Complications
Subscapularis failure
Rotator cuff failure
Instability
Infection
Periprosthetic fracture
Aseptic loosening
Neurological injury
Incidence
Parada et al. J Should Elbow Surg 2021
- 2224 aTSA complication rate 11%, revision rate 5.6%
- 3% cuff failure, 2.5% aseptic glenoid loosening, 1.3% infection rate
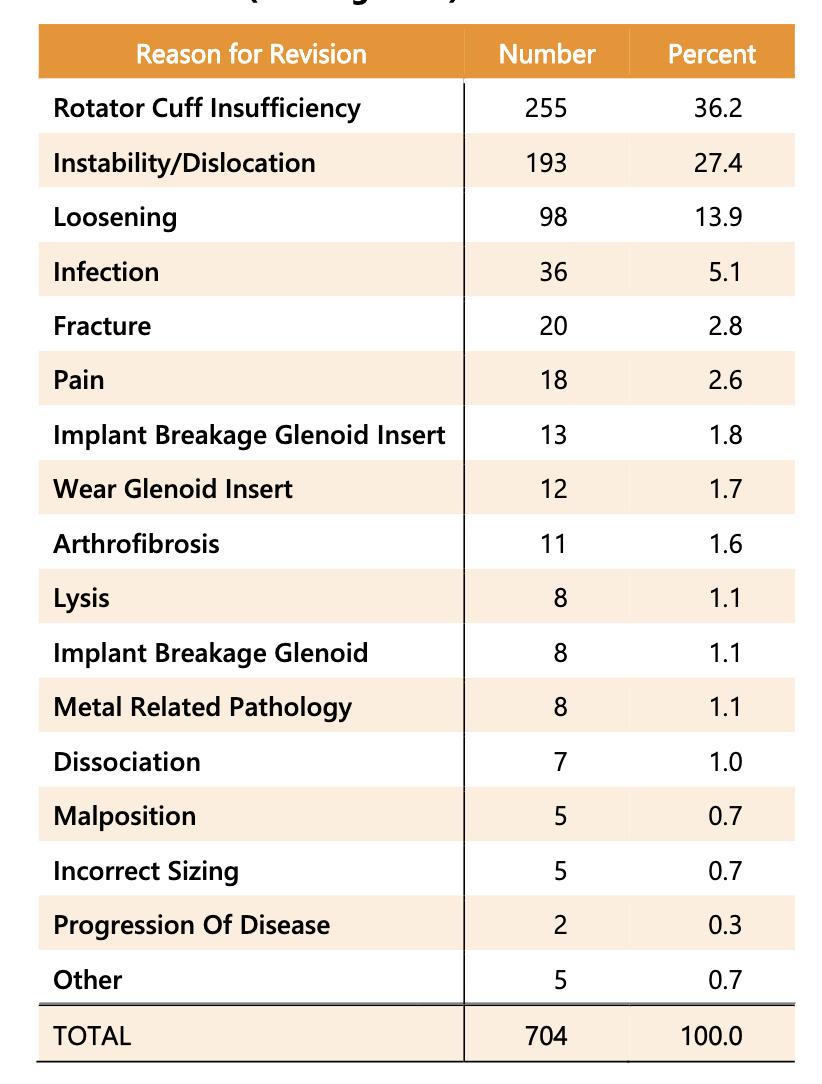
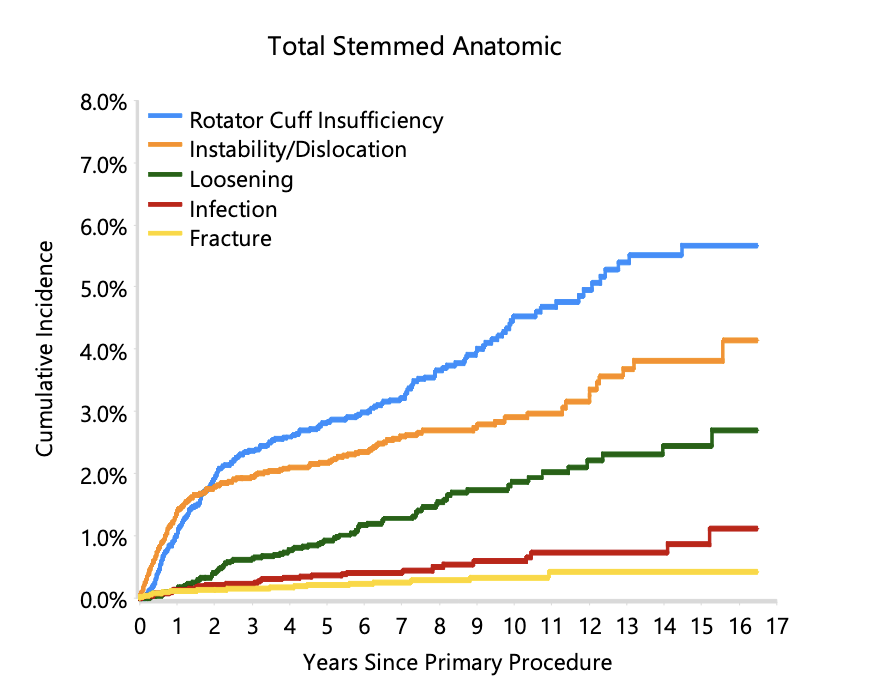
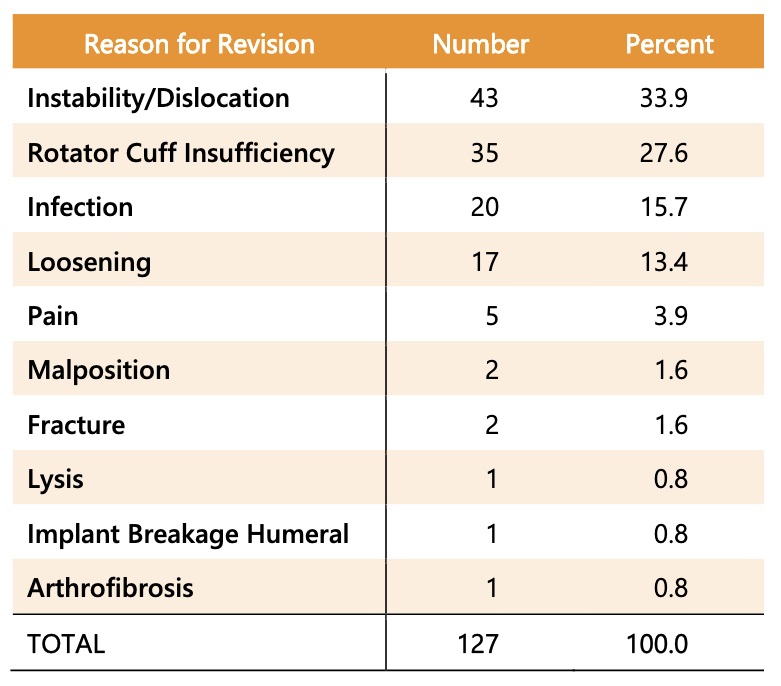
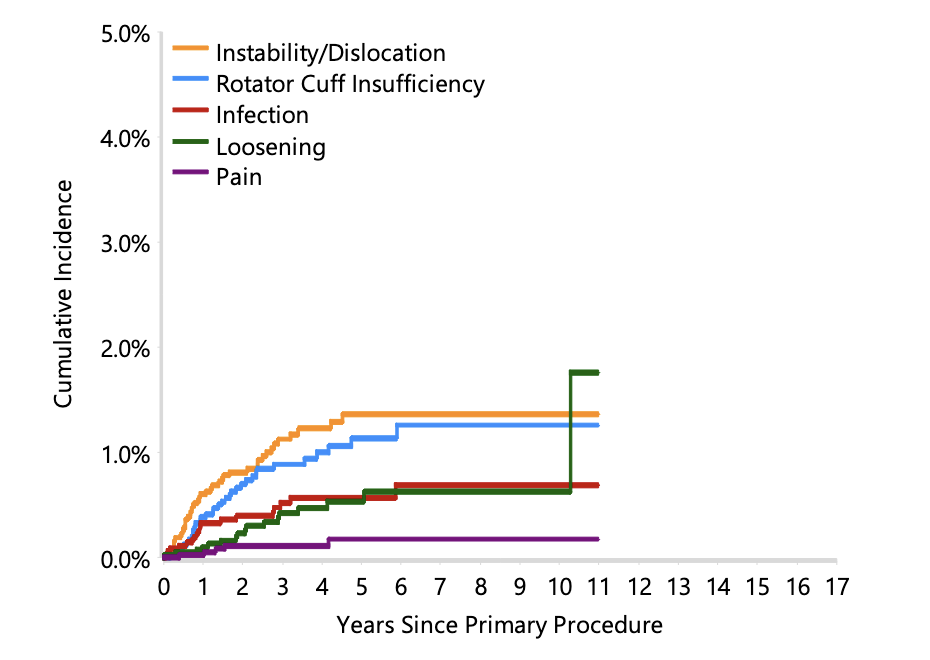
Australian Joint Registry 2024
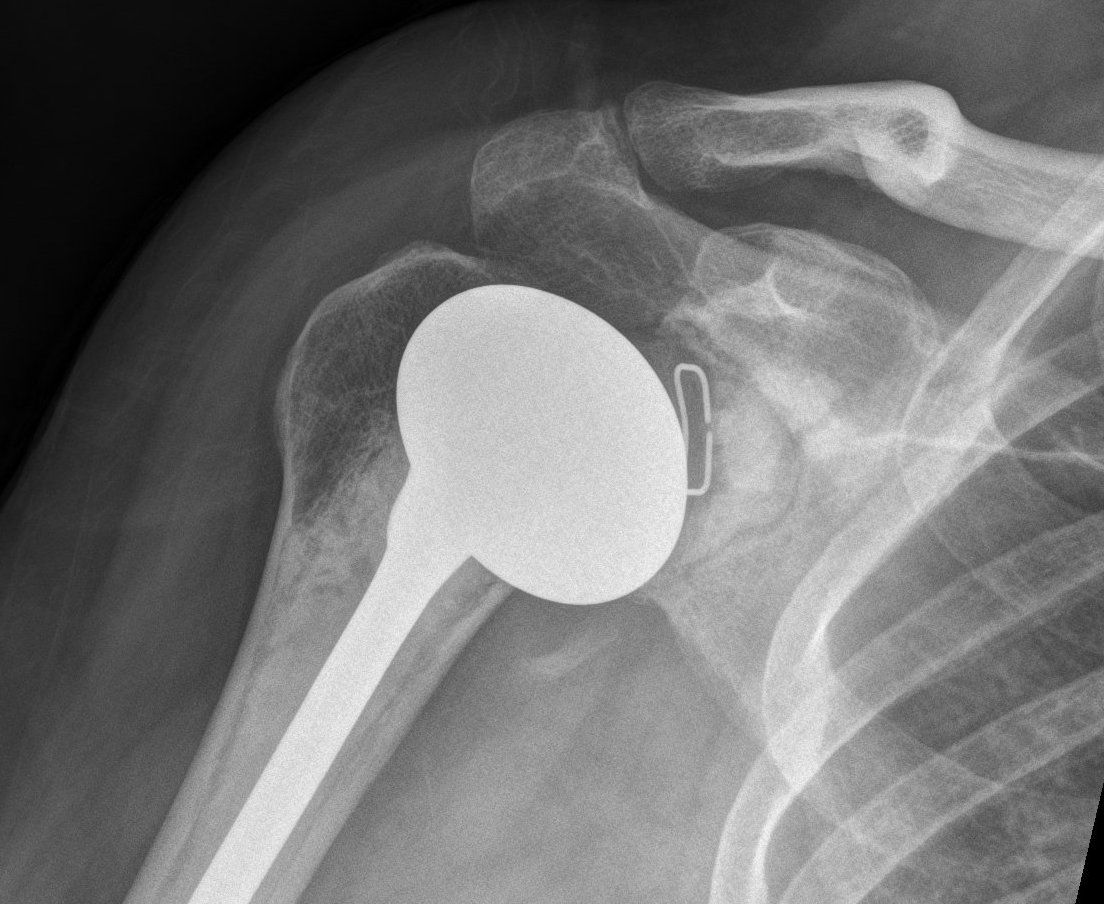
Stemmed aTSA
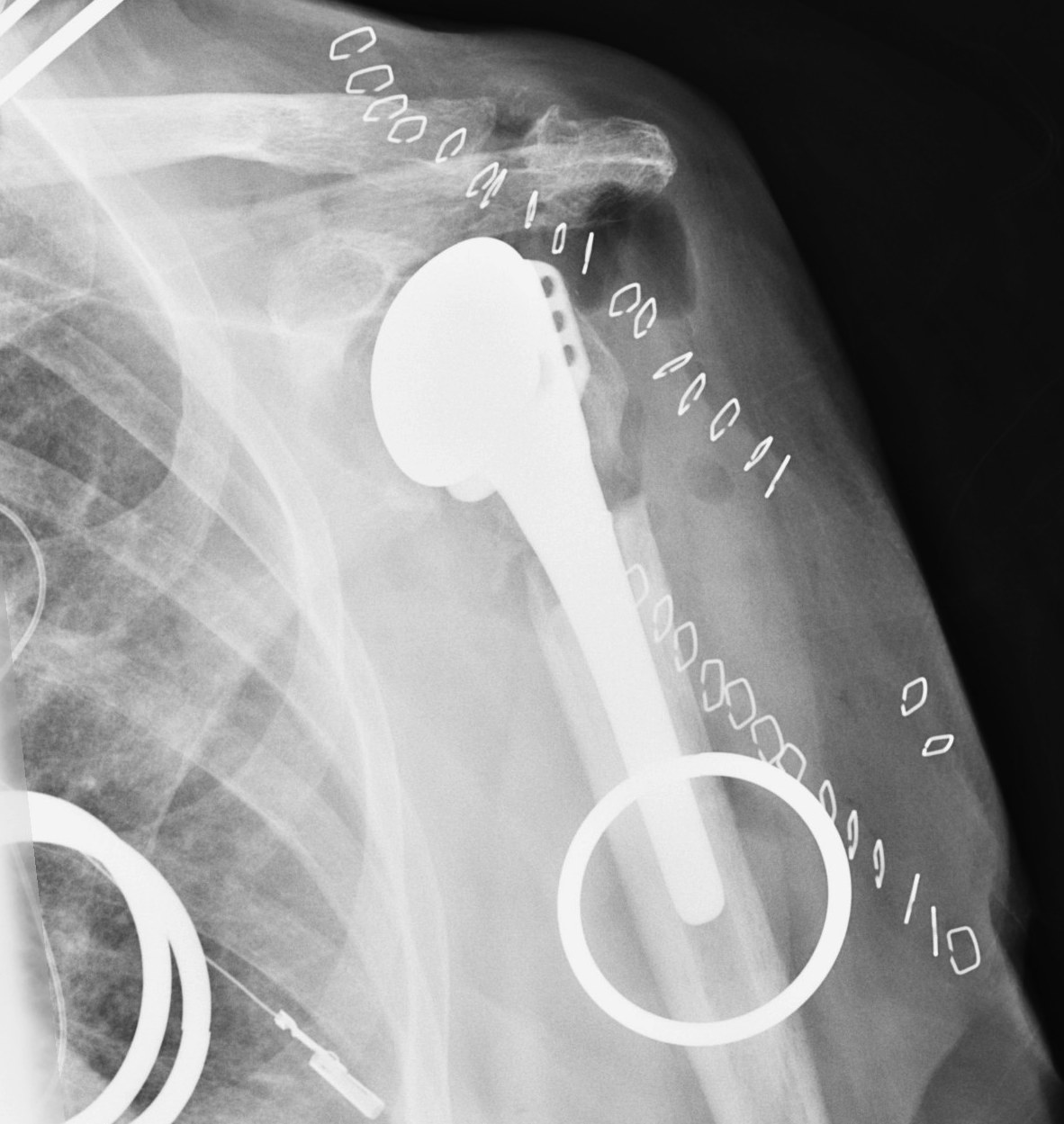
Stemless aTSA
Subscapularis Failure
Causes
Failure of repair
Acute trauma
Overstuffing
Humeral anteversion / anterior offset
Denervation
Incidence
Levy et al. Int J Shoulder Surg 2016
- systematic review of the incidence of subscapularis retears after aTSA
- incidence 3%
- reoperation rate 0.6%
Diagnosis
Often asymptomatic
May complain of pain / weakness / dysfunction
May have anterior instability
- 13% incidence of subscapularis retear on ultrasound
