Anatomy / Biochemistry
Constituents of cartilage
1. Type II collagen
- triple helix
- provides tensile strength and mechanical integrity
- 50% of dry weight
2. Proteoglycans
- 10%
- glycosaminoglycans with keratan sulphate and chondroitin sulphate
- negative charge has high affinity for water
3. Water
- 65-85% of weight
- highly attracted to GAG
- resistant to compressive loads
4. Chondrocytes
- 2% weight
- low oxygen, avascular environment
- anaerobic metabolism
- make collagen and GAG
Structure of cartilage
Superficial zone
- 10-20%
- arranged parallel to surface
Intermediate zone
- more haphazard
Deep zone
- chondrocytes in columns
- perpendicular
Calcified Zone / tidemark
- above subchondral bone
- any mitotic ability of chondrocytes ceases when this develops
Pathology
Inability to heal
- avascular
- nil pluripotent cells in maturity
- nil mitotic ability
- limited synthetic ability in adult
Some ingrowth from sides can occur
- healing size dependant
- 3 mm lesion will heal
- 9 mm will not
Damage
- loss of cartilage results in loss of water and increased stiffness in remainder
- vicious cycle of continued damage
- nil ability to heal unless penetrates thick subchondral bone
- allows bleeding and primitive mesenchymal cells
- typically produce fibrocartilage
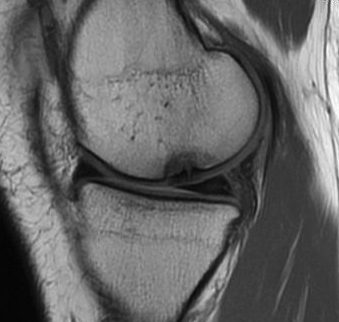
MRI

Classification
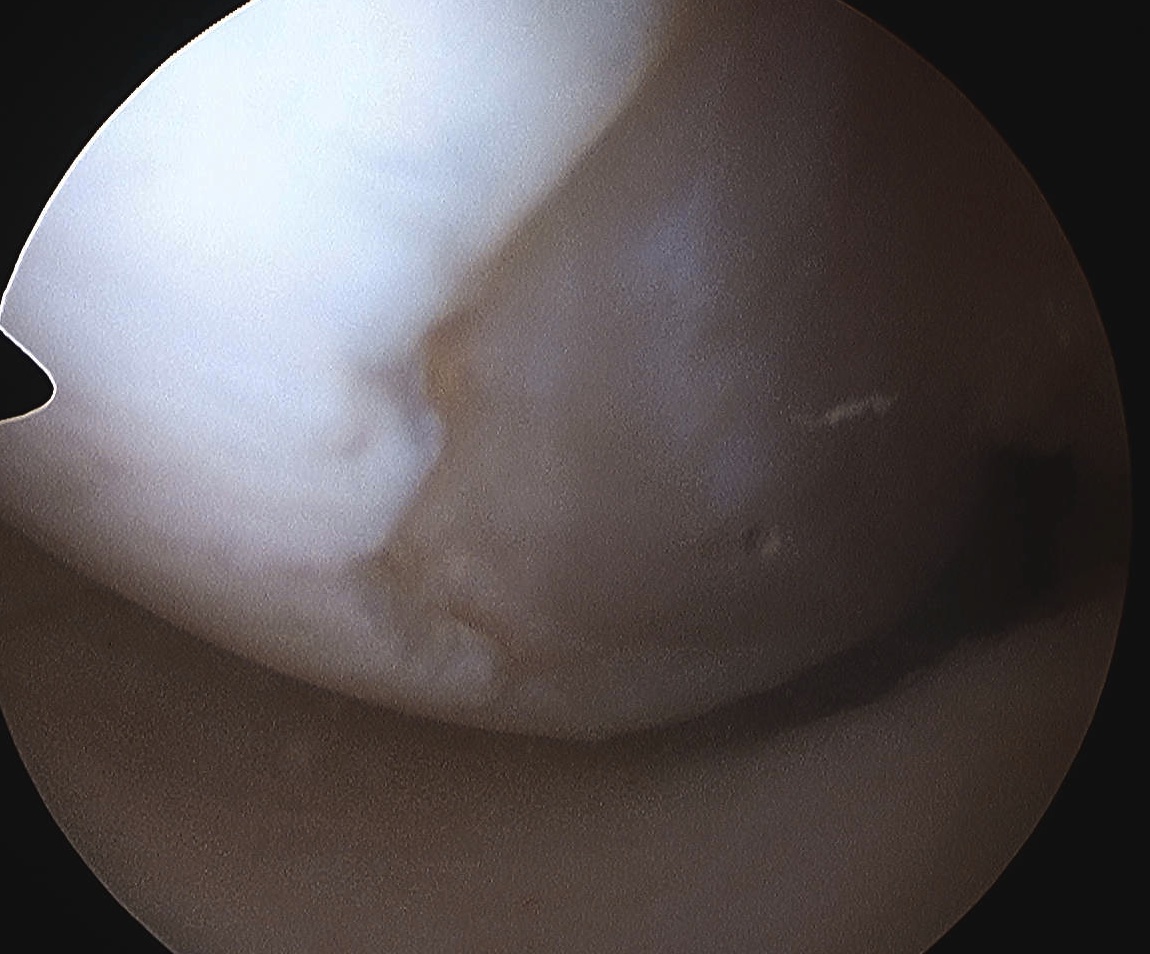
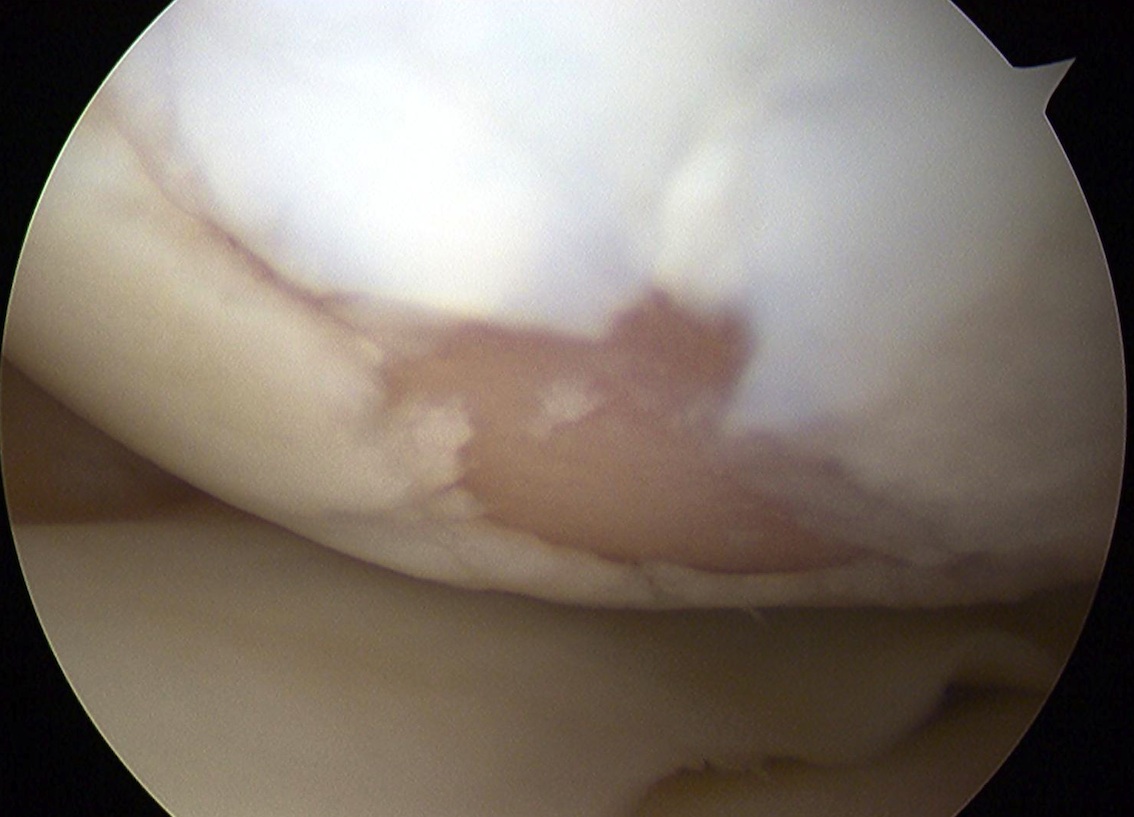
Outerbridge
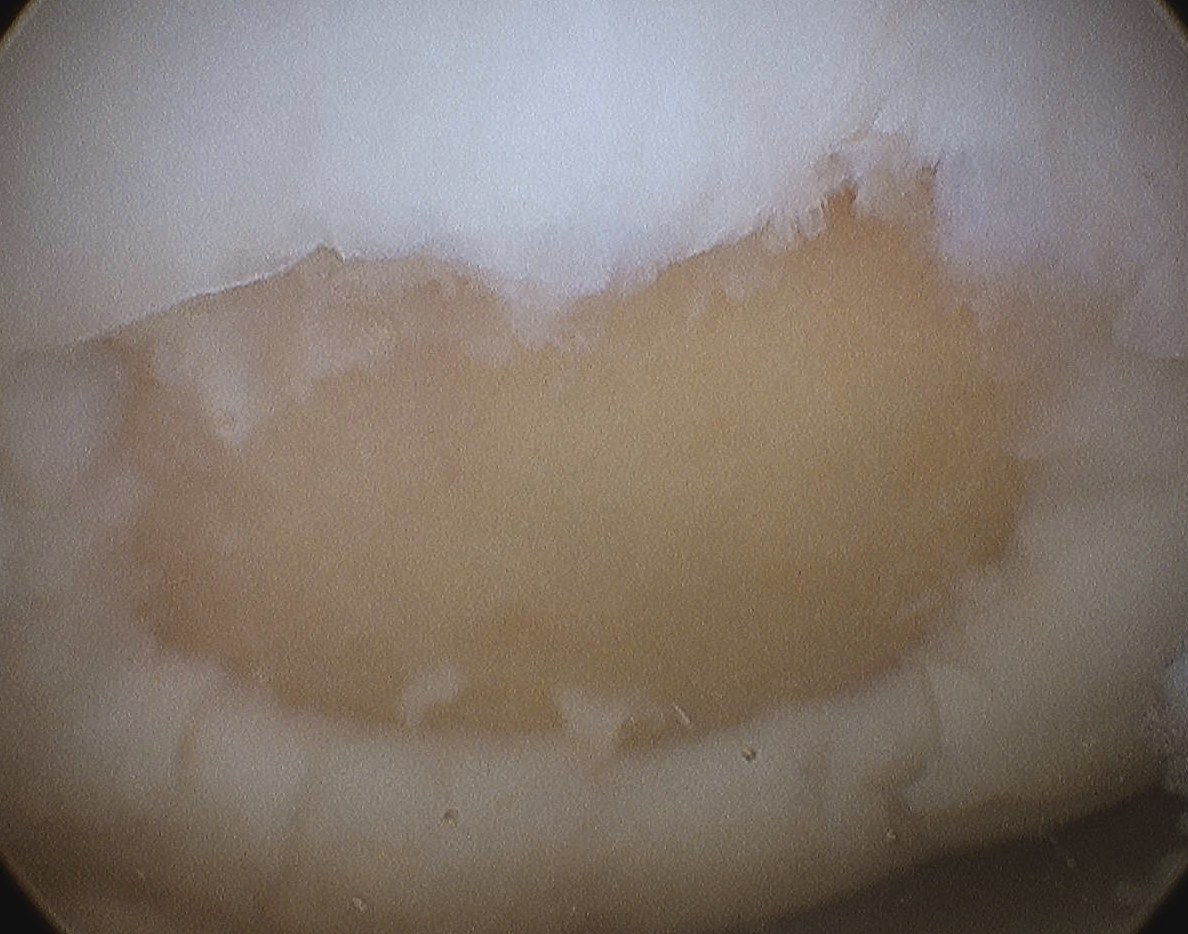
Grade 1: Softening and swelling of the cartilage
Grade 2: Fragmentation and fissuring in an area half an inch or less in diameter
Grade 3: Same as grade 2 but an area more than half an inch in diameter is involved
Grade 4: Erosion of cartilage done to bone
Issue
- difference between grade 2 and 3 is size
- depth is probably more of an issue
ICRS / International Cartilage Research Society
Grade 0: Normal
Grade 1: Nearly normal / soft indentation and/or superficial fissures and cracks

Grade 2: Abnormal (lesions extending down to < 50% of cartilage depth)
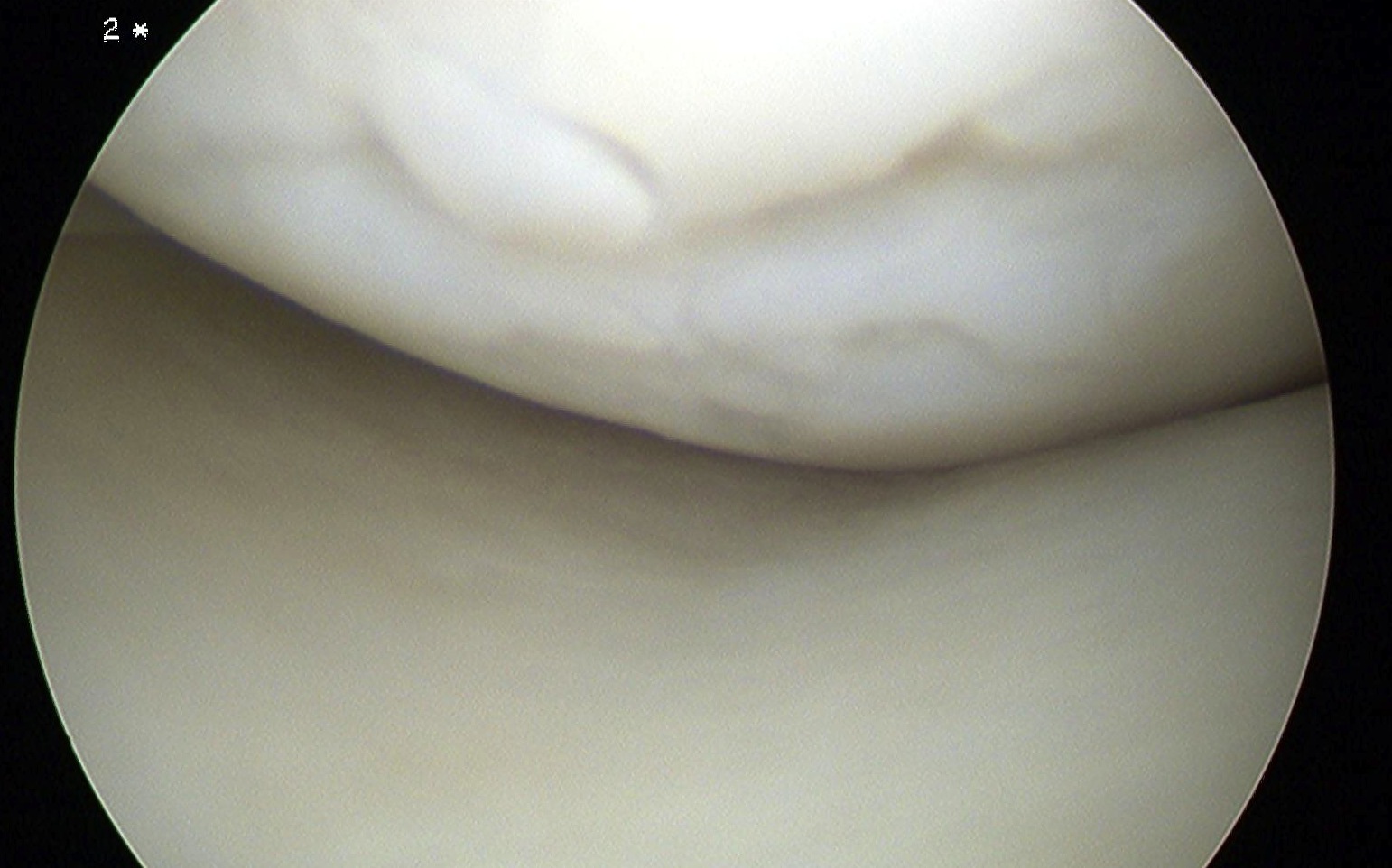
Grade 3: Severely abnormal (cartilage defects > 50% of cartilage depth)
