


Definition
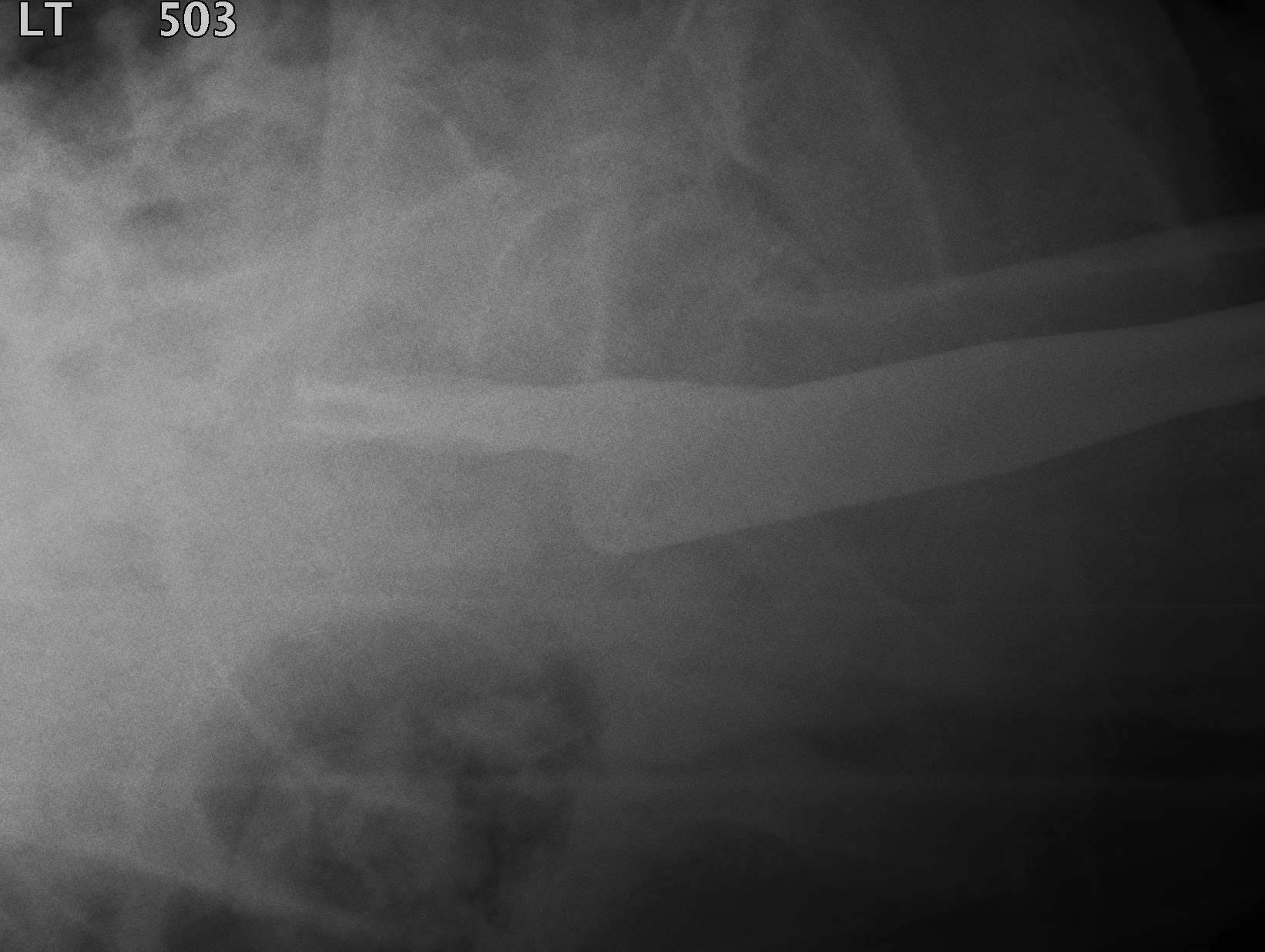
Fracture which extends between the trochanters of the proximal femur
Extra capsular / well vascularized
Epidemiology
50% of hip fractures
- elderly
- osteoporotic
- female
Signs
Leg
- shortened
- externally rotated
- groin pain with leg movement
Evans Classification
Two main types
- Type 1 Intertrochanteric
- Type 2 Reverse Oblique
Type 1 Intertrochanteric
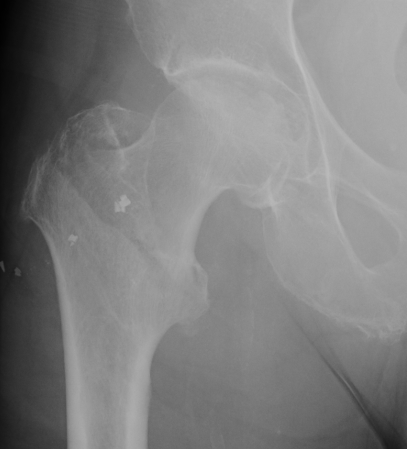
2 part undisplaced