- majority asymptomatic
Options
1. Re-repair
2. Pectoralis major transfer
3. Allograft reconstruction
4. Reverse TSA
- 25 patients with failed subscapularis after aTSA
- 36% reported injury, remainder insidious onset
- 17 underwent repair with 52% reoperation rate
- 8 underwent revision to rTSA with no revisions
- pectoralis major transfer for failed subscapularis after aTSA
- 7/8 failed
- failure associated with anterior subluxation of the humeral head
Superior rotator cuff failure
Cause
Humerus overstuffing
Glenoid superior tilting
Failed rotator cuff repair

Prevention
Must ensure don't leave humeral head proud
- restore Shenton's line
Issue
Results in eccentric loading of the superior aspect of glenoid component & loosening
- "rocking horse glenoid"
Diagnosis
Superior migration of humeral head on xray
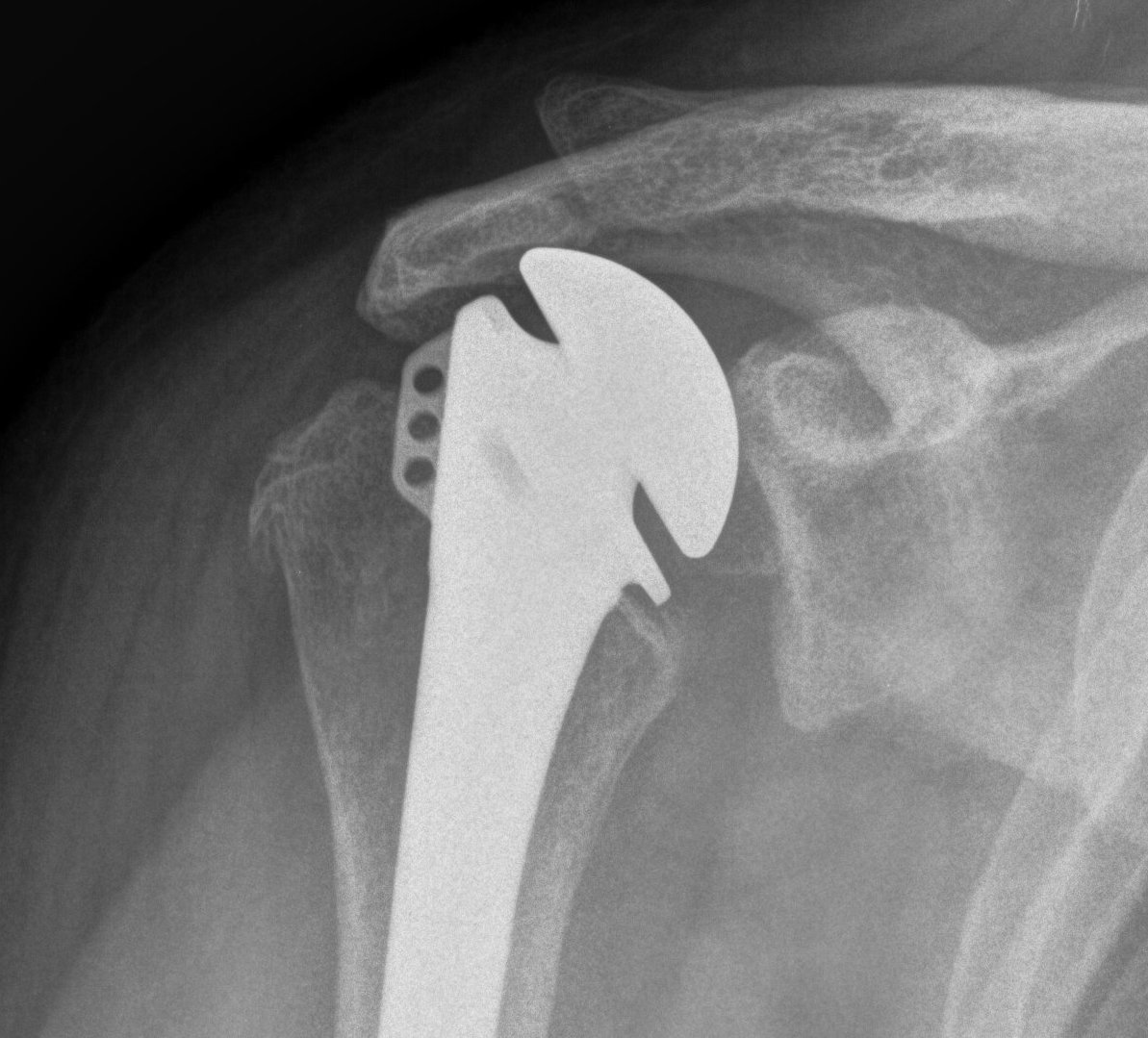


Incidence
- 5 year follow up of 518 aTSA
- incidence of cuff failure of 17%
Options

Revision to reverse TSA
- revision for cuff failure to rTSA compared to primary rTSA
