Definition
A HLA B27 positive, seronegative spondyloarthropathy with sacroiliac joint & spine involvement
Mainly affects the cartilaginous joints of the axial skeleton
Diagostic Criteria (1966 New York)
1. Positive X-ray Sacroiliitis

2. One or more of
- lumbar spine pain
- lumbar spine stiffness
- chest expansion < 1" at 4th intercostal space
Epidemiology
1/1000 Caucasian
FHx in 15 - 20% patients
M:F = 3:1
Females
- less progressive spinal disease
- more peripheral disease
Average onset 25 years
Aetiology
HLA-B27
Autosomal Dominant
- 95% of cases
B27 linked to susceptibility factor
- ? Trigger
- ? GIT infection with Klebsiella
Pathology
Two basic lesions
1. Enthesitis
2. Synovitis of Diarthrodial Synovial Joint
Enthesitis
Enthesis is insertion of tendon, ligament or capsular into bone
A. Discs / Manubriosternal joints / Symphysis pubis
B. Hip / Shoulder
C. Spinous processes of vertebrae / Crests / GT
D. Pelvis Crests / GT / Ischial tuberosities / Iliac spines / Pubic symphysis
E. Heels / Achilles / Plantar fascia
Synovitis
Similar changes to RA
- villous proliferation of synovium / pannus destroys cartilage
- joint ankylosed by fibrous tissue
- converted to bone
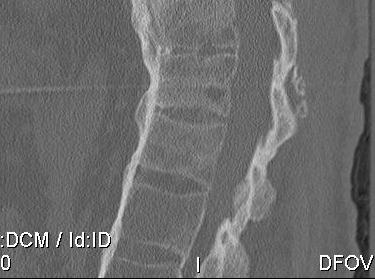