2 part displaced

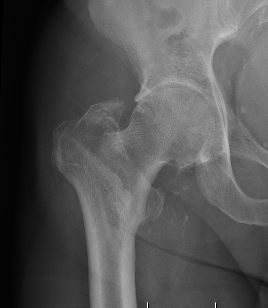
3 part without posterolateral support (GT fracture)

3 part without posteromedial support (LT fracture)


4 part without posterolateral or posteromedial support
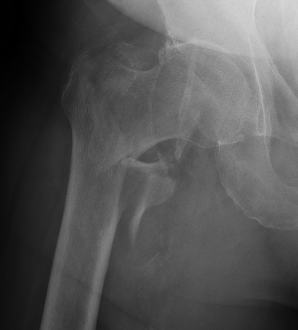
Type II Reverse Oblique Type
Inherently unstable - tendency of femoral shaft fragment to shift medially

Reverse oblique fractures
Stability
Depends on medial cortical reduction
Unstable (AO 31.A2 + 31.A3)
- intact lateral wall
- posteromedial cortical fracture
- reverse oblique
- subtrochanteric extension
Isolated GT Fracture

Management
Non operative
Indications
Unfit for surgery
- high risk of DVT / PE
- pressure ulcers
- pain with nursing
Operative
Goal
Obtain stable fixation
Early mobilisation
Timing
Welford et al Bone Joint J 2021
- systematic review of 46 studies and 500,000 hip fractures
- surgery < 24 hours reduces mortality
Leer-Salveson et al Bone Joint J 2019
- Norwegian registry of 80,000 hip fractures
- no change in mortality (3 day, 1 year) if surgery < 48 hours
Workup
Griffiths et al Anaesthesia 2021
- PDF for guidelines for the management of hip fractures
Issues
- consent
- do not resuscitate
- preoperative hemoglobin
- anti-platelet / anticoagulation
- GA versus spinal
Options


Sliding hip screw/dynamic hip screw
Cephalomdeullary nail
- Short / long
- one screw / two screws / blade
Fixed angle plate
Arthroplasty
- Calcar replacing prosthesis
Results
DHS versus nail
Depends on stability
Requires intact lateral wall for DHS (or GT plate)
- post-operative fracture of lateral wall turns stable intertroch into unstable
- Norwegian hip registry review of 17341 patients
- DHS vs nail for unstable intertrochs (A1/2/3)
- Nails have lower re-operation, and lower mortality rate
- meta-analysis of 22 studies and 3000 patients including all types of extracapsular proximal femur fractures
- DHS v cephalomedullary nail
- no difference in mortality / reoperation / failure fixation / complications
- IMN had shorter operative times and reduced blood loss
- Did no delineate between fracture patterns
Single versus dual screws


Yang et al J Orthop Surg Res 2023
- systematic review of single versus dual screw cephalomedullary nail
- 23 studies and 3500 surgeries
- dual screw reduced risk of failure and reoperation
Nail with helical blade vs screw
Kim et al, J Orthop Trauma 2021
- systematic review of 2331 femoral nails
- TFNA neck screw vs helical blade
- helical blade more likely to fail compared to screw (OR 5.33)
- non-union rate same
Long vs short nail
Cinque et al, Arch Orthop Trauma Surg. 2022
- meta-analysis of 3208 intertrochs
- long vs short nail
- short nails had less blood loss, and operative time
- no difference in re-operation, failure, or transfusion rates
ORIF versus hemiarthroplasty
Hongku et al Orthop Traumatol Surg Res 2022
- systematic review of 7 RCTs and 500 patients
- higher operative failure with DHS / PFN compared with hemiarthroplasty
- higher long term hip scores with PFN
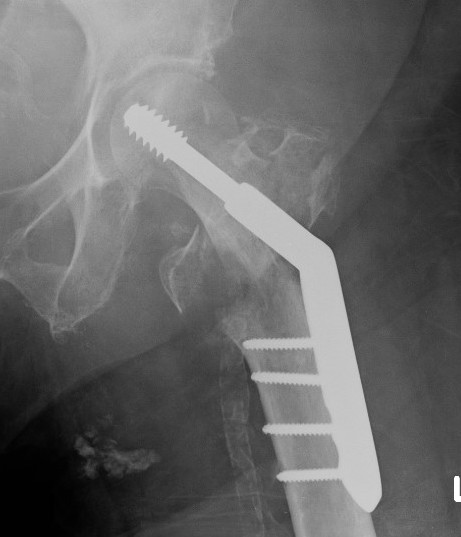
Dynamic hip screw