- increased complications and worse patient outcomes in the revision group
Instability
Anterior
Cause
- mal-rotation humeral component
- subscapularis rupture
- anterior deltoid dysfunction
- glenoid component loosening
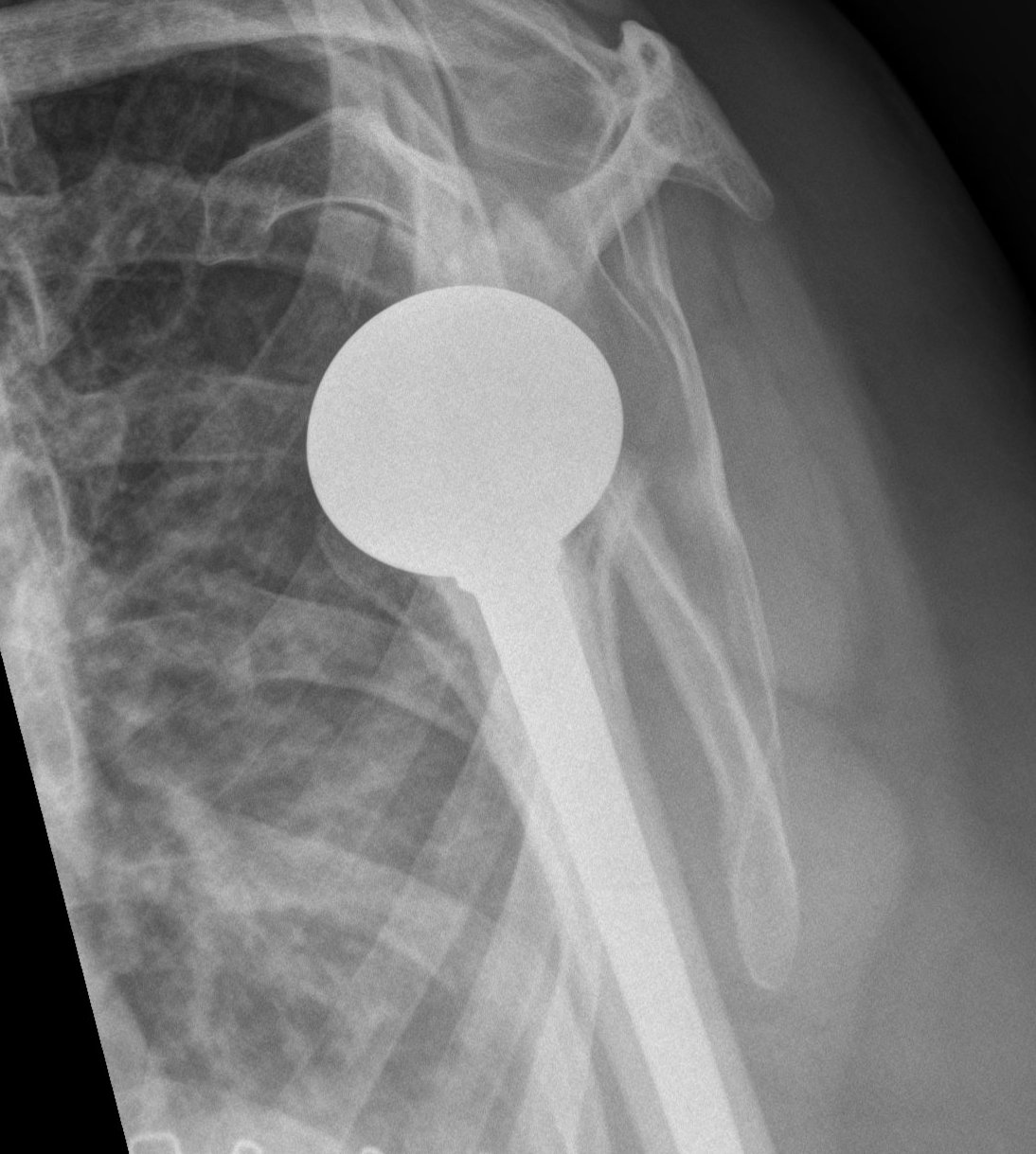
Posterior
Cause
- excess retroversion of glenoid or humerus
- posterior glenoid erosion
- soft tissue imbalance

Inferior
Post fracture with shortening of humerus
- important to re-establish humeral length to restore resting tension of cuff & deltoid
Management
- 27 cases of postoperative instability following aTSA
- 10 subscapularis tears, 6 massive rotator cuff tears, 8 component malposition, 2 component loosening, 1 humeral shortening
- patients undergoing revision to rTSA did better than those undergoing other procedures
- other procedures included component revision, bone blocks, or subscapularis repairs
Abdel et al. Bone Joint Journal 2013
- 33 unstable aTSA revised to rTSA
- 31/33 (94%) stable at final follow up
- 30% of patients unsatisfied
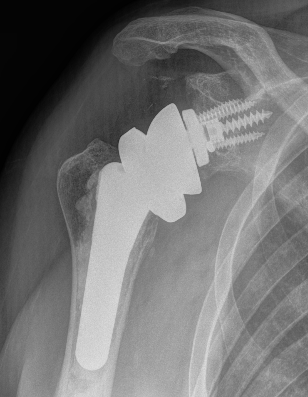