Grade 4: Severely abnormal (through to the subchondral bone)
Sizing
5mm graduated probe
- tend to overestimate size arthroscopically
Measure in 2 dimensions
- give a size in cm2
- assumes that lesions are basically rectangular
Treatment Algorithms
Indications
- grade 3 or 4 ICRS lesions
Niemeyer et al Arthroscopy 2011
- lesions < 4cm2 microfracture
- lesions > 4cm2 or failed microfracture ACI
Cole et al JBJS 2009
- < 2 - 3 cm2 with microfracture or OATS (osteochondral allograft transplantation)
- > 2 - 3 cm2 with osteochondral allograft (OCA) or autologous chondrocyte implantation (ACI)
- trochlea - microfracture or ACI + anteromedialization of the trochlea
Brittberg 2003
- osteochondral lesions < 8mm deep can be managed with ACI
- osteochondral lesions > 8mm deep require bone graft / ACI or OATS
1. Microfracture / drilling

Principle
- pluripotent marrow cells
- produce fibrocartilage to varying degree
- principally type 1 cartilage
- low stiffness and poor wear characteristics over time
- may be more beneficial to combine with realignment procedure
Indications
- young patient
- contained defect
- best results < 2 cm2
- BMI < 30
- age < 40
- need cartilage on each side to contain clot
CI
- axial malalignment
- uncontained lesion (edge of condyles / intercondylar notch
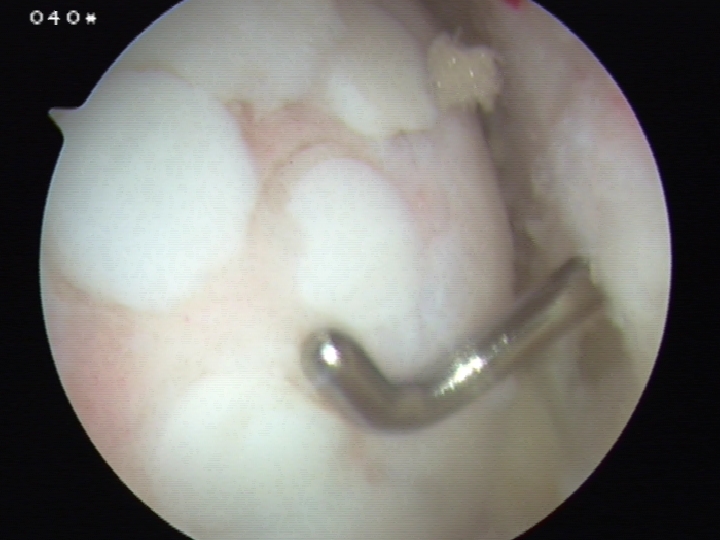
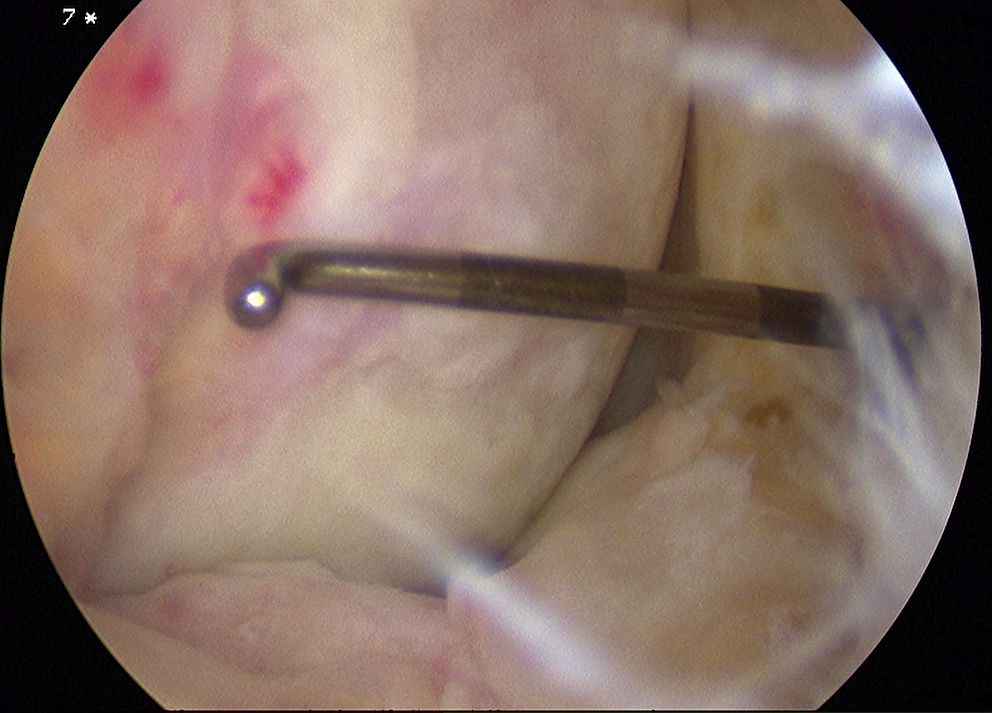
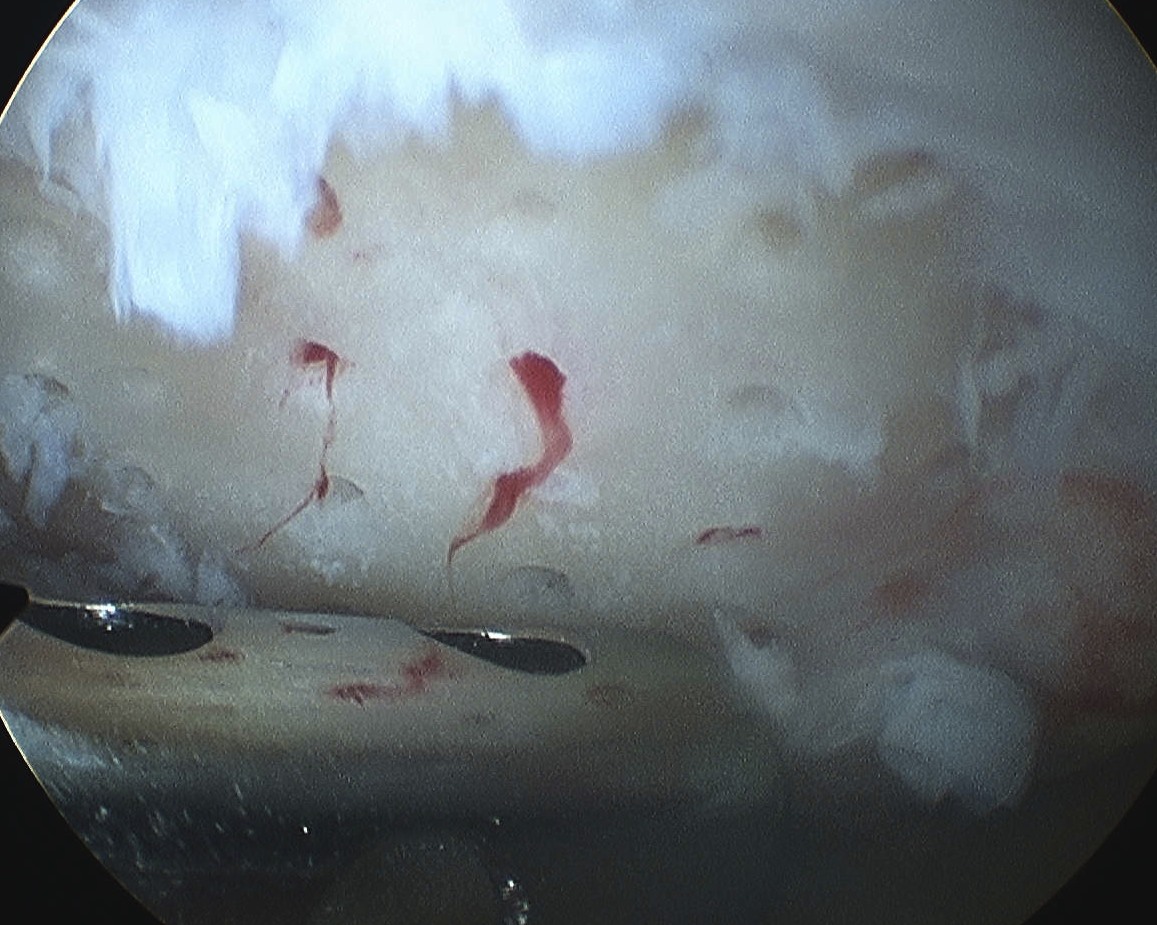
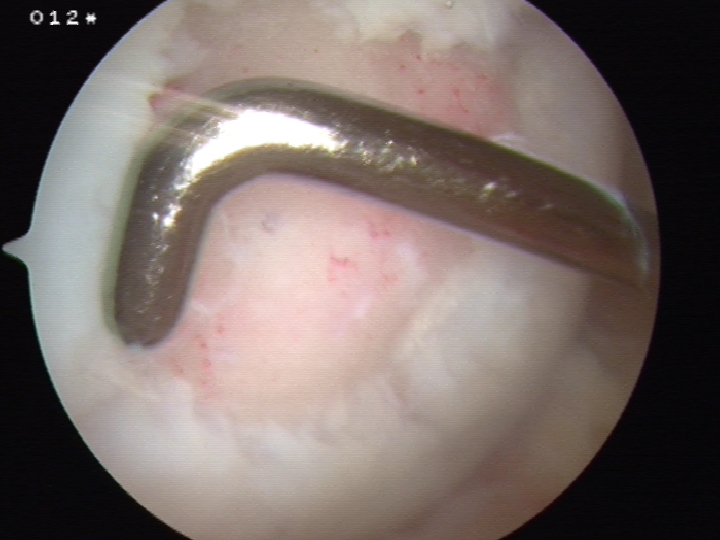
Technique (Steadman J Knee Surg 2002)
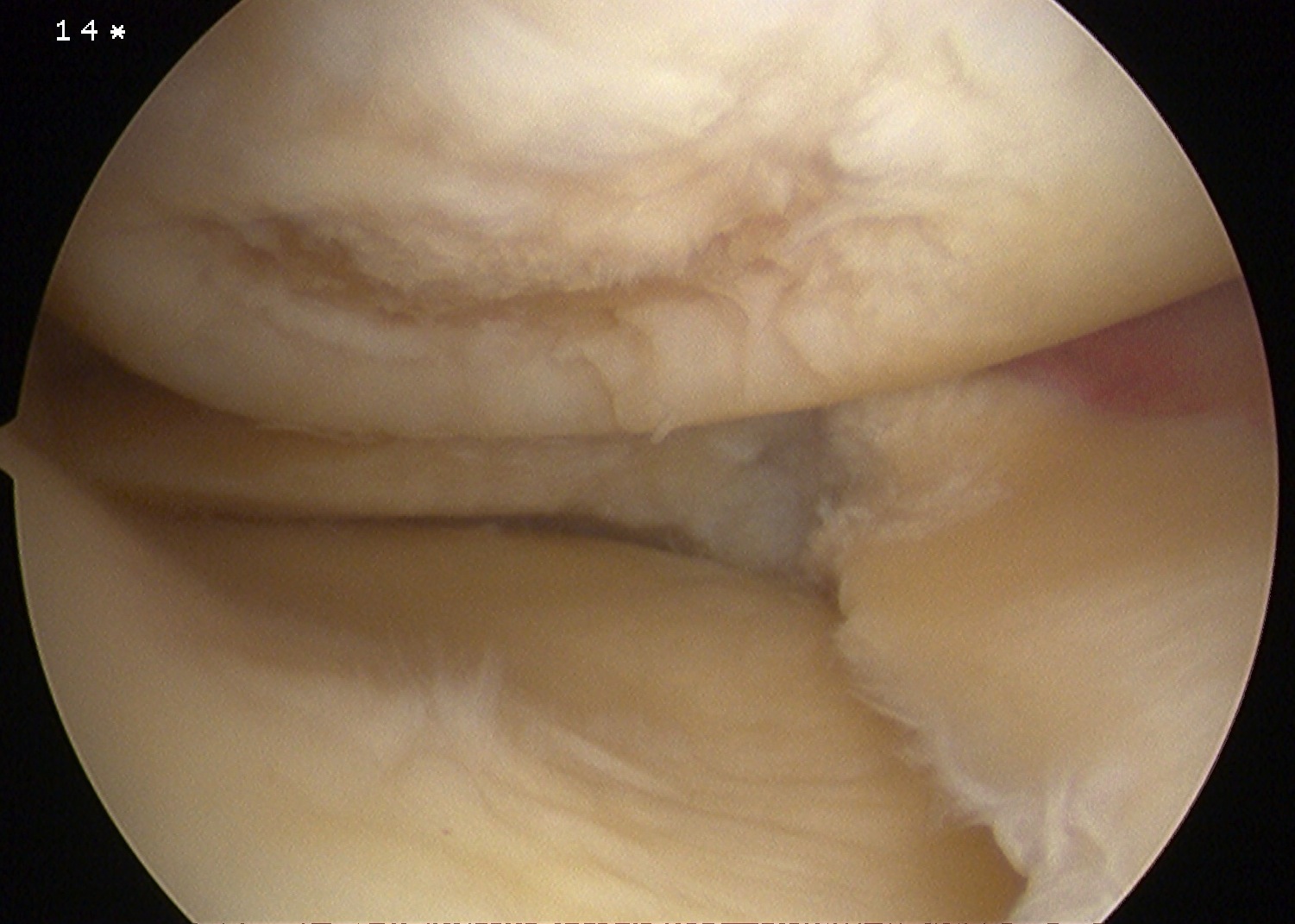
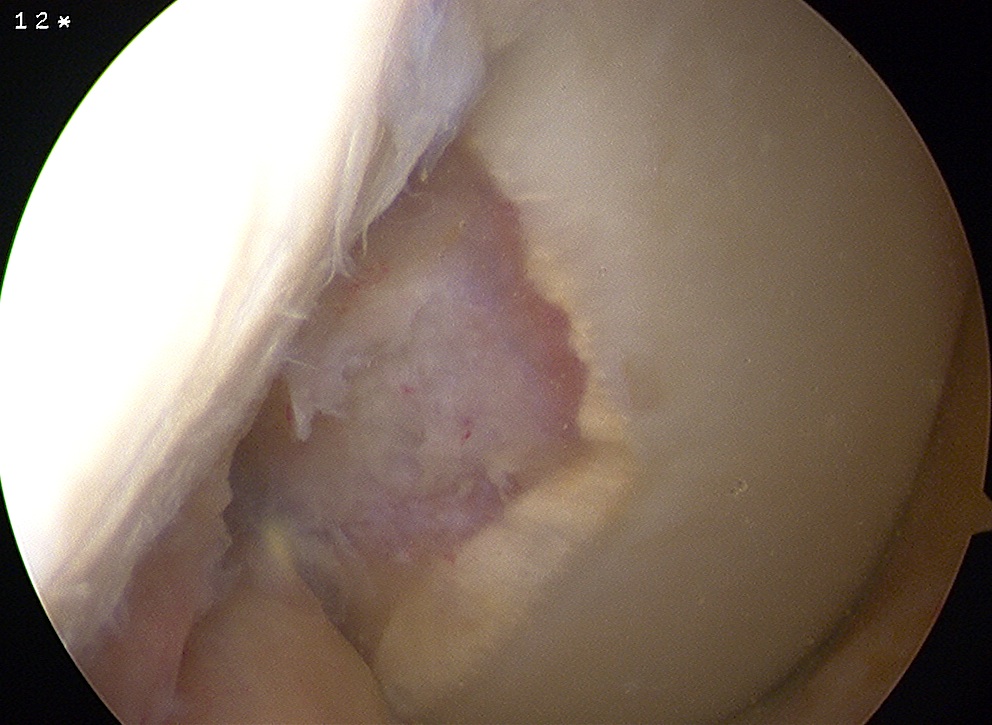
1. Debride all unstable cartilage to stable edge
- removed calcified cartilage layer with curette, protect subchondral bone
- create a perpendicular edge which helps to hold the superclot
- if there is a great deal of subchondral sclerosis may remove with arthroscopic burr
- until reveal punctate bleeding

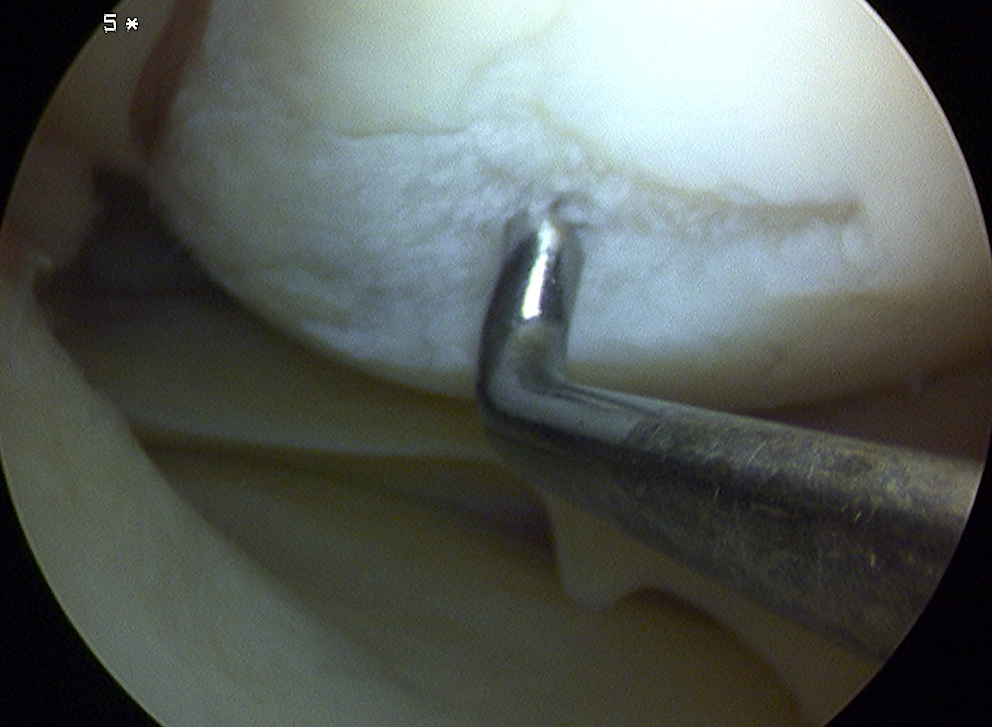
2. Arthroscopic awl
- usually have bend of 30o (Steadman Pick)
- typically 3-4 mm apart
- depth until see fat globules (2-3 mm)
- start at periphery and finish at centre