Mechanism
Plate is a lateral tension band whilst the sliding screw allows controlled fracture impaction
Technique
Youtube step by step sawbone guide
Set up
- traction table with anatomic reduction
- traction, adduction, internal rotation
Lateral approach to femur
- elevate vastus lateralis and control bleeding from perforators
Guide wire
- centred in femoral head in 2 planes
- tip-apex distance < 25 mm
Tip - apex distance
- from tip of screw to apex femoral head
- accumulative on AP and lateral
- > 25 mm, increases cut out
Measure angle
- wire in centre of neck / centre of head
- usually 130o prosthesis
Ream to within 5 mm of end of wire
- tap
- insert screw / tip apex distance < 25 mm
- attach plate
Options for improving stability
a. Valgus Osteotomy for unstable Fractures
Theory
- reduces shear force
- increases compression
- stronger construct
Technique
- 135° plate placed in at 120°
- valgises proximal fragment and medializes shaft
- +/- lateral wedge removed / sarmiento valgus osteotomy
b. Trochanteric stabilization plate
Theory
- buttresses the GT and prevents lateral displacement
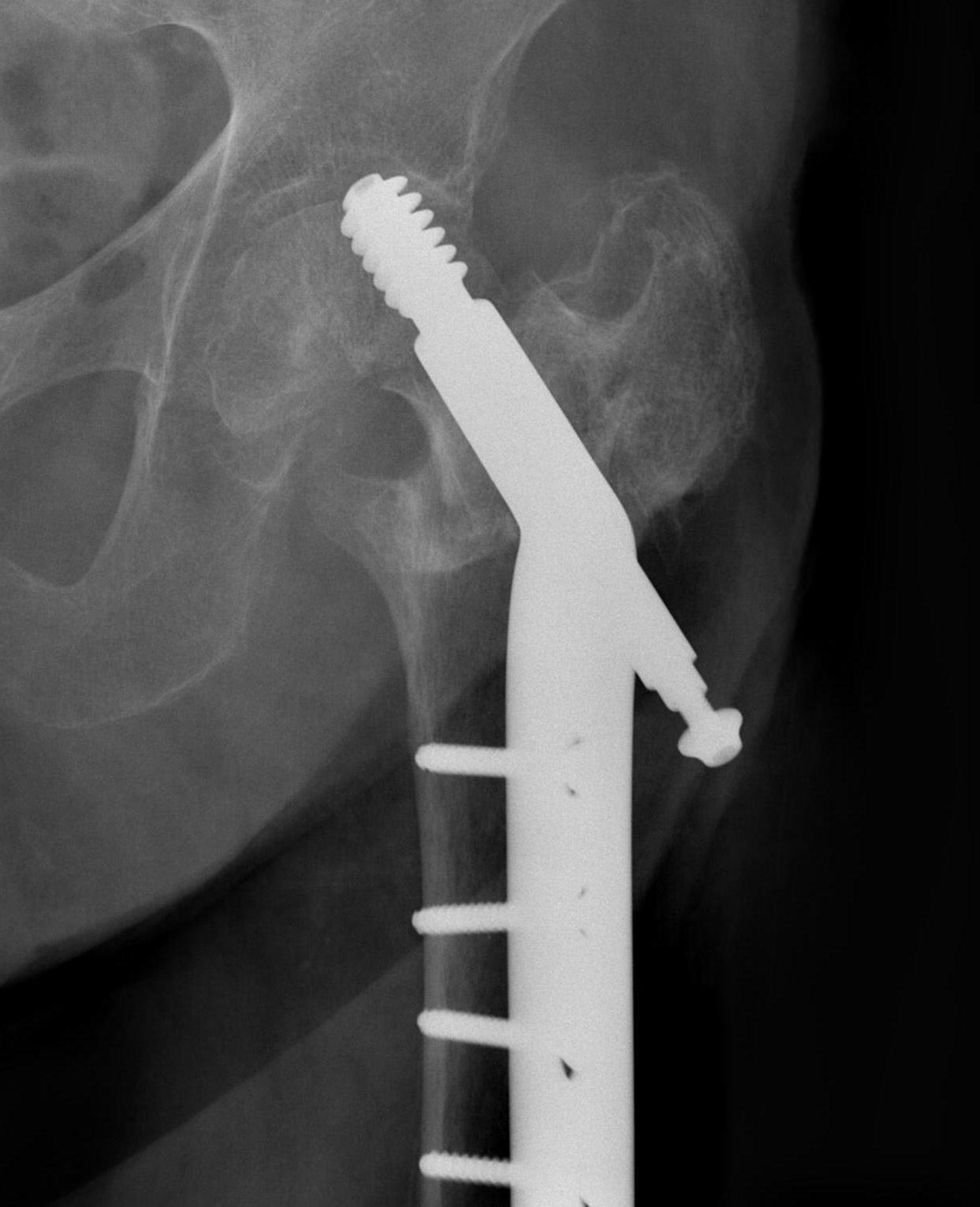
Cephalomedullary nail / Proximal femoral nail