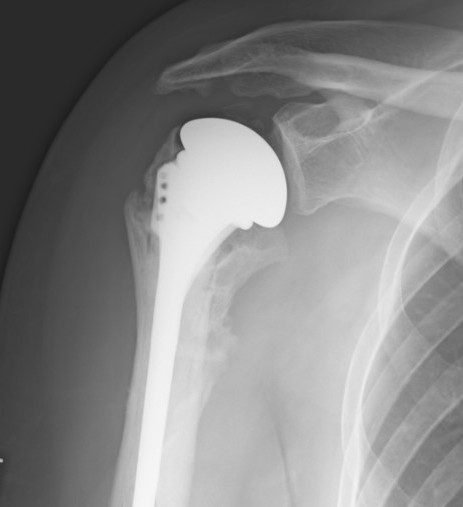
Aseptic loosening




Incidence
- 492 aTSA at 5 year follow up
- 308 (63%) had no radiolucent lines
- 184 (37%) had peri-glenoid lucency
- those with glenoid lucency had decreased ROM and patient-reported outcomes
- 37 patients with loose glenoids revised to rTSA
- all had glenoid bone deficiency
- 29/37 required bone grafting
- 8/37 (21%) required reoperation - glenoid loose (3) / anterior instability (3) / humeral subsidence (2)
Infection
Microbes
Propionibacterium acnes renamed Cutibacterium acnes
- gram postive anaerobe
- commensal skin flora
- 193 revision arthroplasties performed for pain, loosening or stiffness
- Propionibacterium acnes / Cutibacterium acnes cultured in 70%
Brown et al. Shoulder Elbow 2020
- P acnes, Staph aureus, coag negative Staph, and Staph epidermidis commonest
Diagnosis
Symptoms such as fever and redness often absent
Low virulence organisms such as P acnes and S epidermidis
Musculoskeletal Infection Society
Four of the following six criteria
1. Elevated ESR or CRP
2. Elevated synovial WBC count