TL spine
A. Spondylodiscitis / Anderson lesion
- erosion of enthesis at anterolateral annulus at endplate
B. Romano's lesion
- lesions heal by forming new bone / early squaring
C. Marginal syndesmophyte
- with repeated episodes forms thin vertical bone due to ossification of annulus fibrosis

D. Bamboo spine
- fusion / bony disc casing


Extraskeletal Manifestations
Acute Anterior Uveitis 20-40%
Aortitis + secondary Aortic Regurgitation 90%
Pulmonary fibrosis
Symptoms
Lower back pain
- insidious onset
- usually dull & poorly localised
Back stiffness
- worse in am & after inactivity
- improved by warming up
- improves with exercise
Neck pain & stiffness
Signs
1. Altered posture
- increased thoracic kyphosis
- loss of cervical & lumbar lordosis
2. Positive "Wall Test"
- cannot put heels / buttocks and Occiput on wall
3. Reduced ROM
- decreased extension earliest & most severe
- decreased flexion
- Schober's Test < 4cm
- decreased lateral flexion
4. Pain & tender SIJ
- SIJ Stress Tests / FABER
- pain on downward pressure on knee in fig 4
5. Decreased chest expansion
- <1" at 4th ICS
- secondary to costovertebral joint ankylosis
Bloods
ESR
- increased in 75% / elevated for life-time
HLA-B27
- positive 90%
