Definition
Symptoms & signs from compression of ulnar nerve near elbow
Sites of Compression
Proximal
Arcade of Struthers
- thick myofascial band, 1.5-2cm wide
- present in 70%
- 8cm proximal to medial epicondyle
- from medial head of triceps to medial intermuscular septum, superficial to nerve
Medial intermuscular septum
- with subluxation, nerve may impinge on it
Medial head of triceps
- hypertrophied (body builders)
Medial epicondyle
Tardy ulna nerve palsy / cubitus valgus
- compression due to valgus deformity of the bone
- previous supracondylar / lateral condyle fracture
Cubital tunnel / Osbourne's ligament
Anatomy
- walls are humeral & ulna heads of FCU
- floor is MCL
- roof is Osbourne's fascia (continuation of fibro-aponurotic covering of epicondylar groove)
Nerve compression
- occurs in flexion as Osbourne's fascia tightens
- MCL bulges out and tunnel becomes flattened ellipse
FCU
Nerve passes intramuscular for ~5cm
- penetrates fascial layer to lie on FDP
- proximal and distal compression possible
Other
A. Lesions in the groove
- medial epicondyle fracture / arthritic spurs / HO
- lipomas / ganglia / osteochondromas / synovitis / rheumatoid nodule
- infection (TB, leprosy) /bleeding (haemophilia)
B. Conditions outside the groove
- external compression
- anomalous anconeus muscle
C. Subluxation / Dislocation from the groove
- laxity / traumatic tear of fibro-aponurotic roof
History
Pain on ulnar side of elbow
Pain & numbness in ulnar fingers