3. Elevated synovial neutrophil percentage
4. Pus in the joint
5. Isolated of a microbe in one culture
6. Greater than 5 neutrophils per high power field in 5 fields at x400
Prevention
- RCT of 140 patients with the addition of 3% hydrogen peroxide to skin preparation
- positive skin culture C. acnes 17% hydrogen peroxide group versus 34% traditional preparation
- spacer, six weeks antibiotics, negative aspirate
- RCT of 56 patients with the addition of preoperative IV doxycycline
- no difference in intra-operative culture rate
Revision options
Options
Single stage revision
Two-stage revision
Resection arthroplasty
Permanent spacer
Cement spacer Resection arthroplasty
Two stage technique article
Brown et al. Shoulder Elbow 2020


Results
- insertion of gentamycin / vancomycin spacer in 38 patients
- IV Abx for 2 weeks then oral antibiotics for 10 weeks
- revision to rTSA or hemiarthroplasty if glenoid deficient
- 14 / 38 spacer left in situ
- 36 / 38 (95%) had successful infection control
George et al. BMC Musculoskeletal 2016
- systematic review of cure rates
- resection arthroplasty 87%
- single stage revision 95%
- two stage revision 91%
- permanent spacer 96%
- not statistically significant
- systematic review of resection arthroplasty v permanent spacer for salvage
- resection 82% infection eradication
- permanent spacer 85% infection eradication
- improved clinical outcomes with spacer
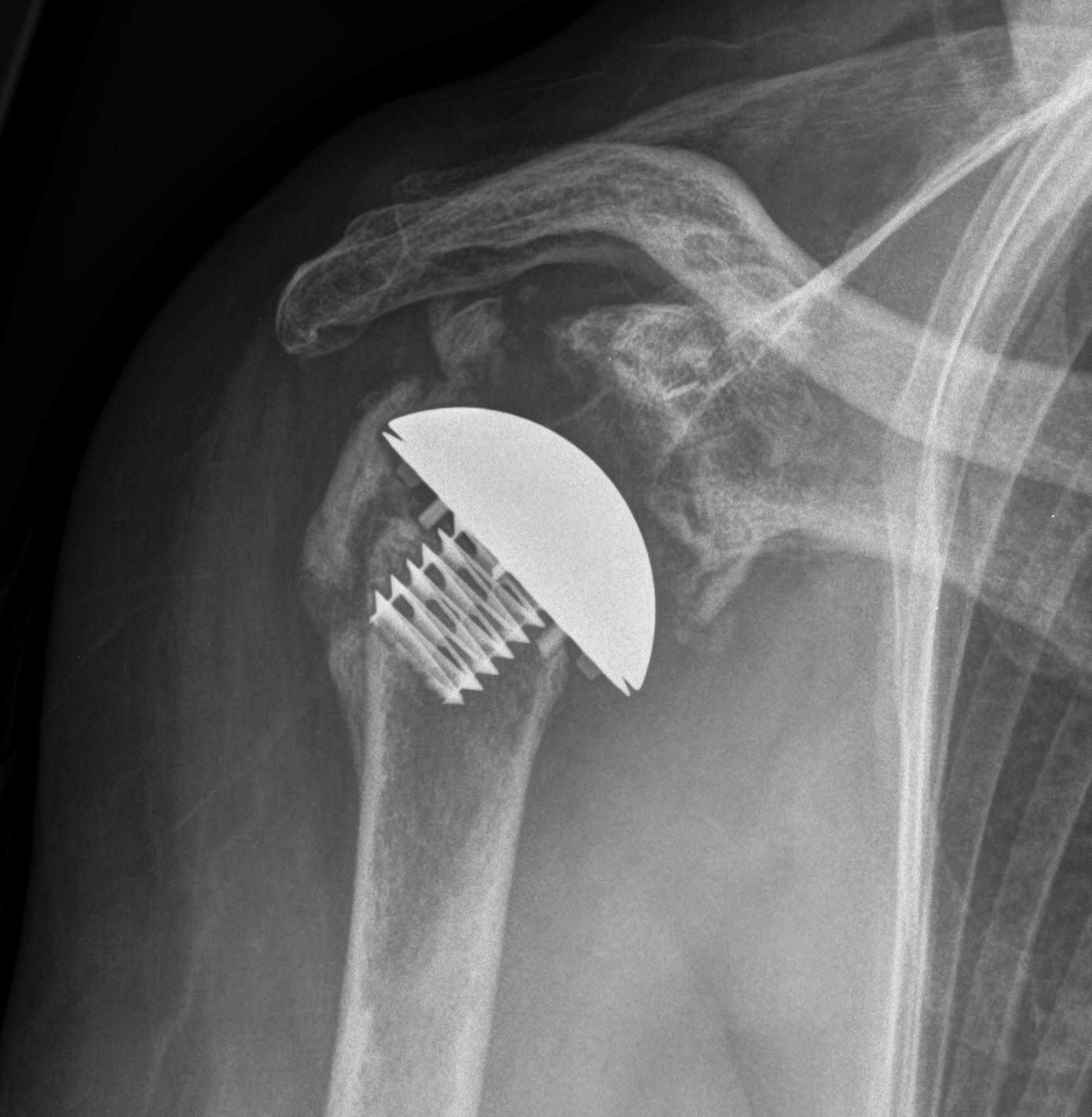
Intra-operative fracture
- 45 intra-operative fractures
- increased risk with press fit (1.7%) versus cemented (0.6%) humeral components
- increased risk with revision (3.3%) versus primary (1.2%) arthroplasty
- all united at a mean of 17 weeks


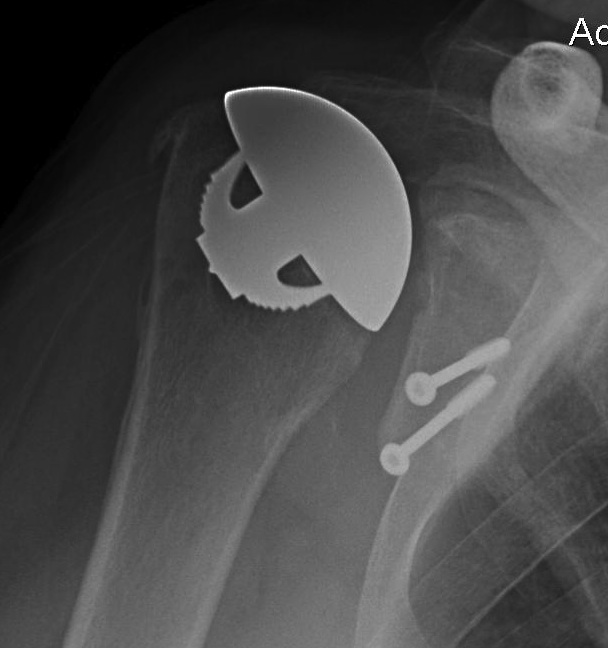
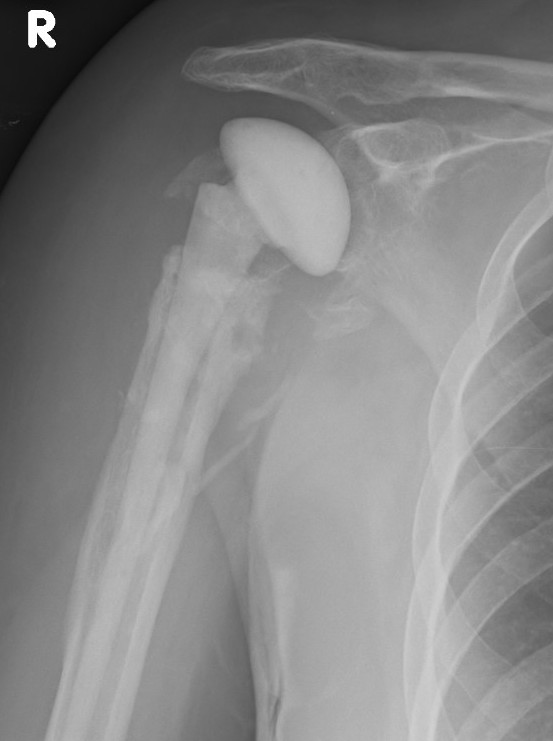
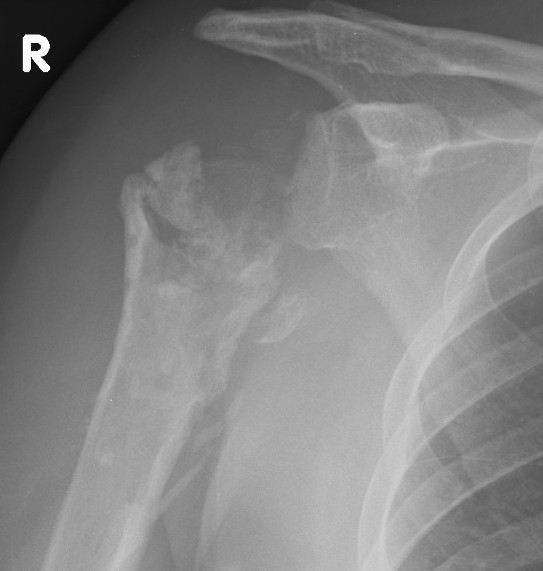
Peri-prosthetic Fracture
Cause
1. Trauma
2. Atraumatic - stress riser / loosening
Wright and Cofield Classification
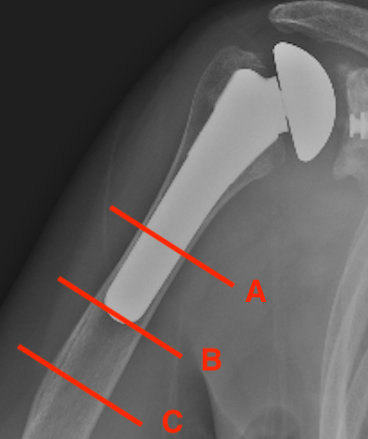
A: Fracture centred at the tip and extends proximally greater than 1/3
B: Fracture at tip only
