Overview
Isolated posterior labral tears
- usually history of trauma
- often have posterior shoulder pain rather than instability
- do well with surgery
Recurrent posterior shoulder instability
- typically dsubluxation rather than dislocation
- often have element of ligamentous laxity / capsular stretching
- crossover with MDI
- arthroscopic management of 136 shoulders with posterior instability
- 51% had reverse Bankart lesion
- 67% had posterior capsular stretching
- 15% had both
Pathology
| Soft tissue | Bony |
|---|---|
| Posterior labral tears | Reverse Hill Sachs |
| Ligamentous laxity / capsular laxity | Posterior bony bankart |
|
Posterior / reverse HAGL |
Glenoid retroversion |
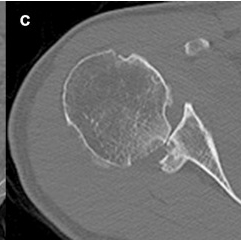
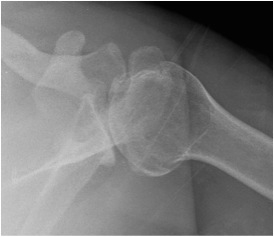
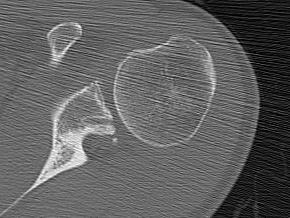
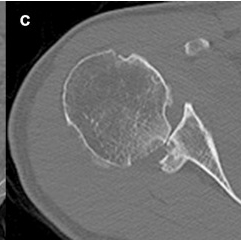
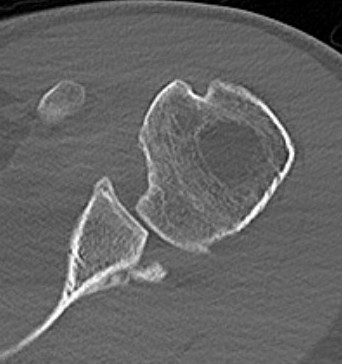
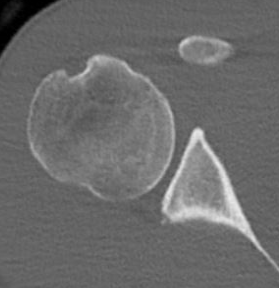
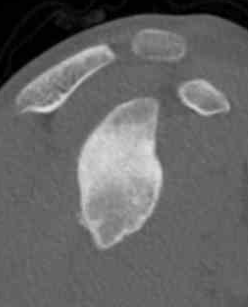
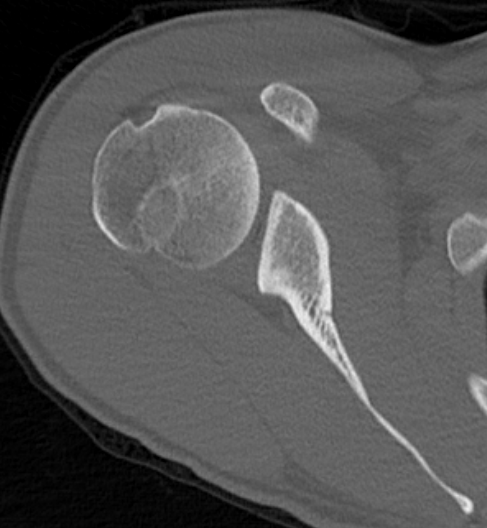
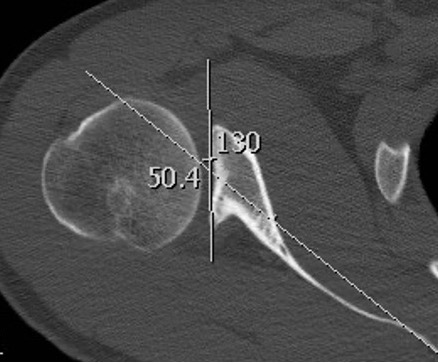