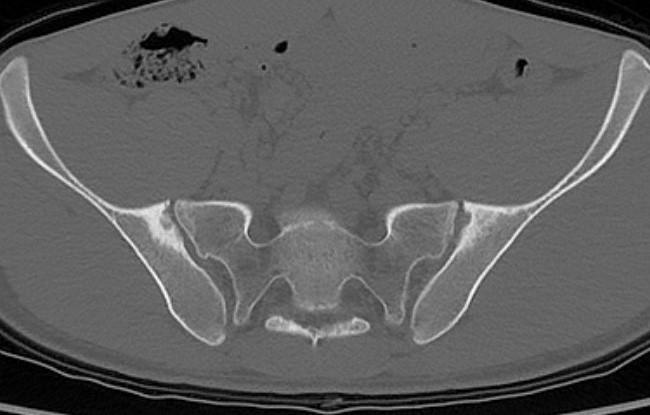
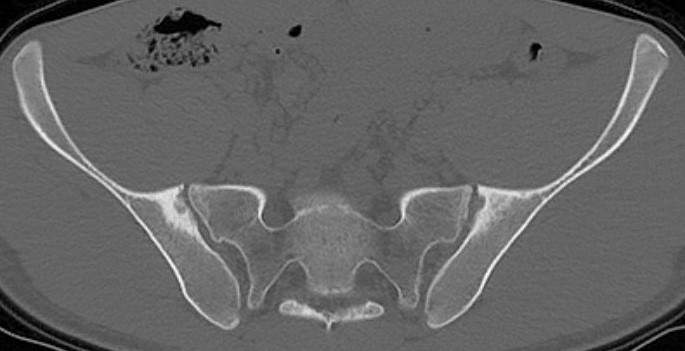
Sacro-iliac joint
- erosion / sclerosis / finally ankylosis

Spine
- marginal erosions / squaring of anterior body concavity
- marginal syndesmophytes
- bamboo spine



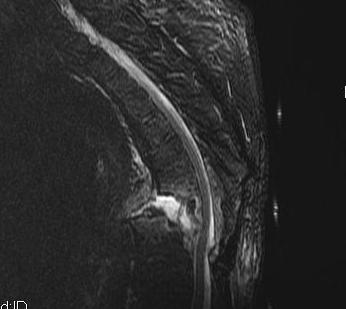
Hip & Shoulder
- concentric joint space narrowing
- bony ankylosis
- protrusio
DDx
Seronegative Seroarthropathies
- Reiters / Psoriasis / Enterocolitis
DISH
- °Inflammatory / no SIJ involvement
- non-marginal syndesmophytes
Scheuermann's
- end plate changes
Management
Non-operative
Simple analgesia
NSAID
Physio
Maintain ROM & posture especially extension
Operative Management
Issues
1. Spinal fracture
2. Kyphotic deformity
3. THR
Spinal Fractures


Pathology
- fused spine acts as long bone
- fracturs at cervico-thoracic junction / thoraco-lumbar junction
Non operative management
- stable, minimally displaced lesion
- no neurological deficit
Operative Indications
- unstable fractures
- incomplete neurological deficit
- failure of bracing
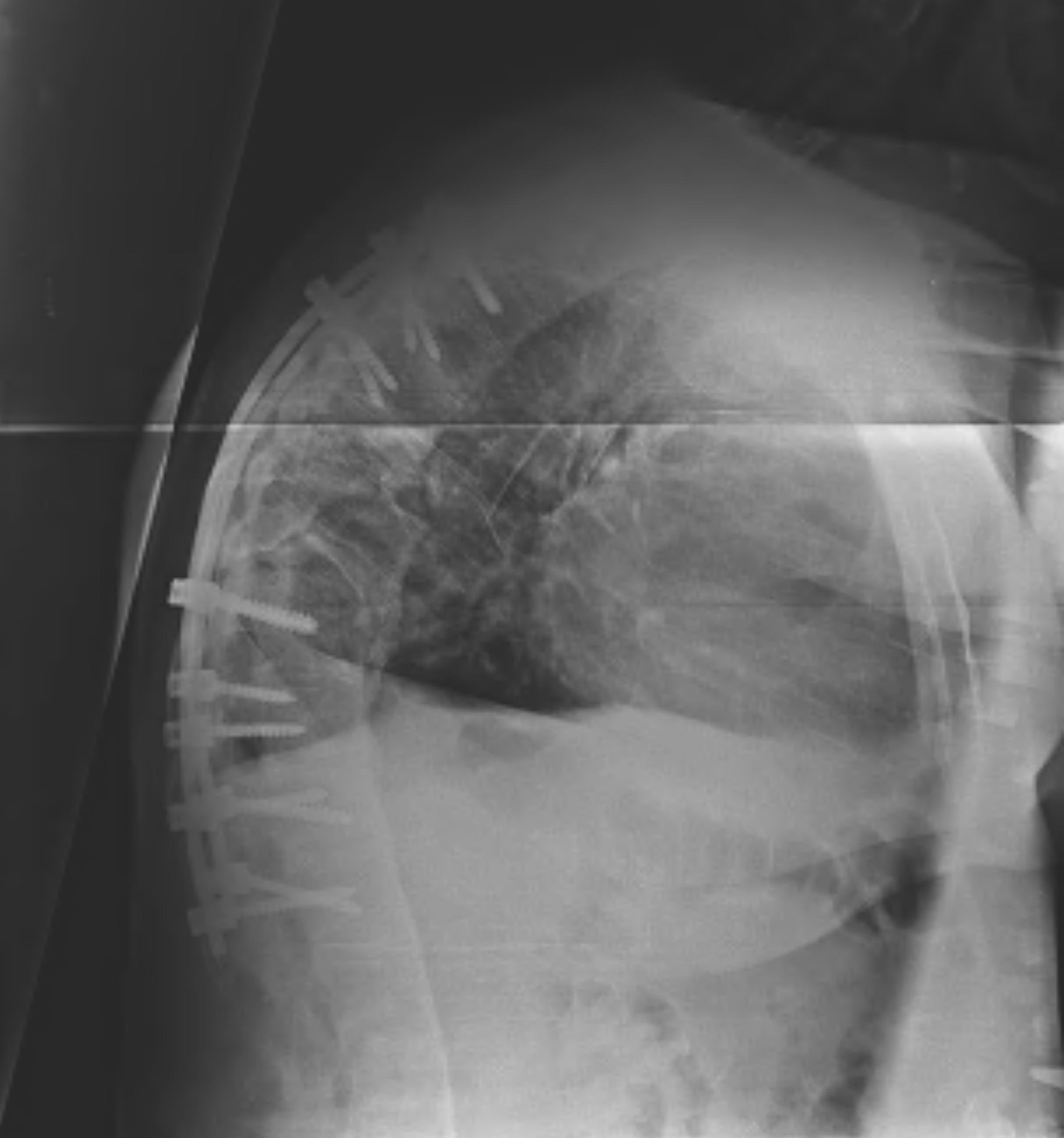
Kyphosis
Indication for corrective osteotomy
A. Severe cervical kyphotic deformity
- difficulty in looking forward / opening mouth