- will see blood oozing if drop pump pressure / turn off tourniquet / apply suction
Post op
NWB 8/52
Full passive ROM
Brace locked 0 - 20o for PFJ
ROM brace to prevent varus / valgus
No running for 3/12
No sports for 6/12
Complications
Patients may feel catching of perpendicular edge
- will resolve over time
Swelling common for 6-8 weeks
Results
Knutsen et al JBJS Am 2007
- prospective RCT ACI v microfracture
- 77% good results in both groups at 5 years
Steadman et al Am J Sports Med 2004
- combined microfracture and HTO in patients with varus > 5o
- effective at reducing pain and improving function
2. Membranous Autologous Cartilage Implantation

Principle
Transplant living viable cells
- capable of synthesising and maintaining a cartilaginous matrix
- makes a substance physically and histologically similar to hyaline cartilage
MACI v ACI
- cells presented on a membrane for implant
- ACI have to harvest periosteum to secure cells in place
Requirements
Nil instability
Nil malalignment
Problem
Doesn't deal with bony defect
- only cartilage defect
Technique Harvest
Harvest mature chondrocytes
Biopsy taken from NWB area
- in notch or lateral edge of femoral cartilage
- use small punch, take 5 - 6 very small bites
Placed in tubes of saline for transport
- provided by company
- blood taken to isolate serum
- cells isolated and washed
- expanded in cell culture
- attached to membrane
- process takes about six weeks
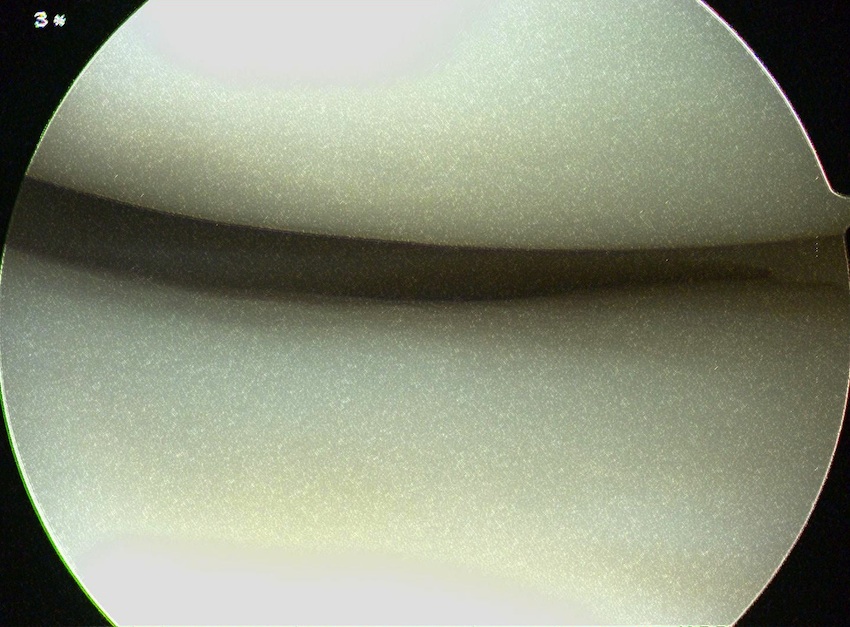
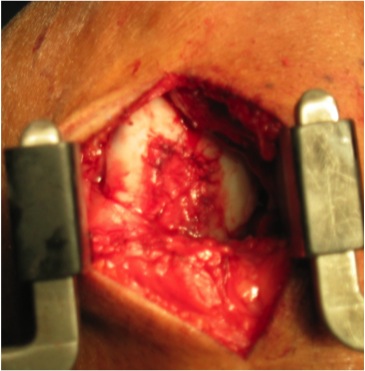
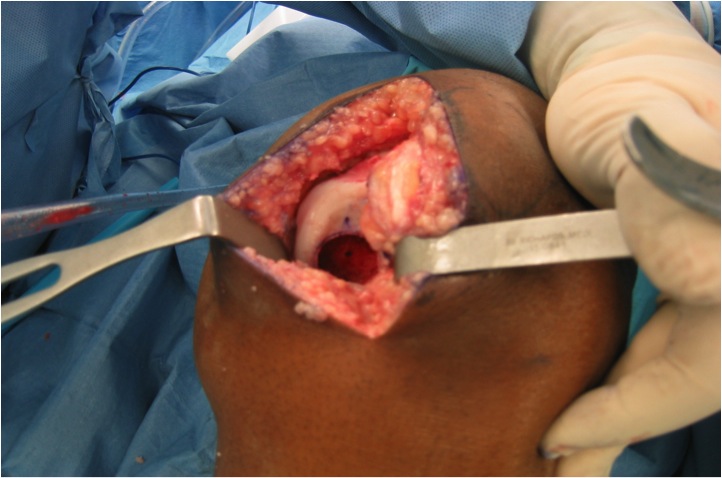
Technique Implantation
Approach
- medial or lateral parapatellar
- if lateral lesion very large, may need medial parapatellar approach to evert patella
- cut through retinaculum in extension so can pull up tissue towards knife and avoid cutting femoral condyle
- distally often have to make small radial incision in meniscus which can be repaired afterwards
- again, take care to protect the tibial plateau cartilage
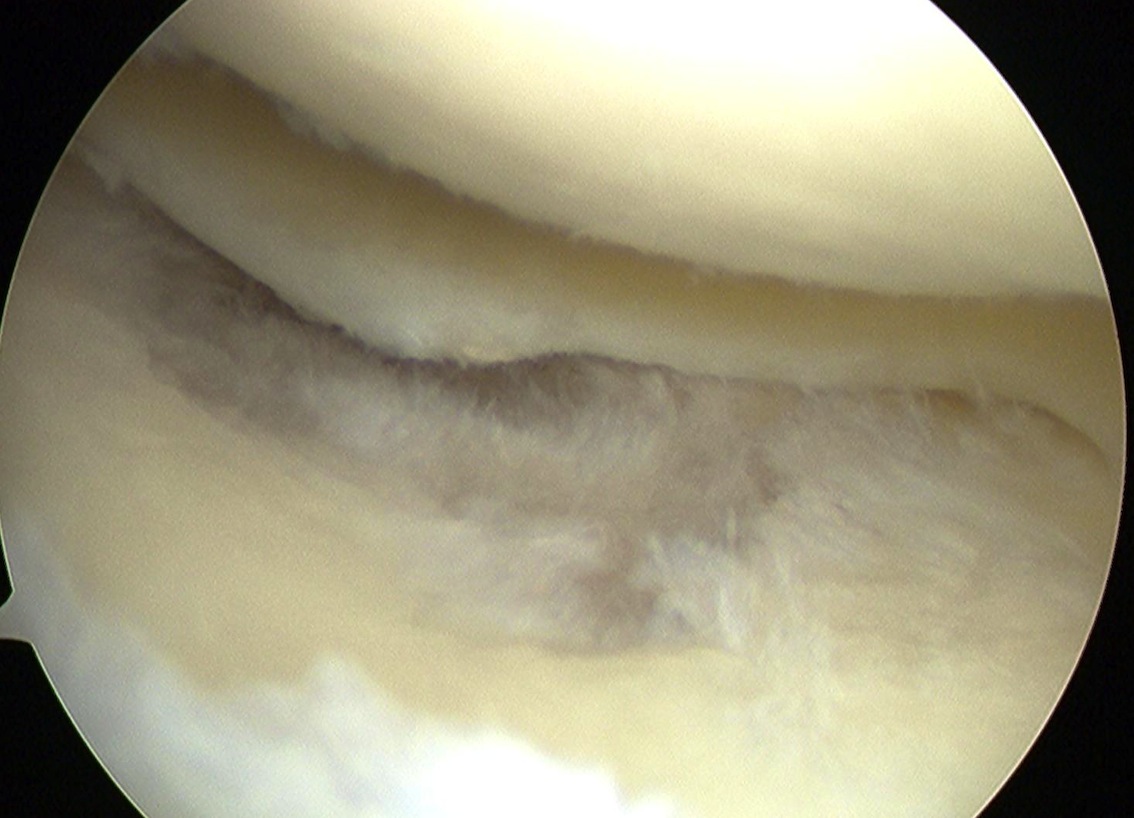
Lesion
- use knife to cut cartilage edge to sharp stable margin
- use curette at base, but must keep subchondral plate intact to prevent bleeding