Reverse Hill Sachs / Posterior bony Bankart / Glenoid retroversion
History
Recurrent subluxation / feelings of posterior instability
Traumatic posterior dislocation - MVA / seizures / electrocution
Posterior shoulder pain - more common than instability with posterior labral tears
Examination
Ligamentous laxity / sulcus sign
Posterior stress test - patient supine / adduct, forward flex and IR arm / posterior force / apprehension test
Load and Shift / Posterior Drawer / Altchek Gradingd
Grade 0 No translation
Grade 1+ Up to glenoid rim
Grade 2+ Beyond rim with spontaneous reduction
Grade 3+ Translation beyond rim without spontaneous reduction
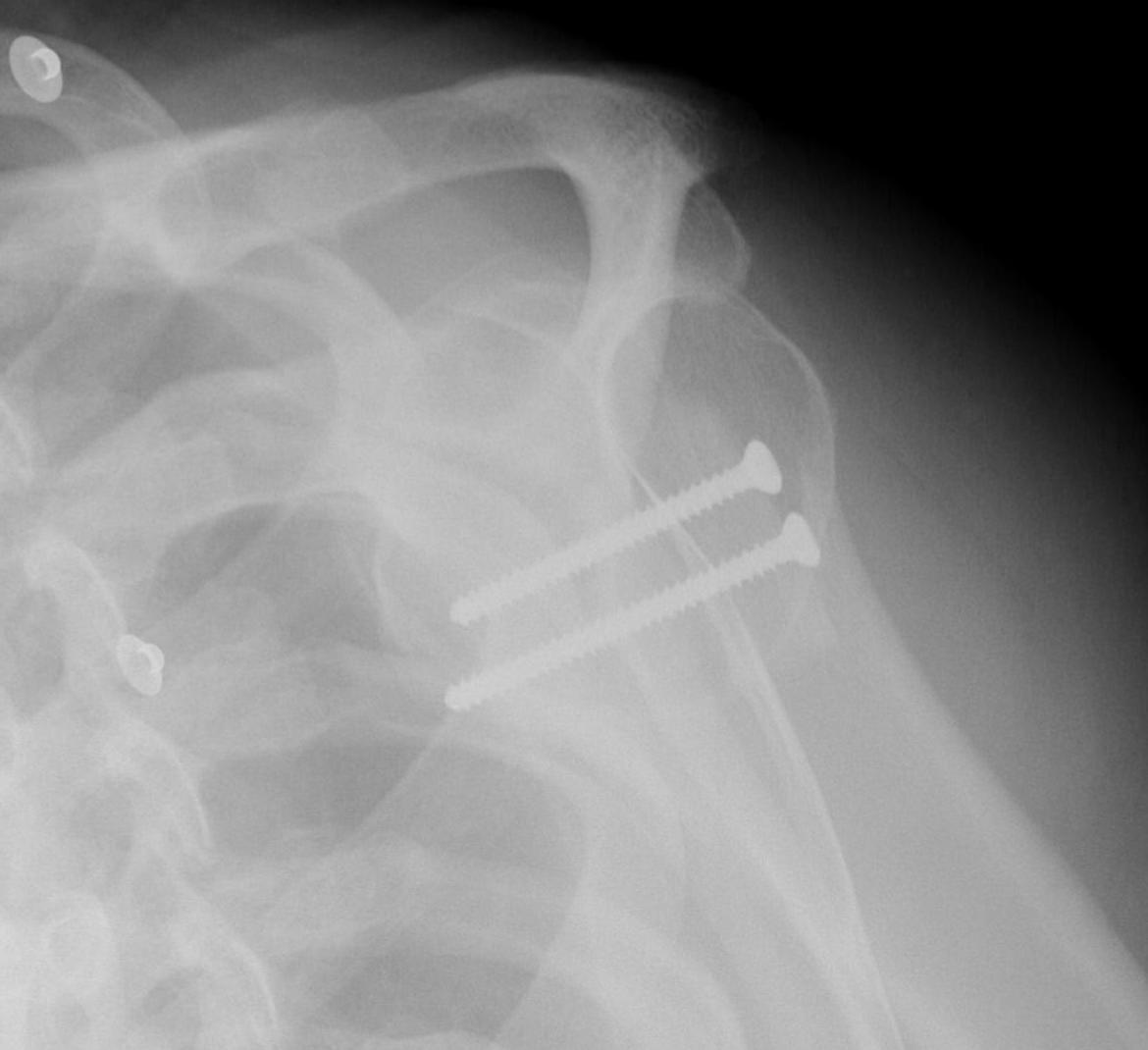
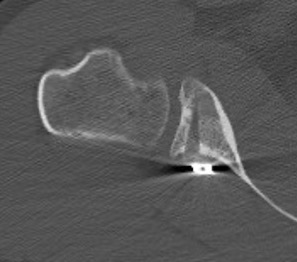
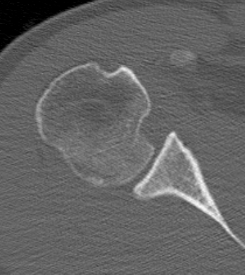
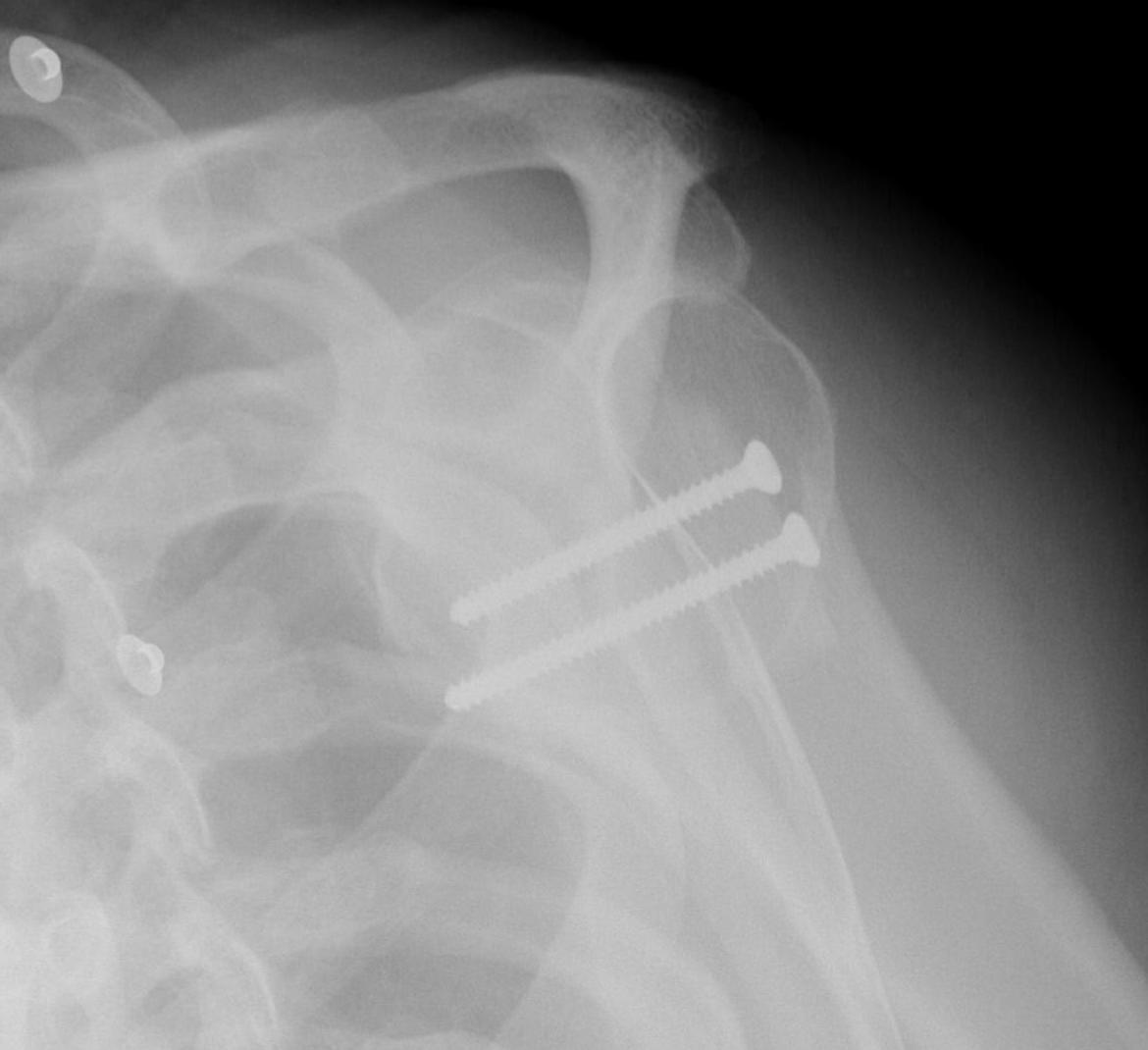
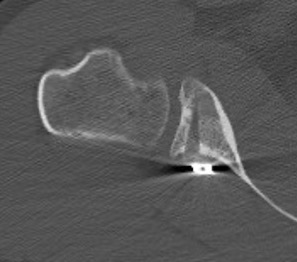
CT
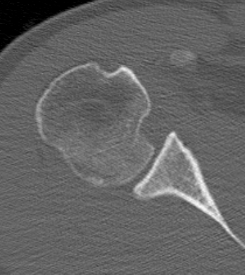
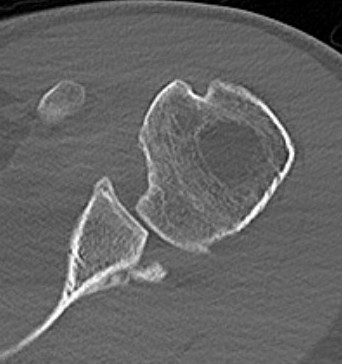
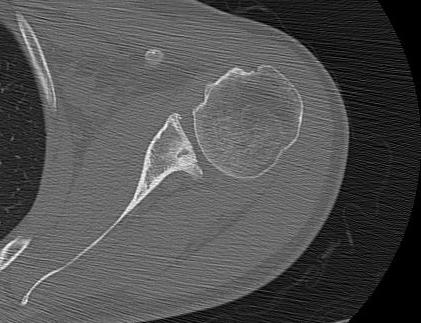
Hill Sachs lesion / posterior bony bankart / glenoid retroversion
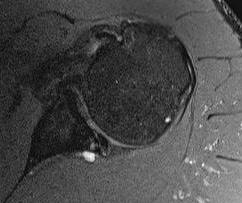