Provoked by elbow flexion
Weakness of fine movements
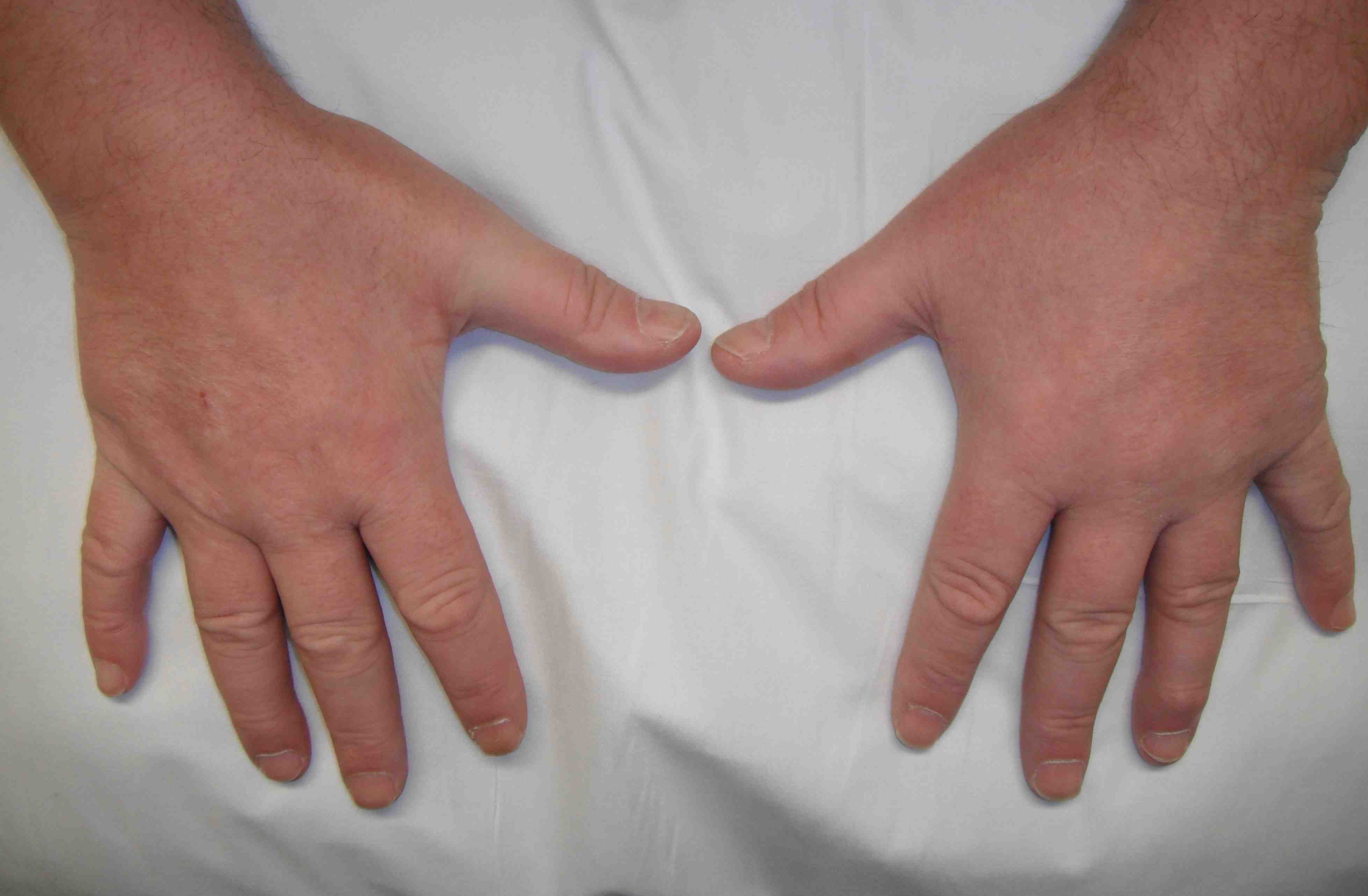
Examination
Look
- deformity or carrying angle
- full ROM
- wasting intrinsics dorsum hand
Feel
- tenderness tunnel
- Tinel's
- subluxation ulna nerve
- sensation in hand / involvement of dorsal and palmar branches
Move
A. Power FCU / FDP LF
B. Hand
- intrinsics
- abductor digiti minimi
- adductor pollicis / 1st dorsal interossei (Froment's)
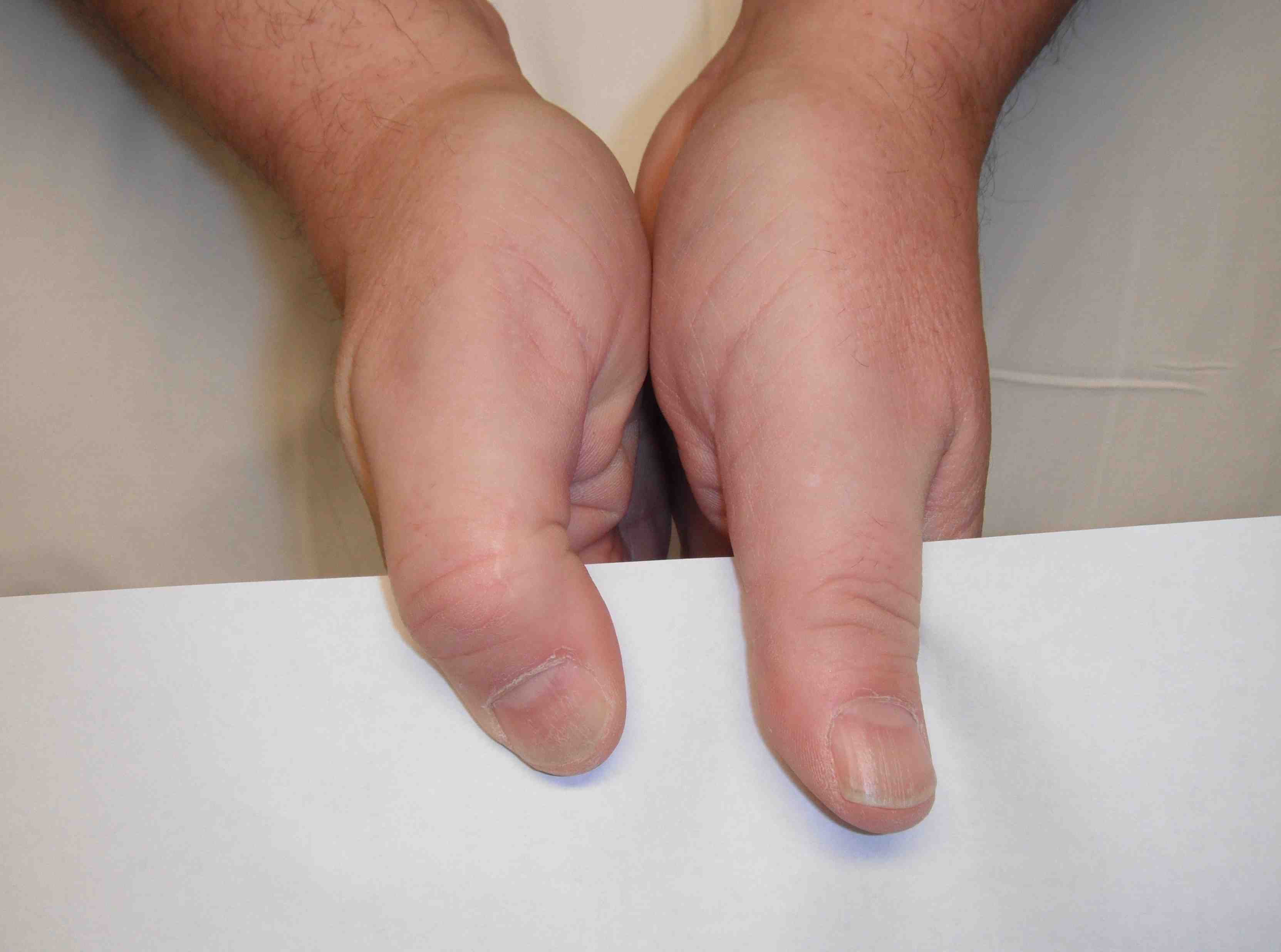
Concealed
- C spine
- axilla
DDx
TOS
- symptoms worse with overhead position
C spine
- neck / shoulder pain
T1 nerve root lesion
- thenar muscle power will be reduced
- decreased sensation medial forearm
C8 nerve root lesion
- IF / MF FDP & FPL weakened
Ulna tunnel syndrome
- sensation normal palmar / dorsal branch
- FCU / FDP LF normal
Pancoast tumour
Systemic illness
- DM
- alcohol
- hypothyroid
- vitamin deficiency
NCS
High false negative
Test with elbow flexed
- < 50 m/s conduction velocity across elbow
EMG
Denervation in hypothenar muscles in severe cases
Management
Non-operative Management
Options
50% resolve with night elbow extension splint
Avoid leaning on elbows
NSAID
Rest / activity modification
Operative Management
Indications
Intrinsic weakness
Failed non-operative > 3/12
Options
1. Open release
2. Endoscopic release
3. Open release + Nerve transposition
4. Open release + Medial Epicondylectomy
1. Open release
Indications
- mild disease