C: Fracture distal to tip of the prosthesis and extends into distal metaphysis
Options Humeral Shaft Fracture
A. Non operative Management
- well-fixed prosthesis
- acceptable alignment


B. ORIF
- displaced tuberosity fractures
- well-fixed prosthesis and fracture distal to prosthesis
Anterolateral approach and plate
C. Revision
- loose humeral prosthesis / osteolysis
Long stem > 2 cortical diameters past fracture



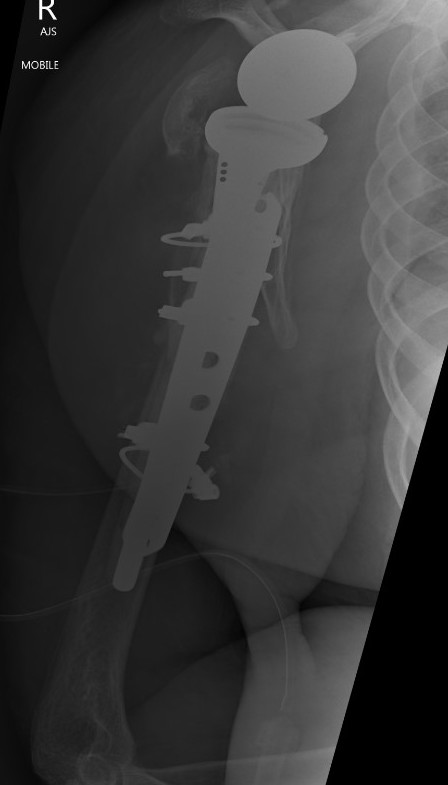
Results
- 11 / 16 patients with periprosthetic humeral fractures treated nonoperatively
- 6 healed after 180 days of non operative treatment
- 5 required operation after 123 days for non union
- recommended all fractures can be treated nonoperatively if well aligned and prosthesis stable
- if not united by 3 months, recommend intervention
Neurovascular injury
Incidence
Florcynski et al. JBJS Am 2021
- incidence of clinically apparent nerve injury after aTSA is 0.63%
Dangers
Musculocutaneous nerve
Axillary nerve
Brachial plexus
1. Musculocutaneous nerve
Branch lateral cord
- penetrates coracobrachialis 2-8 cm distal to coracoid
- palpate MCN under conjoint tendon
- place finger under tendon and sweep downwards to palpate
Most common cause of damage is overzealous retraction
2. Axillary nerve
Terminal branch of posterior cord
- arises inferior to coracoid
- crosses anteroinferior border of subscapularis muscle
- exits quadrangular space with posterior circumflex humeral artery
Palpate
- slide finger downwards over SSC muscle
- hook finger to feel nerve
- relatively tight cord running posteriorly
- relatively protected with adduction & ER
Quadrangular space
- below subscapularis anteriorly
- between Teres minor and Teres major posteriorly
- between long head triceps medially and humerus laterally
- contents: axillary nerve and the posterior circumflex humeral artery
Splits into 2 trunks
1. Posterior to teres minor & posterior deltoid
- terminates as superior lateral cutaneous nerve
2. Anterior passes to middle then anterior deltoid
Brachial Plexus
Diffuse injuries
Mixed picture
Thought to be secondary to stretch / traction
Heterotopic Ossification
