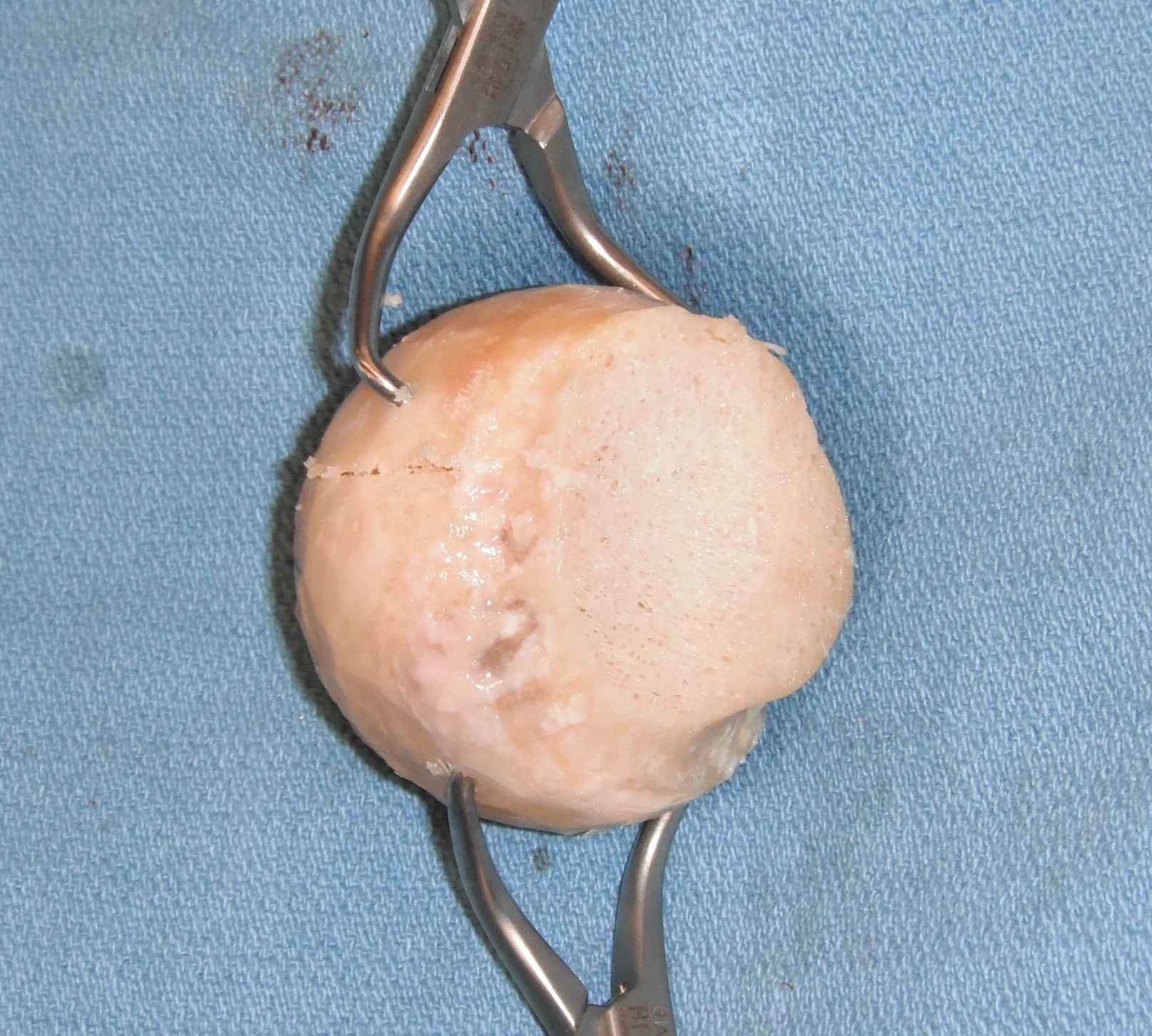
Cancellous allograft chips
- osteochondral ossification
Disadvantages
Osteointegration is invariably
- incomplete
- much slower than autograft
Results
Gibson et al Spine 2002
- RCT of fresh frozen morcellised allograft v autograft in PLF
- comparable results
2. Demineralised Bone Matrix / DBM
Concept
Produced by acid extraction of allograft
- retention of collagen and growth factors
- no structural strength
- osteoinductive
- comes as putty or gel
- used in spinal surgery
Results
Lindsay et al Orthopedics 2006
- compared DMB + BM aspirate to autograft in long bone fractures
- comparable findings in regards to union
Vaccaro et al Orthopedics 2007
- prospective study of DMB v autograft in posterolateral spinal fusion
- comparable findings
Synthetic Grafts
Calcium Phosphate Synthetic Substitutes
Properties
- osteoconductive
- provide scaffold
- allow host osteogenic cells to create bone under the influence of host osteoinductive factors
Structure
Ceramics
- highly crystalline structures
- obtained by sintering (heating > 1000o)
- pore size and porosity important
- osteoid formation requires minimum pore size of 100 microns (preferably 300 – 500)
A. Tricalcium phosphate / Chronos
- formed by treating coral with ammonium
- similar structure and porosity to cancellous bone
B. Synthetic hydroxyapatite / Pro Osteon
- may have some osteoinduction properties
- slower in vivo resorption than tricalcium phosphate
- higher brittleness
C. Cements/ Norian
Indications
Metaphyseal defects
- calcaneum
- tibial plateau
- distal radius
Resorption
80% at 10 weeks
- can continue for as long as 30 weeks
- dissolution + osteoclast resorption
Results
Russell et al JBJS Am 2008
- RCT of autograft v calcium phosphate cement in tibial plateau fractures
- significantly reduced rates of subsidence
Buckley et al J Trauma 2009
- RCT of autograft v calcium phosphate past in displaced IA calcaneal fractures
- significantly reduced rate of articular depression
Calcium Sulfate Synthetic Graft
Plaster of paris
- calcium sulfate + water
- forms dihydrate known as gypsum
Properties
- ? osteconductive
- may resorb too rapidly
- takes 4 – 12 weeks depending on size of defect
- low mechanical strength
Indications
- bone graft extender
Types
- MIG
- Osteoset
Results
Niu Spine 2009
- RCT of autograft + BMA v calcium sulphate + BMA in PLF
- significantly reduced rates of union in calcium sulphate group
BMP
Bone Morphogenic Protein
Background
Group of growth factors / cytokines
- 20 different types
- a type of transforming growth factor
- interact with receptors on the cell surface
Production
- initially extracted from demineralised bone graft by Urist in 1965
- demonstrated ability to stimulate bone growth in rabbits
- now produced by recombinant technologies
Types
Infuse (BMP-2)
OP1 (BMP-7)
Usually delivered on a collagen matrix
Uses
Spinal fusion
Non union long bones
Tibial Results
Friedlaender et al JBJS Am 2001
- As efficacious as autograft in established tibial non union
Govender et al JBJS Am 2002
- RCT of control v BMP in open tibial fractures
– less secondary interventions, accelerated time to union, reduced infection rates
Jones et al JBJS Am 2006
- RCT allograft + BMP2 v autograft in tibial diaphyseal cortical defects
- similar rates of healing, reduced blood loss in BMP group
Spine Results
Vaccaro et al Spine 2008
- RCT OP1 v autograft in PLF spine
- as least as efficious as autograft
Dimar et al Spine 2006
- RCT of iliac crest autograft v rhBMP2 on a collagen matrix
- reduced surgical time, bleeding and increased fusion rates with BMP