- normal anatomy
- no subluxation
Technique
Incision
- 10cm curved incision centred over cubital tunnel
- 1/2 way between olecranon & medial epicondyle
- extended proximally along medial edge of triceps & distally parallel to border of Ulna
Danger
- Posterior branch of MCNFA
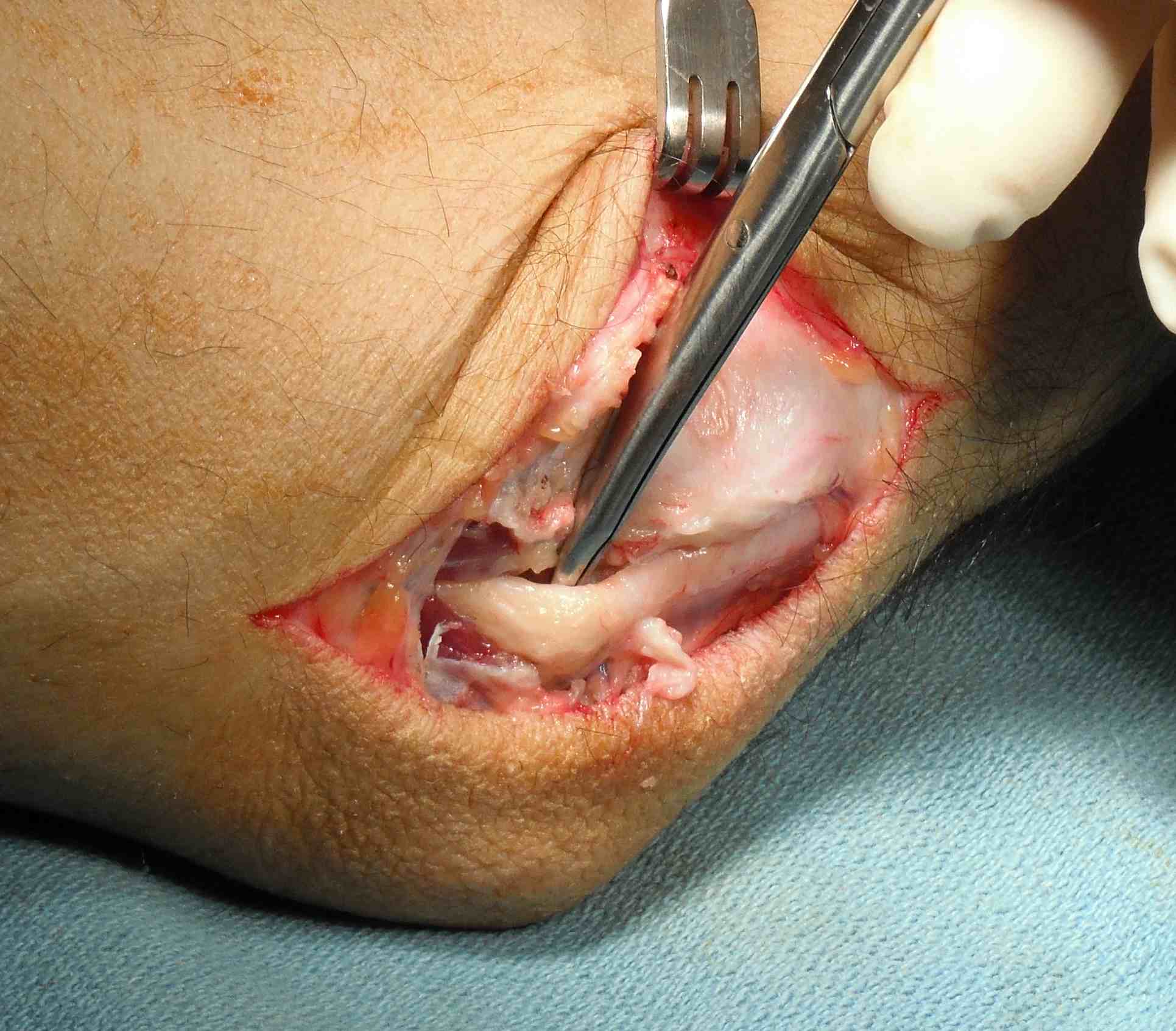
Superficial dissection
- deepened through deep fascia
- nerve identified in proximal tunnel
Release
- proximally ensure no arcade of Struthers
- release Osbourne ligament
- distally release fibrous band of FCU
- ensure ulna nerve stable at end of case
- if unstable, transpose
Dangers
- protect distal muscular branches
- 2 branches to FCU
- branch to FDP

Results
Ziowodzki et al JBJS Am 2007
- meta-analysis of decompression v anterior transposition
- no deformity or previous surgyer
- no evidence of improved outcome with anterior transposition
Vogel et al Br J Plastic Surg 2004
- revision surgery in 22 patients
- combination of simple release and subcutaneous transposition initially
- findings were scarring / incomplete release medial intermuscular septum / incomplete FCU release
- all had submuscular transposition and Z lengthening of CFO
- 78% satisfaction rate
2. Endoscopic Release
Indication
- normal anatomy / simple release
- no SOL / ganglion requiring removal
Technique
Small incision over epicondylar groove
- release osbourne's ligament under vision
- lift skin flaps with special retractor proximally and distally