B. Respiratory compromise
- chin on chest position
Contra-indication
- elderly
- aortic calcification
A. Cervical
Use brow-chin angle to calculate osteotomy size
Closing wedge extension osteotomy
- fulcrum must be posterior elements of C7-T1
- avoids vertebral artery at C6
- canal is relatively wide at this level
- C8 nerve root most mobile & expendable
- decompress C8 nerve roots
- short-acting GA when close osteotomy
- wake up test
- HTB post-operatively
Belanger et al JBJS Am 2005
- 26 patients
- average 38o correction
- 1 quadriplegia who died due to subluxation at osteotomy site
- 2 delayed unions
- 5 patients had irritation of C8 nerve root
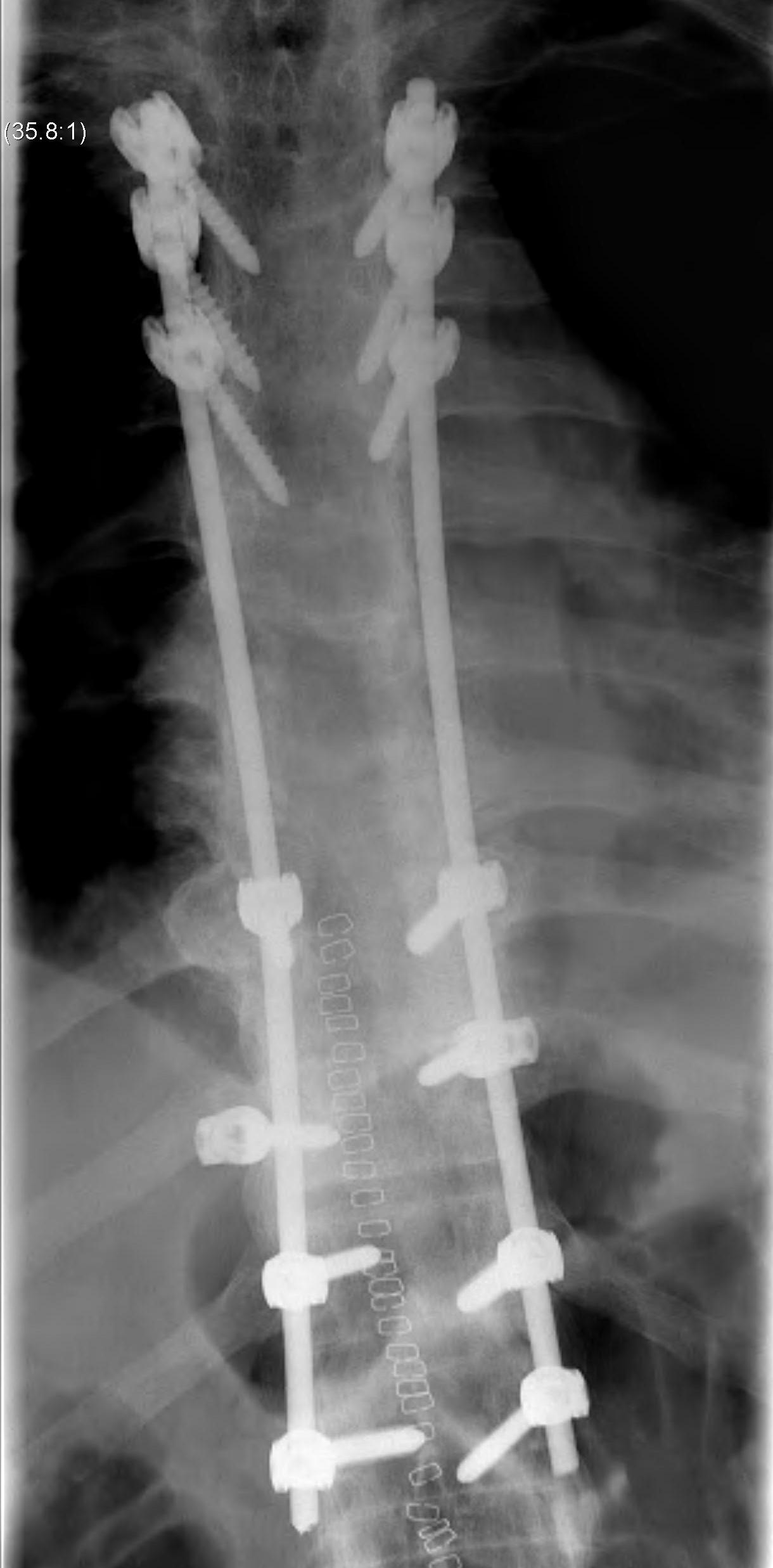
B. Thoracolumbar
Options
Smith-Peterson Osteotomy with instrumentation
- osteotomies in SP above & below central vertebra
- centre of correction is disc / must be healthy
- 10o per level / maximum 30o
- major risk is to aorta
Pedicle subtraction osteotomy
- 30 - 40o per level
- centre of correction vertebral body
- more dangerous / increased correction with better union
THR
Good functional outcome
- no increased loosening seen
- must restore centre of rotation
Main complication is HO
- 20% > Brooker III
- indomethacin indicated