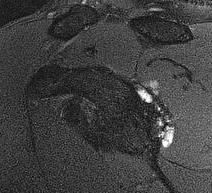
MRI
Posterior labral tears / bankart lesion

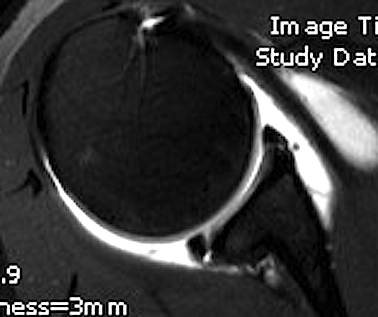
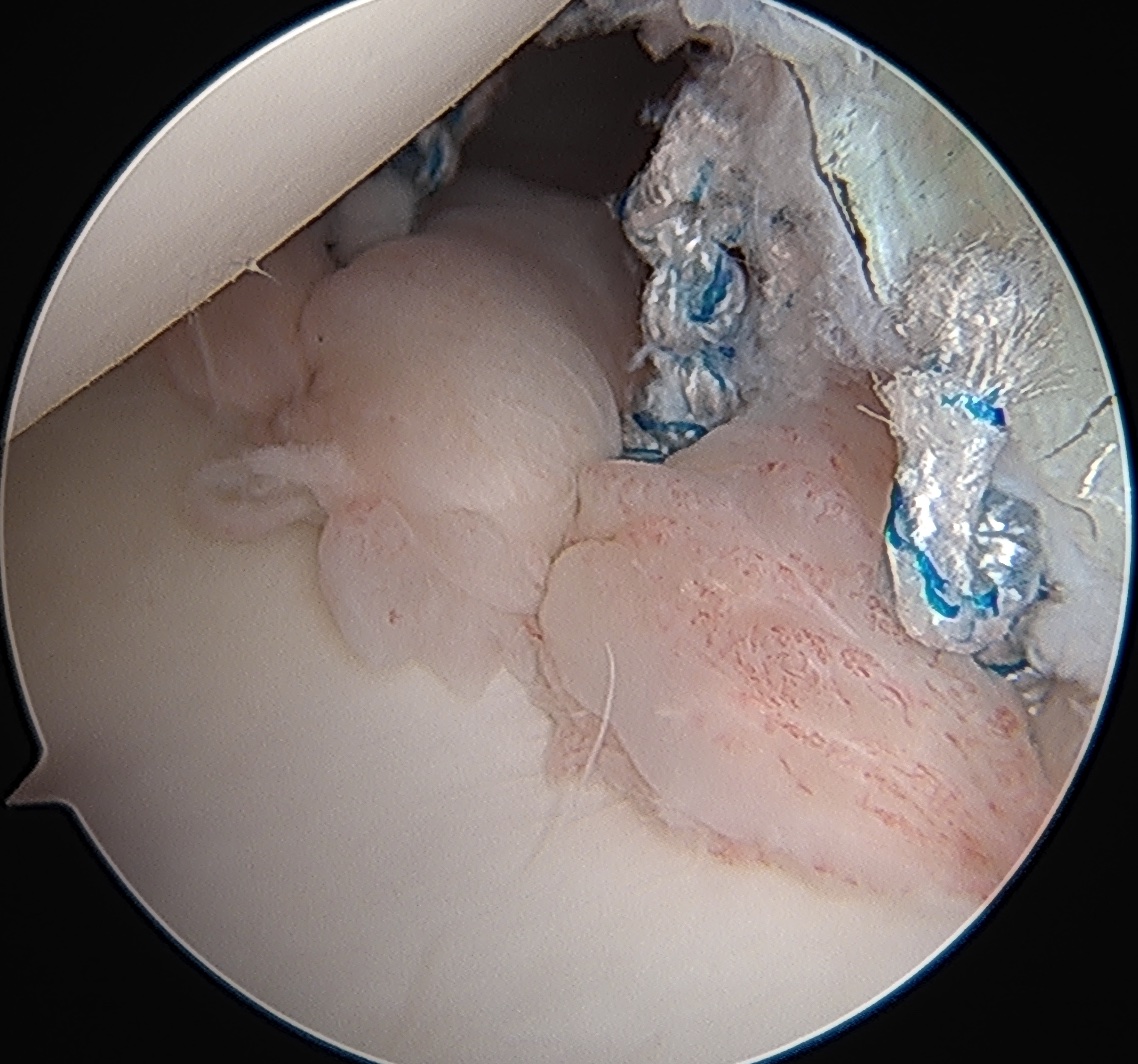
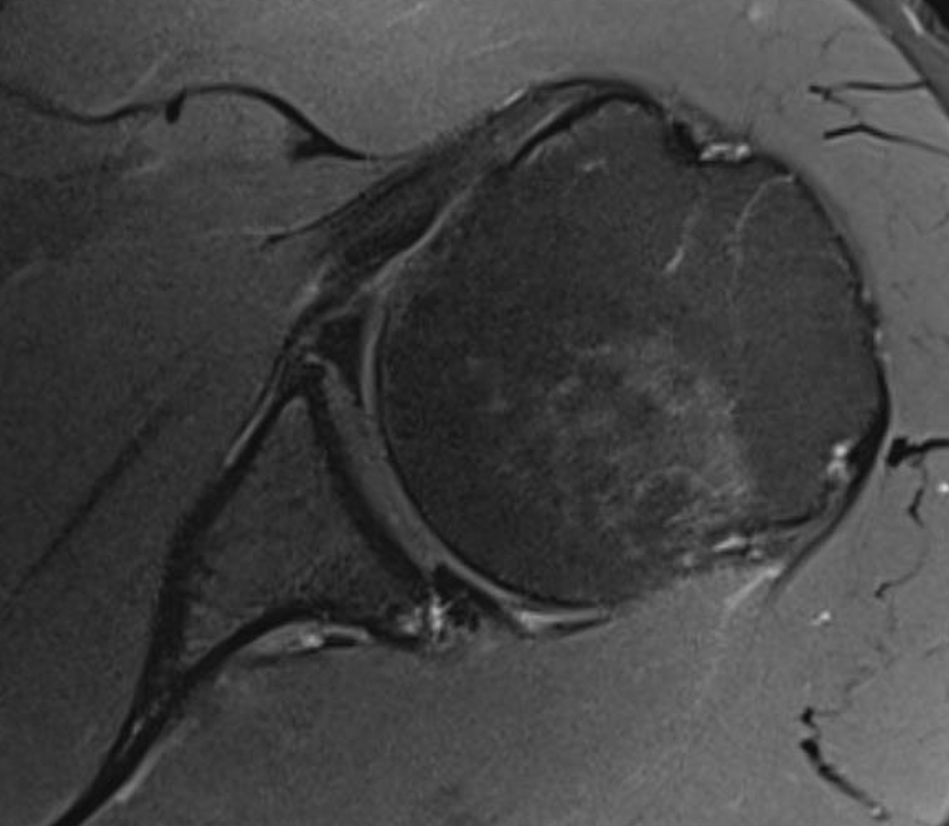
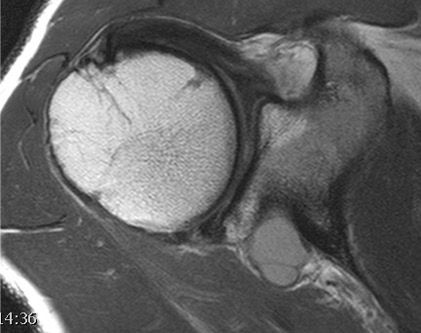
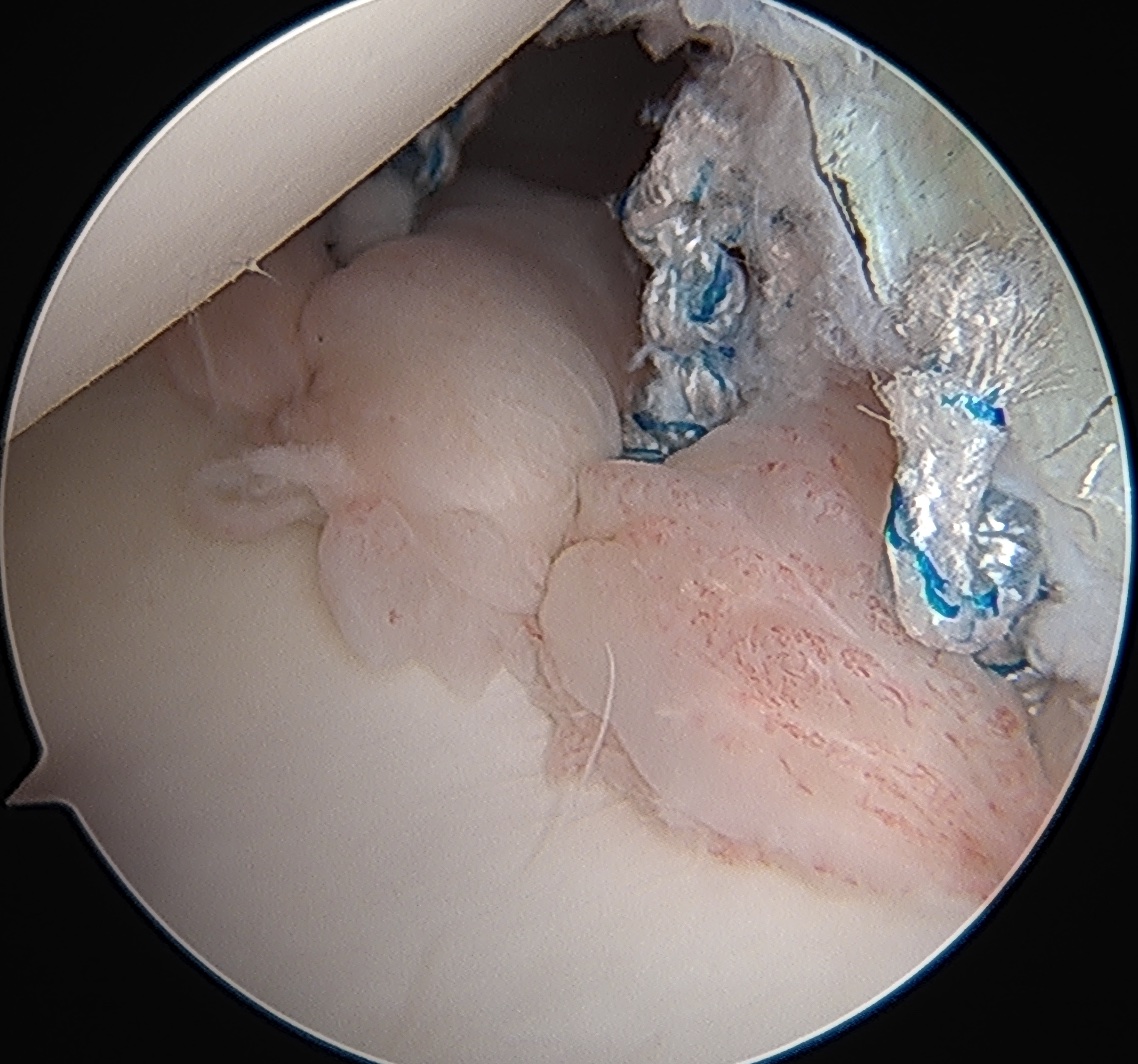
Posterior labral tear


Posterior labral tear
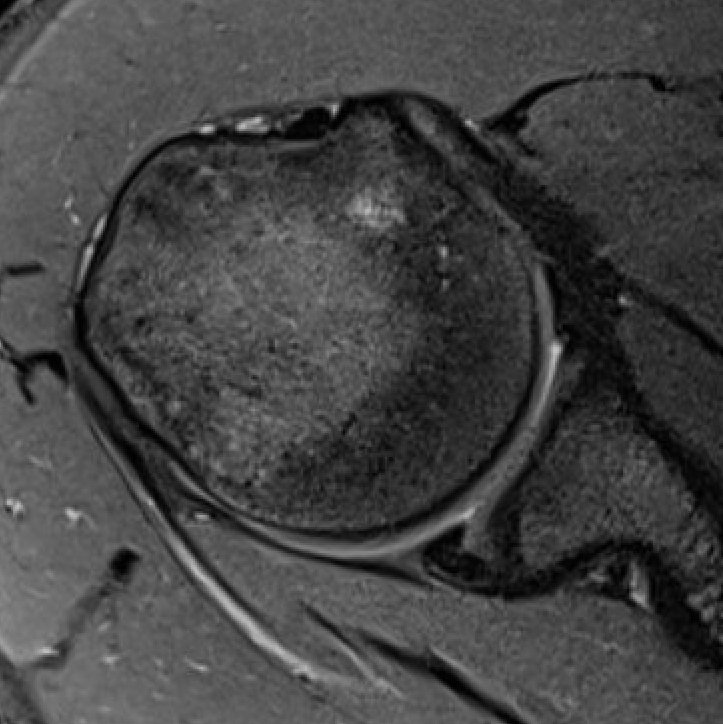
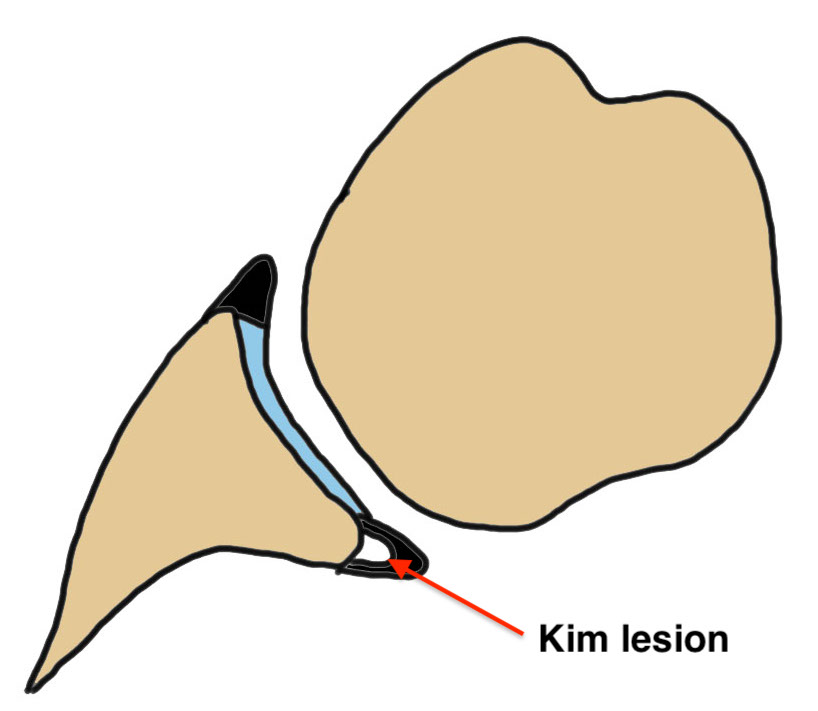
Kim lesion
- Kim lesion
- incomplete and concealed avulsion of the posteroinferior labrum
- superficial portion attached, deep portion detached
- labrum flat with loss of normal height resulting in retroversion of the chondrolabral glenoid
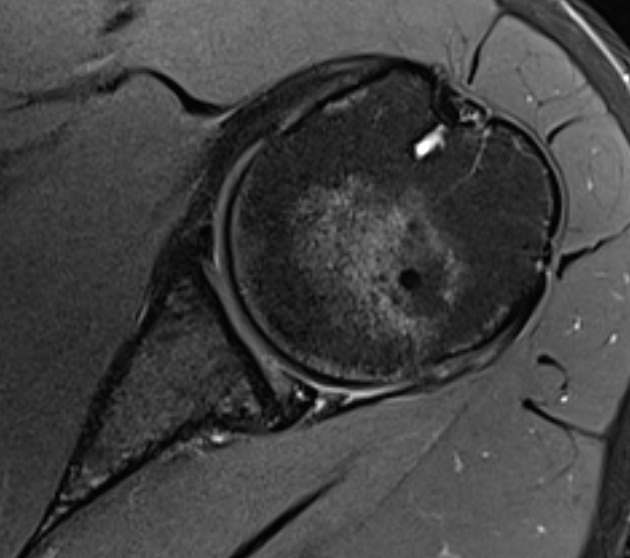
Posterior labral tears + cyst
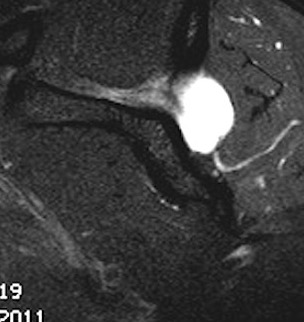

www.boneschool.com/posterior-labral-cysts-suprascapular-nerve-compression
Posterior glenoid wear / osteoarthritis
Beware early posterior glenoid OA presenting as posterior labral tear
Operative management
Indications
Pain - typical with posterior labral tears
Instability - often capsular laxity / ligamentous laxity
Options