Mechanical advantages
- load sharing rather than load bearing
- decreases lever arm
- supports medial cortex
Surgical advantages
- smaller incision / minimally invasive
- reduced blood loss
- shorter surgical times
Indications
- reverse oblique
- unstable fracture / loss of lateral buttress / loss posteromedial support
- subtrochanteric extension
Technique
Vumedi surgical technique cephalomedullary nail
Stryker gamma nail technique animations
Smith&Nephew Intertan youtube animation
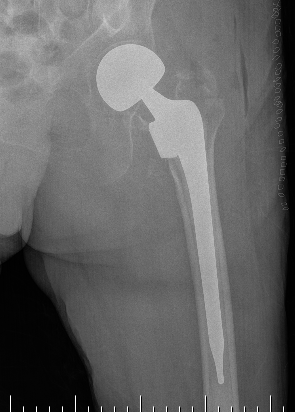
Hemiarthroplasty / Total hip replacement

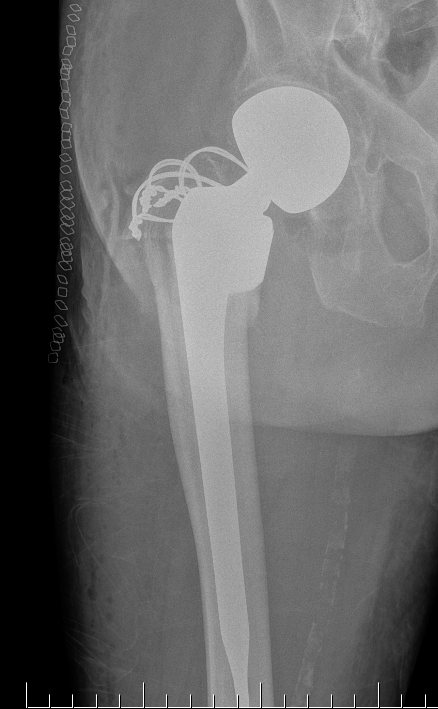
Indications
- severe comminution
- salvage of failure of previous fixation
Technical
- may need calcar replacement
- may need greater trochanter fixation
Complications
Malreduction
Screw cut out
Malunion
Non union
Infection
Periprosthetic fracture
Malreduction

Screw Cut


Causes
- malreduction
- poor screw position / high tip apex distance
- poor bone quality
- Retrospective review of 198 intertrochs treated DHS
- none < 25mm cutout. > 25mm strong predictor of cut-out
Options
- revised to 95o DCS
- hemiarthroplasty / THA
THA Issues


A. Femoral component
- cement will come out screw holes
- Option 1: leave screws in laterally, and strip medially to insert small screws
- Option 2: use uncemented stem
B. Length of femoral stem
- should bypass distal screw hole by 2 cortical diameters
C. Calcar
- normal stem usually sufficient if LT healed back on
- otherwise may calcar replacing
D. Greater trochanter
- may need plate / cables to reduce