- excess bleeding will wash away graft
- options to control bleeding involve the use of adrenalin soaked gauze or fibrin glue
Sizing
- use foil from suture pack and cut to size
- want graft to be undersized rather than oversized
- needs to fit into defect and not overlap edges
- in this way it will be stable and not be torn away with ROM
- place onto membrane
- must ensure that the cartilage cell side (which look rough) will be placed down
Insertion
- run fibrin glue from above down
- will set quickly
- take graft off paper and insert
- finger digital pressure whilst glue sets
- reassess MACI and check edges are not overhanging
- trim with scissors if needed
- ensure is stuck down (can reapply glue and re-pressurise)
ROM
- do a rough aggressive ROM to ensure is graft stable
Post op
NWB 8/52
- limit ROM to 90o for 6 weeks
- no sports minimum 6 months
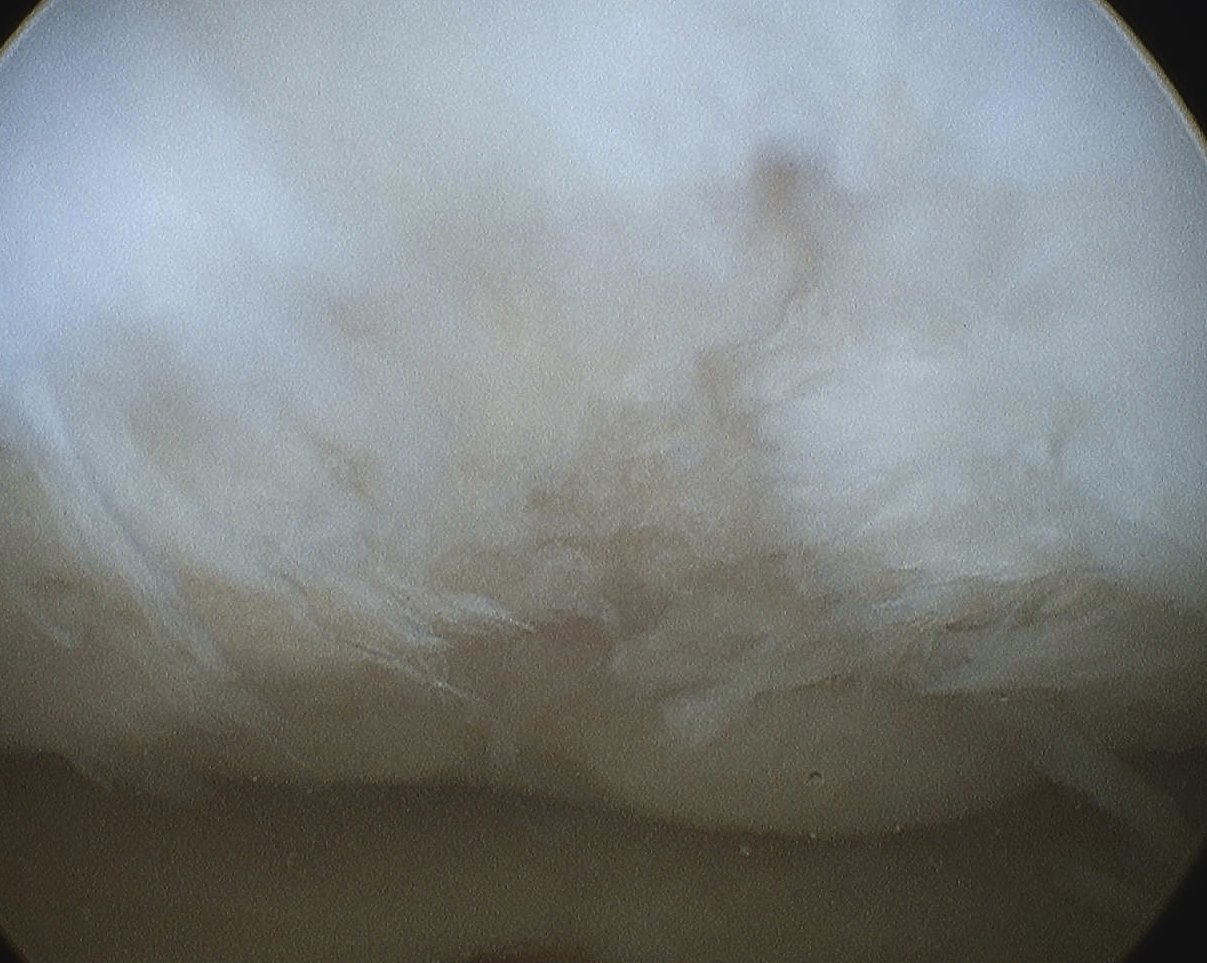
Results
Ebert et al Am J Sports Med 2011
- 5 year clinical and MRI follow up of 41 patients
- 90% good or excellent filling of chondral defect on MRI