- insert 30o scope
- release remainder ulna nerve under endoscopic vision
Results
Watts et al J Hand Surg 2009
- compared results from open and endoscopic release
- greater patient satisfaction in endoscopic with fewer complications
3. Nerve Transposition
Indication
- subluxation
- valgus deformity / FFD
- failed decompression / revision surgery
Advantage
- allows functional lengthening of nerve 3-4cm
- low recurrence rate
Disadvantage
- scar formation with possible new proximal site of compression
3 options
A. Submuscular
- muscles elevated from CFO protecting MCL
- nerve transposed anteriorly
- muscles reattached
B. Intra-muscular
- 5 mm trough made in CFO
- nerve transposed into groove
- superficial fascia closed over nerve
C. Subcutaneous
- nerve transposed anterior medial epicondyle
- sutcutaneous tissue from skin flap sutured to muscle fascia behind nerve
4. Medial Epicondylectomy
Indications
- valgus deformity
- malunited fracture
- bony abnormality
Disadvantages
- produces scarring
- protection of medial epicondyle lost / pain if lean on elbows
- weakens flexors (contraindicated in athlete)
- MCL injury can occur
Technique
- nerve identified, released & protected
- CFO elevated
- medial condyle & supracondylar ridge removed
- guide is medial border of trochlea
- flexor origin attached to periosteum
- MCL should be left attached as it is deep & lateral
Complications
Hypertrophic scar
Neuroma MCNF
RSD
Non resolution of parasthesia