| Arthroscopic | Open |
|---|---|
|
Posterior labral repair +/- capsular shift - posterior labral tears |
Open capsular plication +/- infraspinatus shift - revision procedures - ligamentous laxity with no labral tear |
|
Capsular plication - no labral tear - ligamentous laxity with posterior instability |
Posterior capsule reconstruction - revision procedures - ligamentous laxity with no labral tear |
|
McLaughlin procedure / Reverse remplissage - reverse Hill Sachs - add to above procedures |
Posterior glenoid reconstruction / bone block - posterior glenoid bone loss - revision procedures |
Arthroscopic posterior labral repair / capsular plication
Technique
Vumedi arthroscopic posterior labral repair video
Vumedi arthroscopic posterior labral repair + reverse remplissage video
Vumedi arthroscopic posterior labral repair + McLaughlin video
Vumedi arthroscopic posterior capsular plication video
Lateral or beach chair
- posterior cannula with anterosuperior viewing portal
- often need to insert anchors via accessory stab incision
- curved anchors very useful
- anteroinferior viewing portal useful for suture management
- posterior labral repair
- isolated capsular plication often difficult due to limited room and poor tissue
- postoperative external rotation brace useful
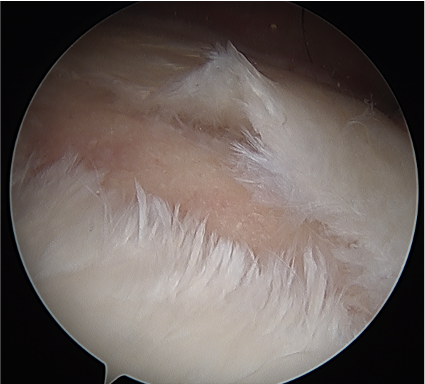
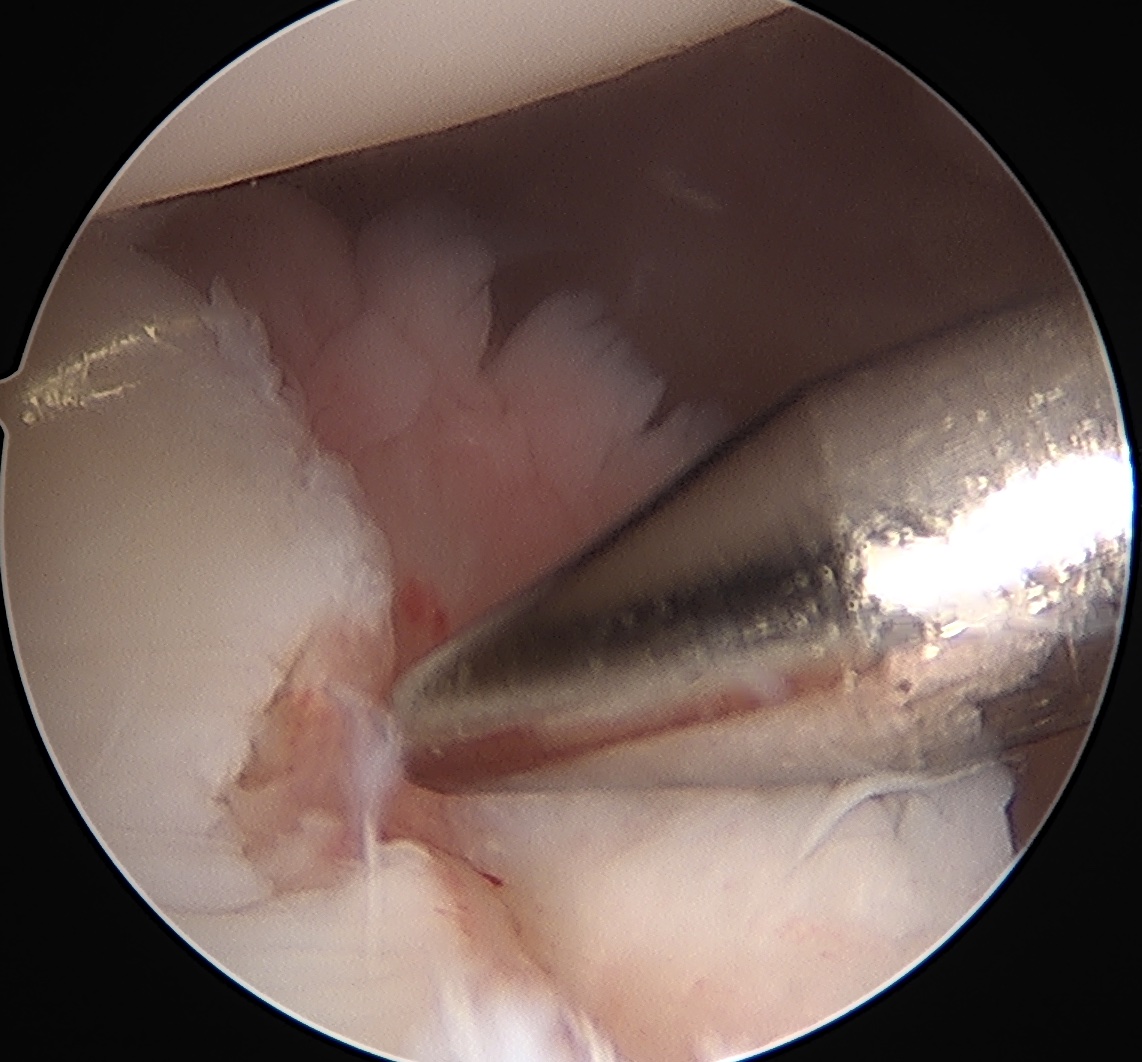
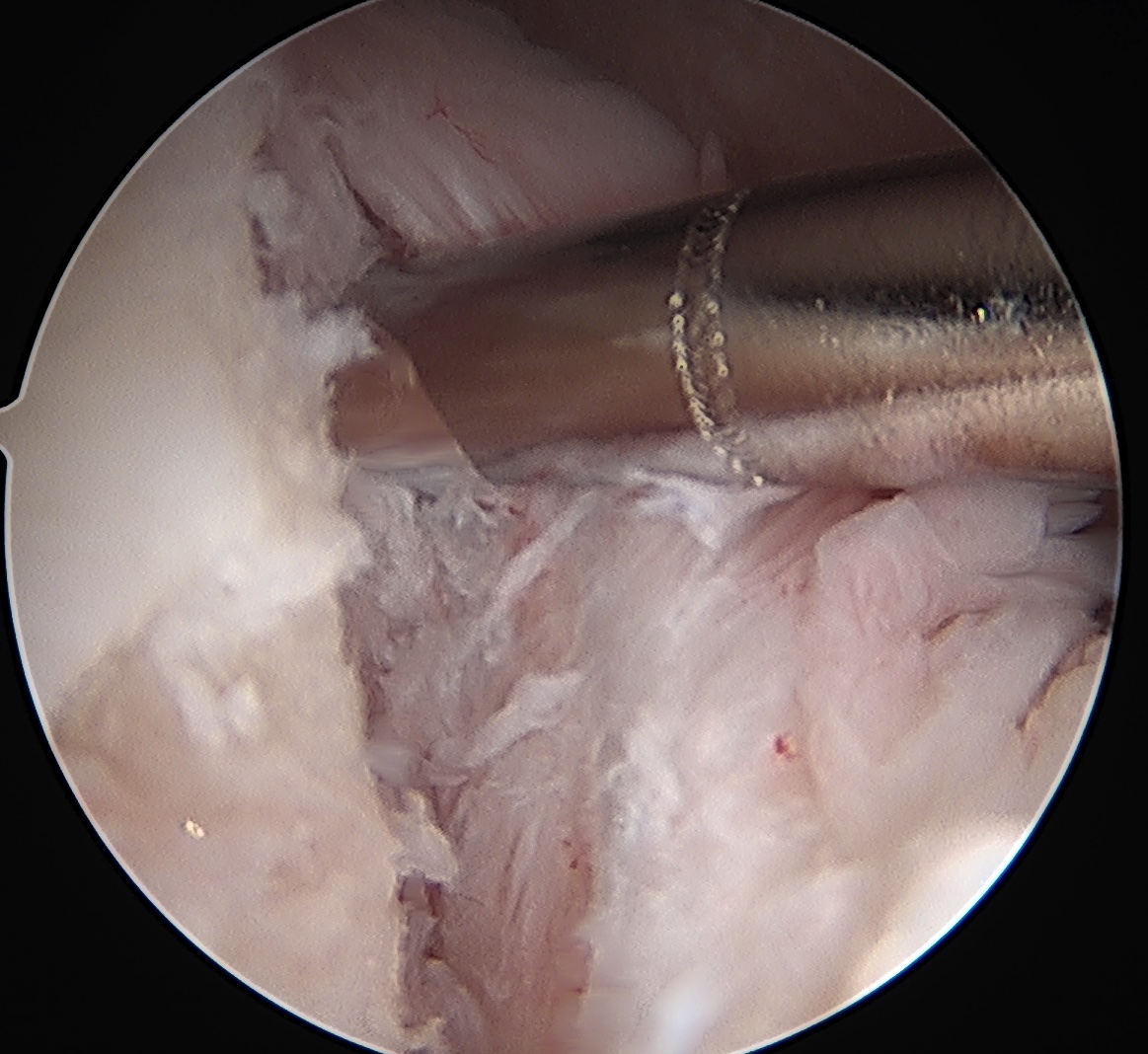
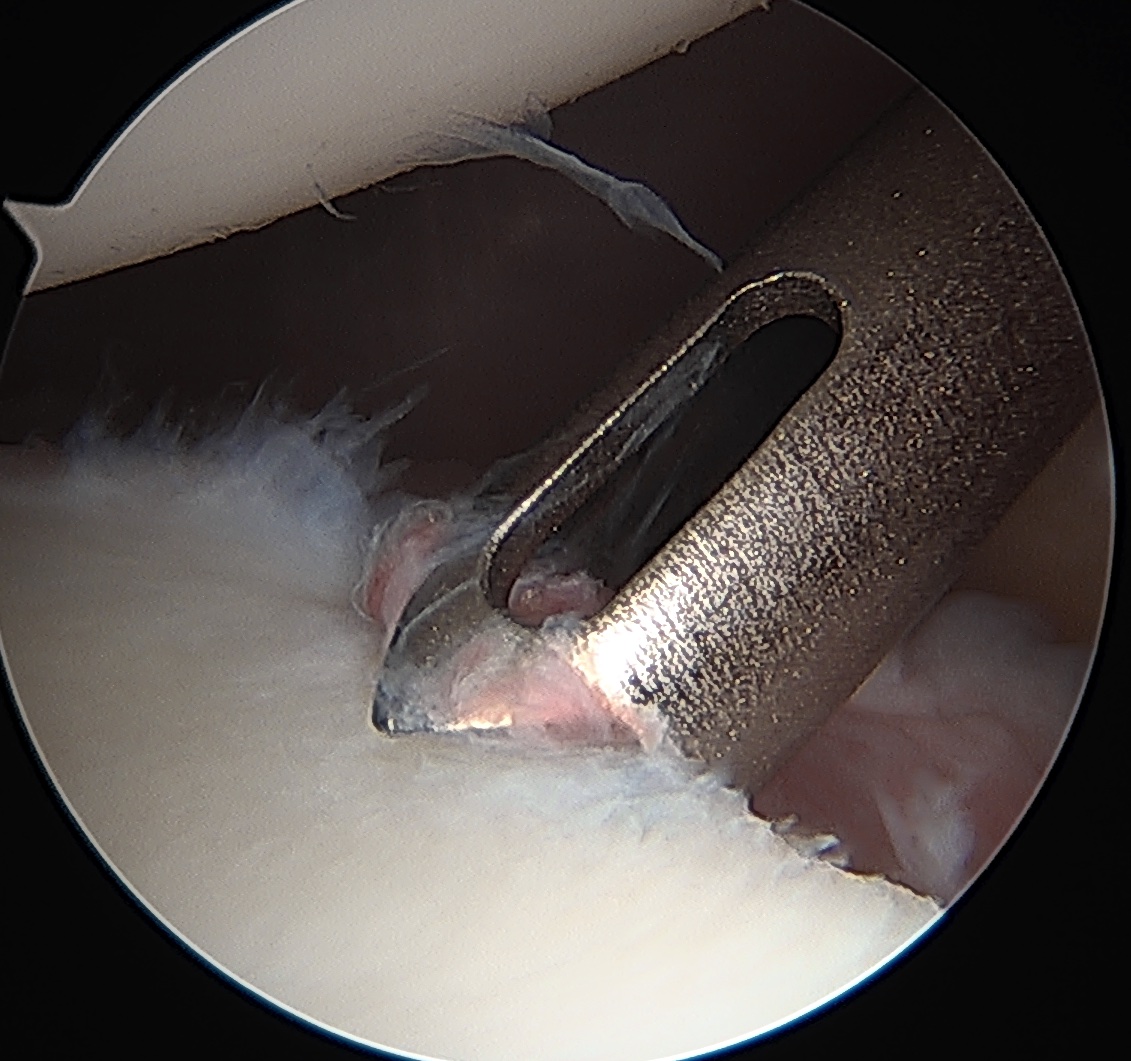
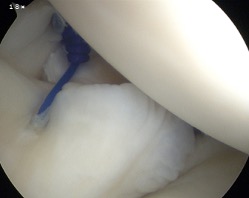
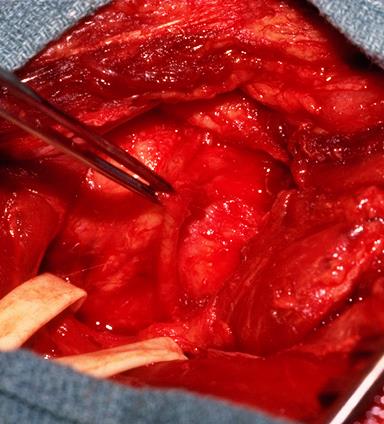
Posterior labral repair
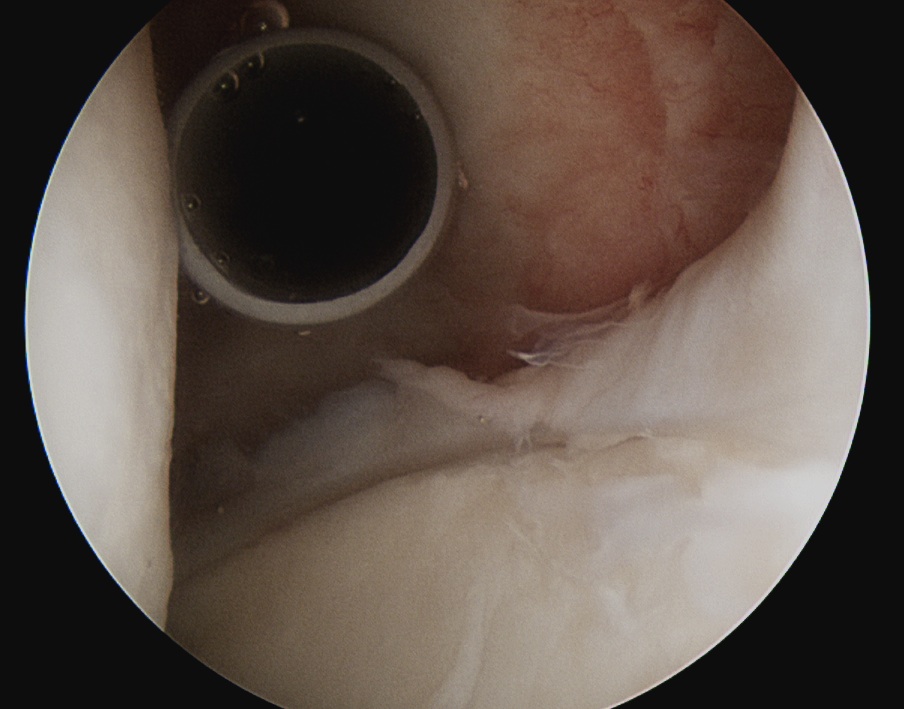
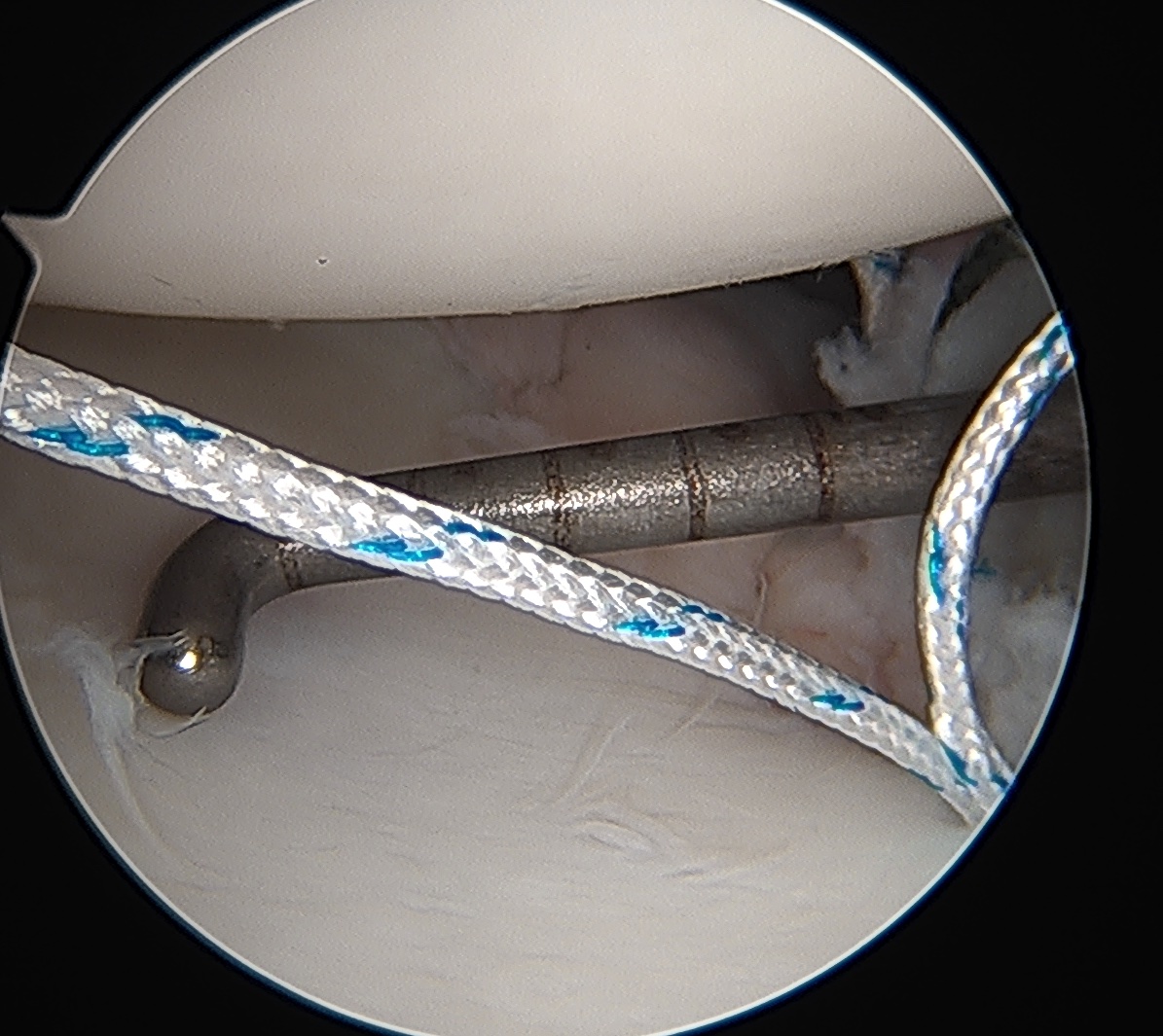
Posterior capsular plication


Results posterior labral repair
Pennington et al Arthroscopy 2010
- 28 patients with isolated posterior labral tears undergoing arthroscopic labral repair
- all had history of trauma to shoulder
- 26/28 (93%) satisfied and returned to sport
Results posterior shoulder instability
- 200 shoulders with unidirectional posterior instability
- treated with capsulolabral repair / plication
- 90% return to sport
- better outcome with capsule plication with anchors versus capsule plication without anchors