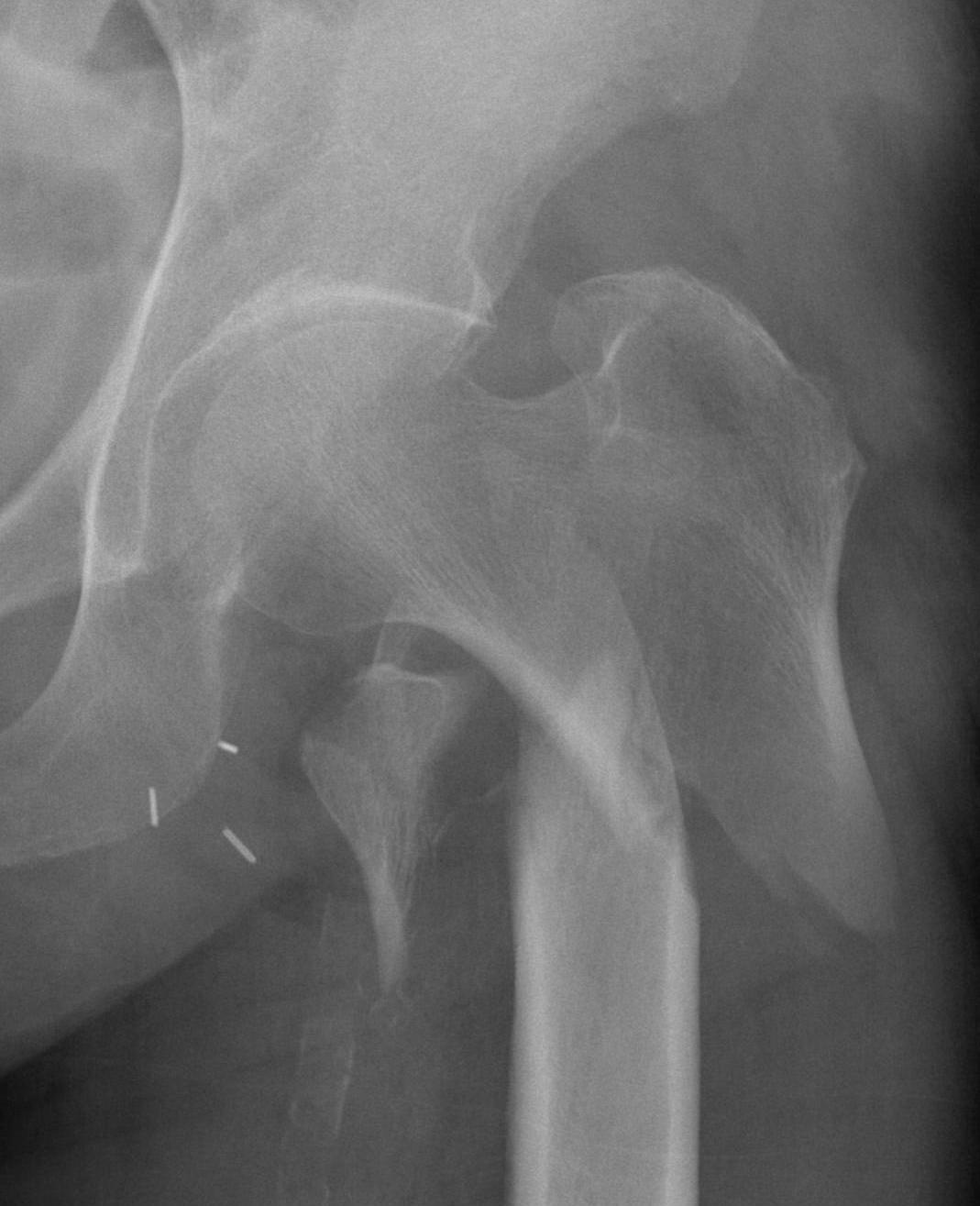
Malunion
Excessive lateral sliding / shaft medialisation
Cause
- collapse with insufficent lateral buttress
- reverse obliquity fracture

Management
1. Fracture united
- remove screw
2. Fracture non union
- revise fixation in young patient
- hemiarthroplasty / THA
Non Union
Uncommon
Presentation
- pain
- hardware failure
- exclude infection


Options
A. Closing lateral wedge valgising osteotomy + graft - younger patients
B. Revision fixation - 95 degree DCS Plate / IM nail
C. THA


Periprosthetic fracture