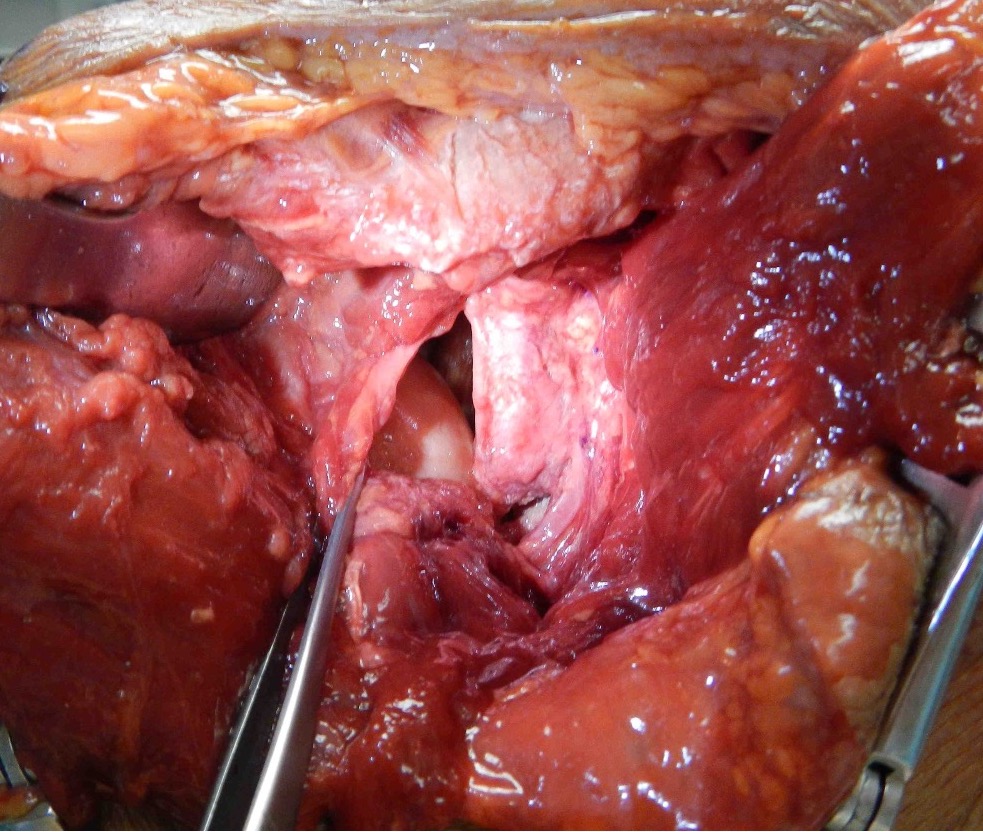
Open posterior capsular plication
Indication
Revision instability surgery
Technique
AO surgical foundation posterior approach glenoid / scapula
Lateral Position
- vertical incision over glenohumeral joint
- elevate deltoid or split deltoid
- interval: between supraspinatus and infraspinatus
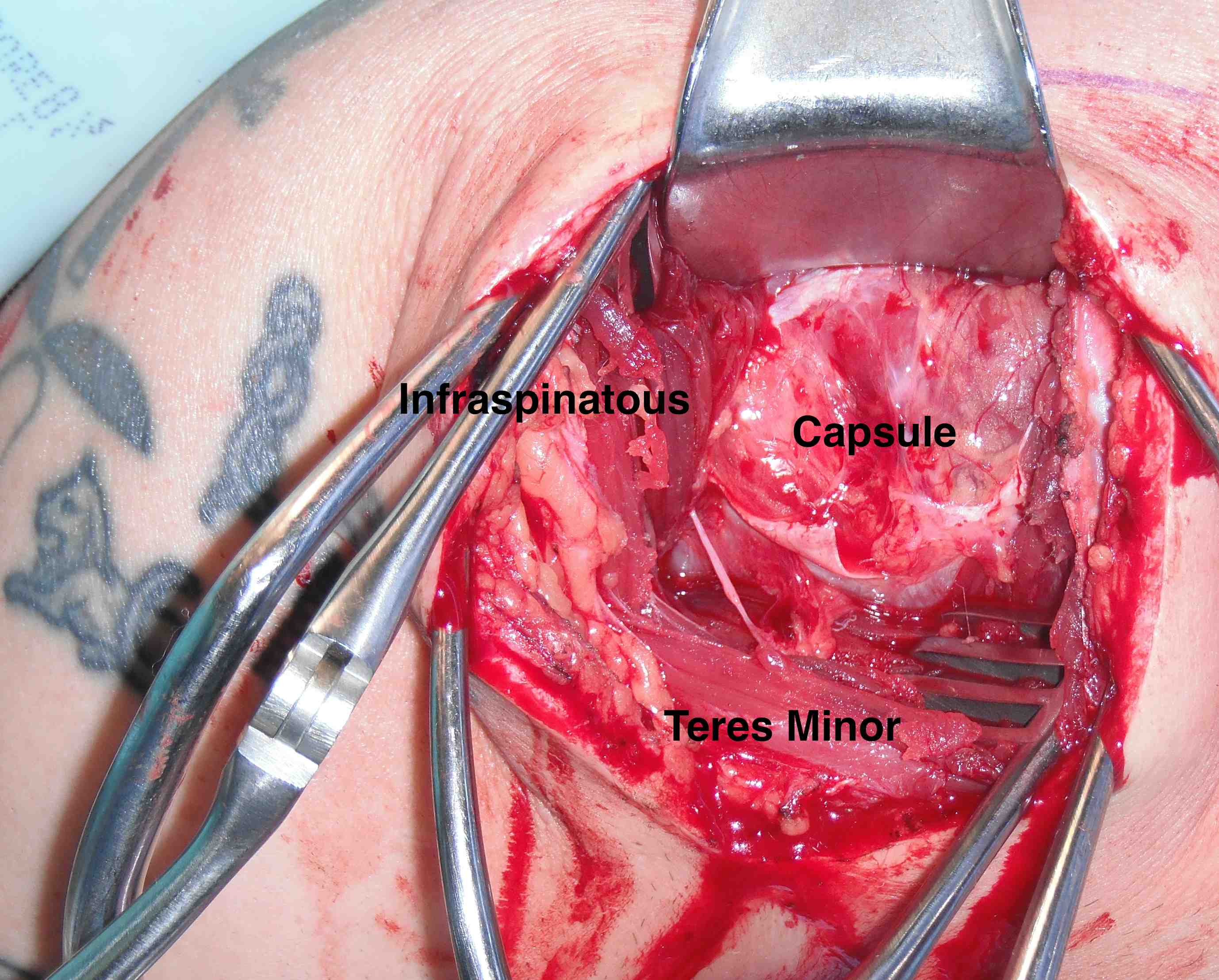
- interval: between infraspinaus and teres minor
- can detach infraspinatus tendon and elevate off capsule
- suprascapular nerve 1.5cm medial to glenoid
- axillary nerve below teres minor
- perform capsular plication / capsular shift
- +/- lateral advancement of infraspinatus


Posterior glenohumeral capsule reconstruction with allograft
Indication
Recurrent posterior instability
Ligamentous laxity
Technique
Arthroscopic posterior capsule reconstruction with acellular dermal allograft PDF
Open posterior capsular reconstruction with acellular dermal allograft PDF / video
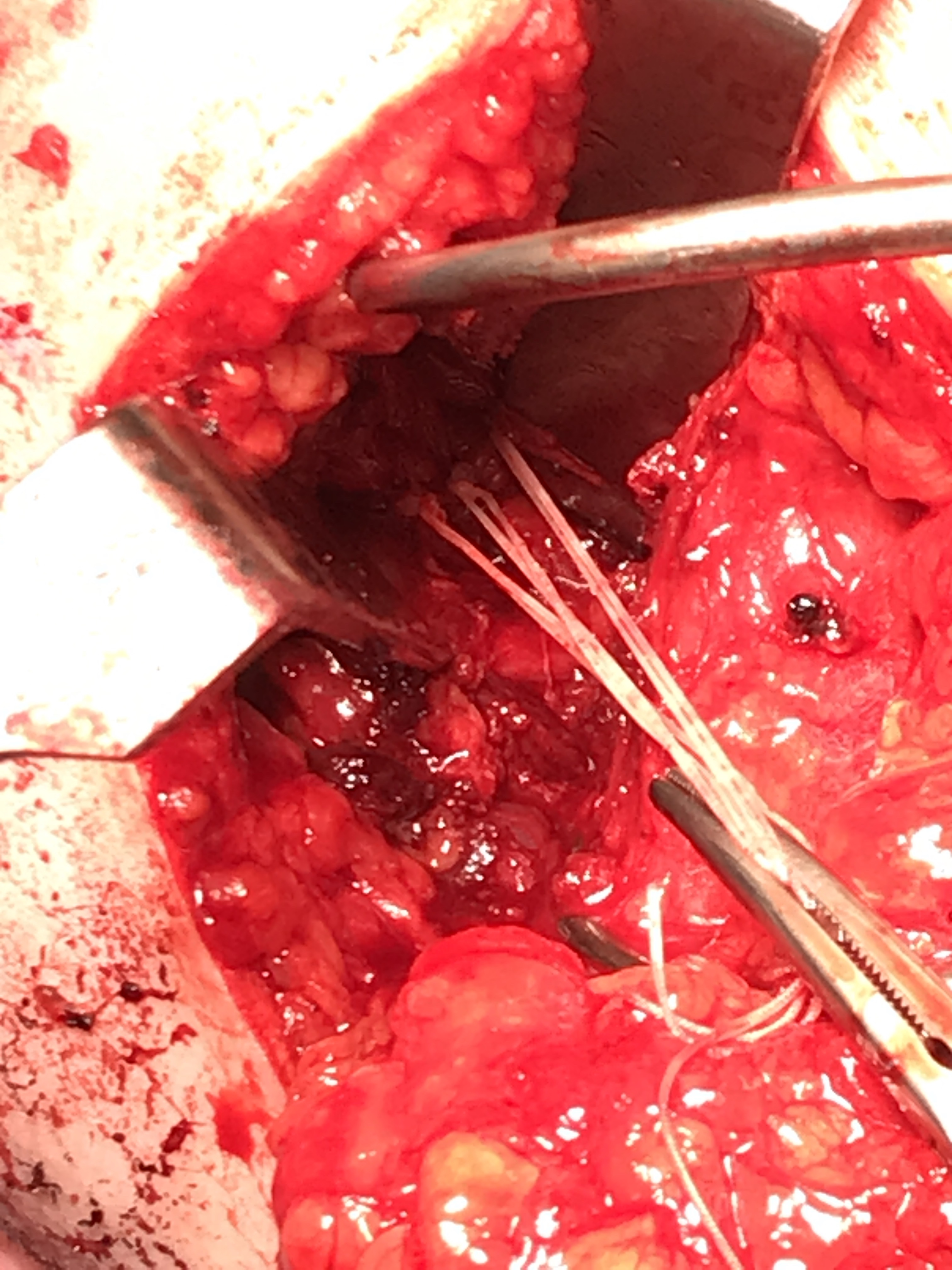
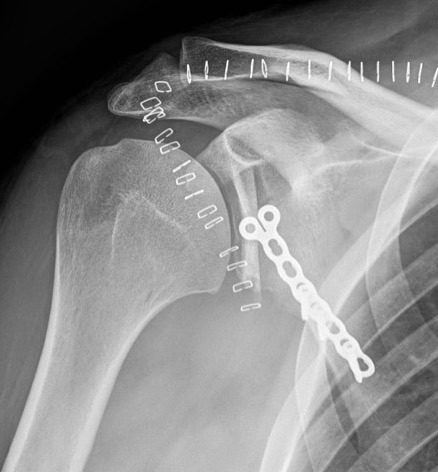
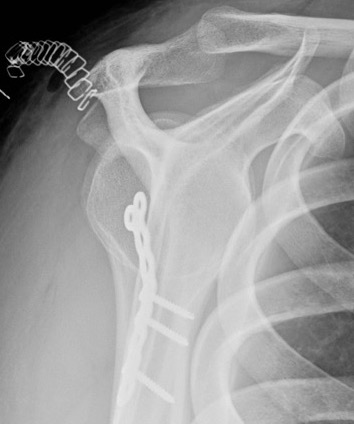
Posterior glenoid reconstruction / bone block procedure
Indication
Posterior glenoid bone loss
Revision posterior instability
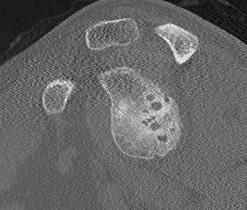
Critical posterior glenoid bone loss
- compared successful posterior labral surgery with unsuccessful
- 11% glenoid bone loss - 10 x failure rate
- 15% glenoid bone loss - 25 x failure rate

Technique
Arthroscopic posterior glenoid reconstruction technique
Open posterior glenoid reconstruction PDF
Open posterior glenoid bony reconstruction PDF
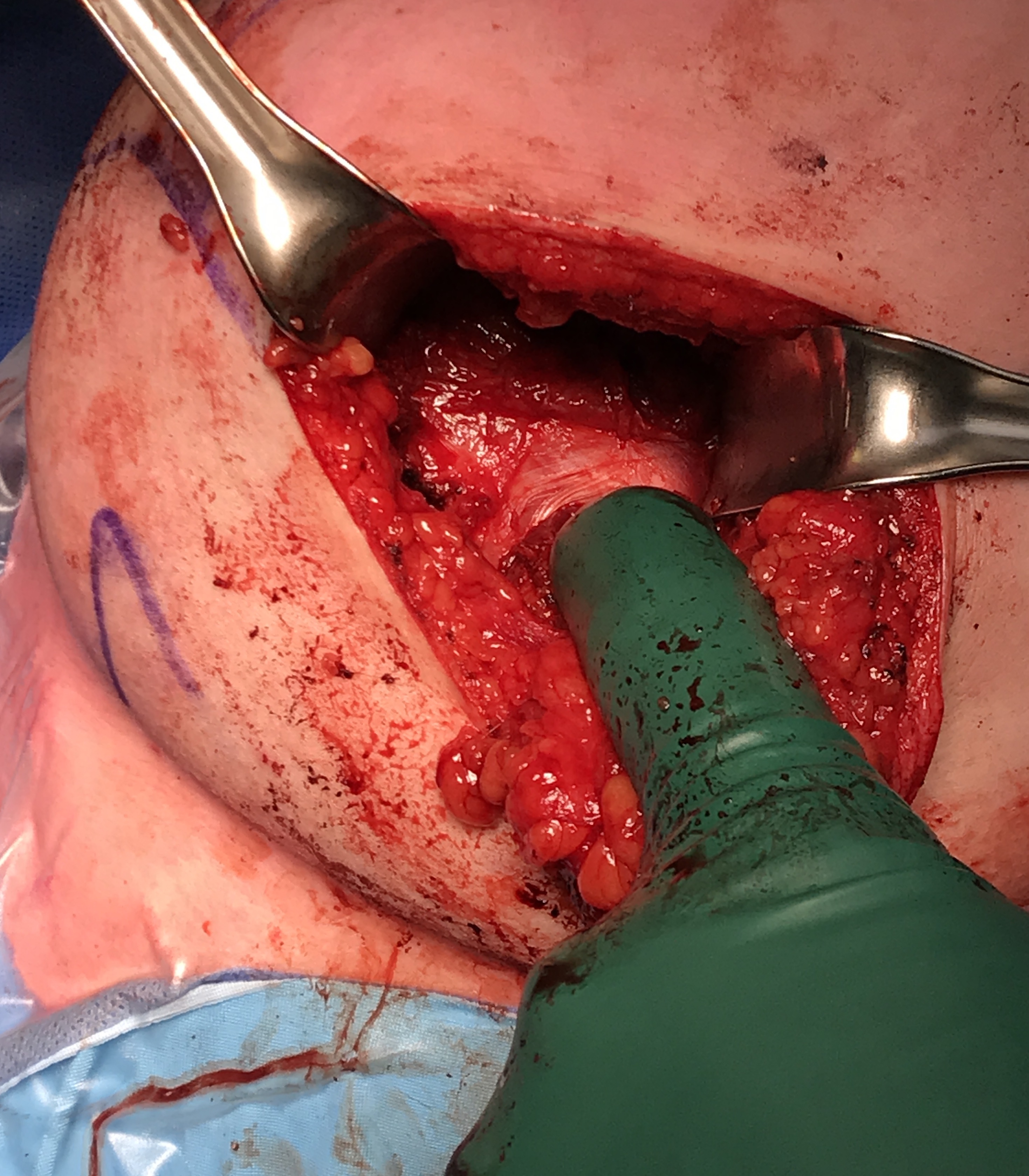
Beach chair or lateral position
- posterior approach / L shaped incision
- elevate or detach deltoid from scapular spine
- detach infraspinatus
- iliac crest or distal tibial allograft
Identify and elevate deltoid / detach from scapular spine / identify infraspinatus
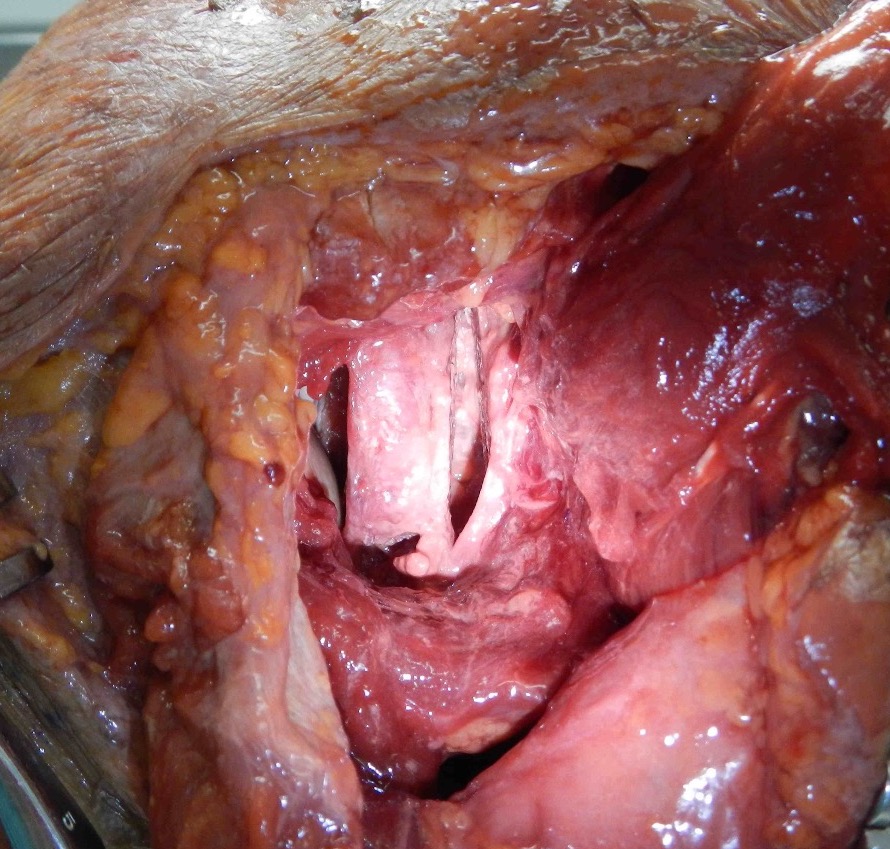
Identify interval between infraspinatus and teres minor, detach and reflect infraspinatus to expose posterior capsule and glenoid

Results
- systematic review of posterior glenoid bone block for posterior instability
- 11 studies and 225 shoulders
- recurrent instability 10%
- complications: 11% hardware, 0.5% wound, 0.5% nerve
- residual pain 12%
Glenoid Osteotomy
Indication
Posterior instability with retroversion > 10 degrees / glenoid dysplasia
Young patient with no osteoarthritis

Technique
Arthroscopic glenoid osteotomy technique PDF
Beach chair or lateral
- posterior approach / detach deltoid / tentomy infraspinatus
- capsulotomy to expose glenoid
- osteotomy parallel to articular surface, 1.5 cm from articular surface
- preserves anterior 1 cm of glenoid to prevent iatrogenic fractures
- open 4 - 5 mm and insert bone graft
- +/- fixation

Results
- 9 glenoid osteotomies for posterior shoulder instability
- good functional outcome and reduction in pain
- residual instability in 75%
- osteotomy did not recenter humeral head
- progression of osteoarthritis continues
- 7 glenoid osteotomies for posterior shoulder instability
- 4/7 good or excellent results
- residual instability in 6/7 (86%)
- 5/7 patients osteotomy did not recenter humeral head
- 100% progression of osteoarthritis continues