- 86% able to do ADL's
- 76% able to return to sport
3. Autologous Chondrocyte Implantation
Implantation
1. Harvest a periosteal graft form proximal medial tibia
- medial or lateral parapatellar approach
- nothing done to subchondral plate to prevent any bleeding
- place periosteum cambium layer down
- suture in place with 6.0 Dexon / Vicryl
- seal edges with fibrin glue except with one corner
- inject cells, seal edge with fibrin glue
2. Porcine collagen ACI-C
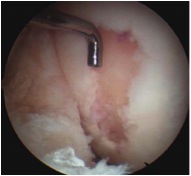
Results
Bartlett et al JBJS Br 2005
- RCT of ACI-C v MACI
- arthroscopic review at one year
- 80% good cartilage in ACI v 66% in MACI
- similar clinical outcomes in each
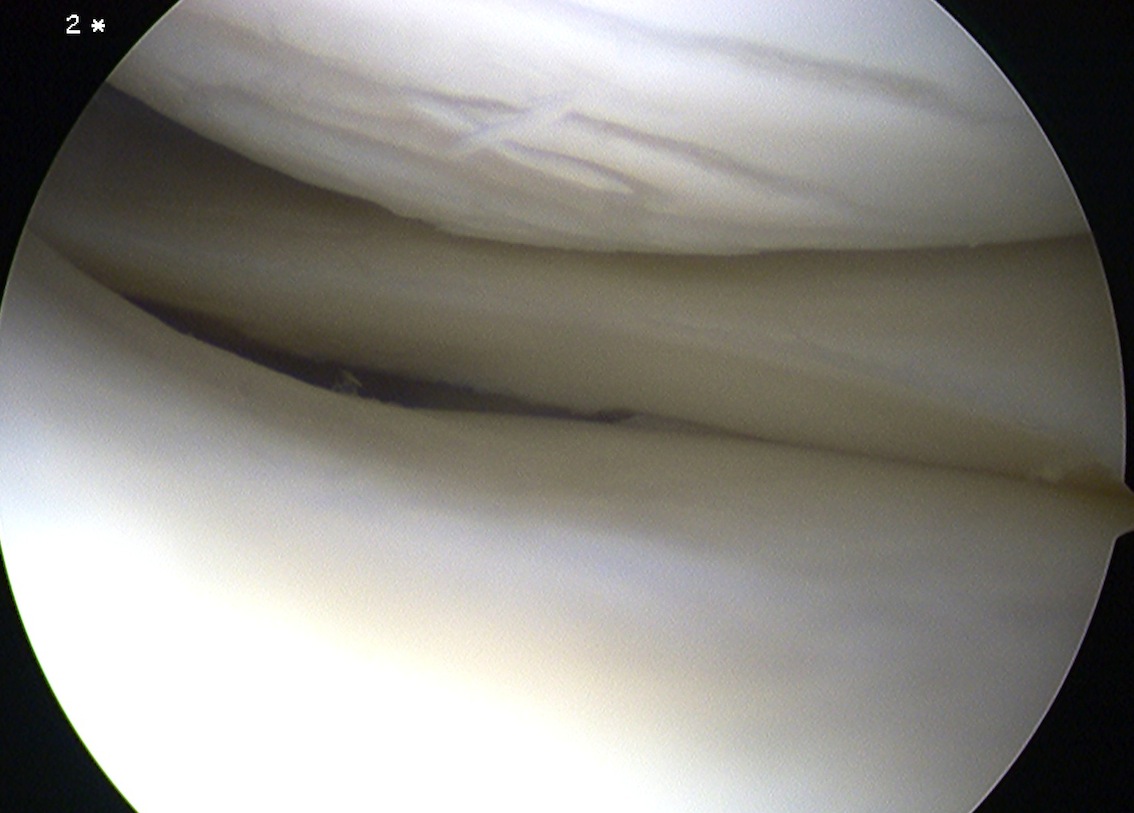
4. Mosaicplasty / Osteochondral Autograft Transplant / Osteochondral Allograft Transplantation (OATS)
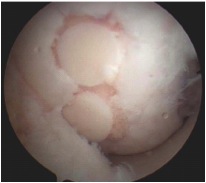


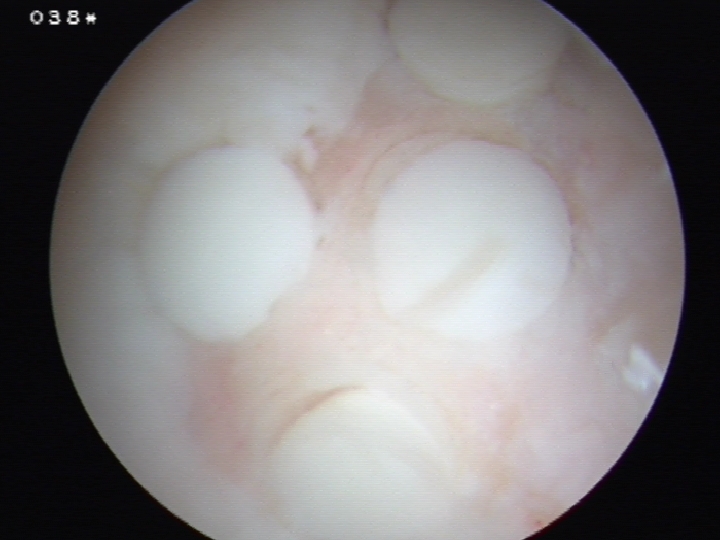
Principle
Take bone plugs on bone and cartilage
- implant in defect
- get coverage with normal hyline cartilage
- also deals with bone defect
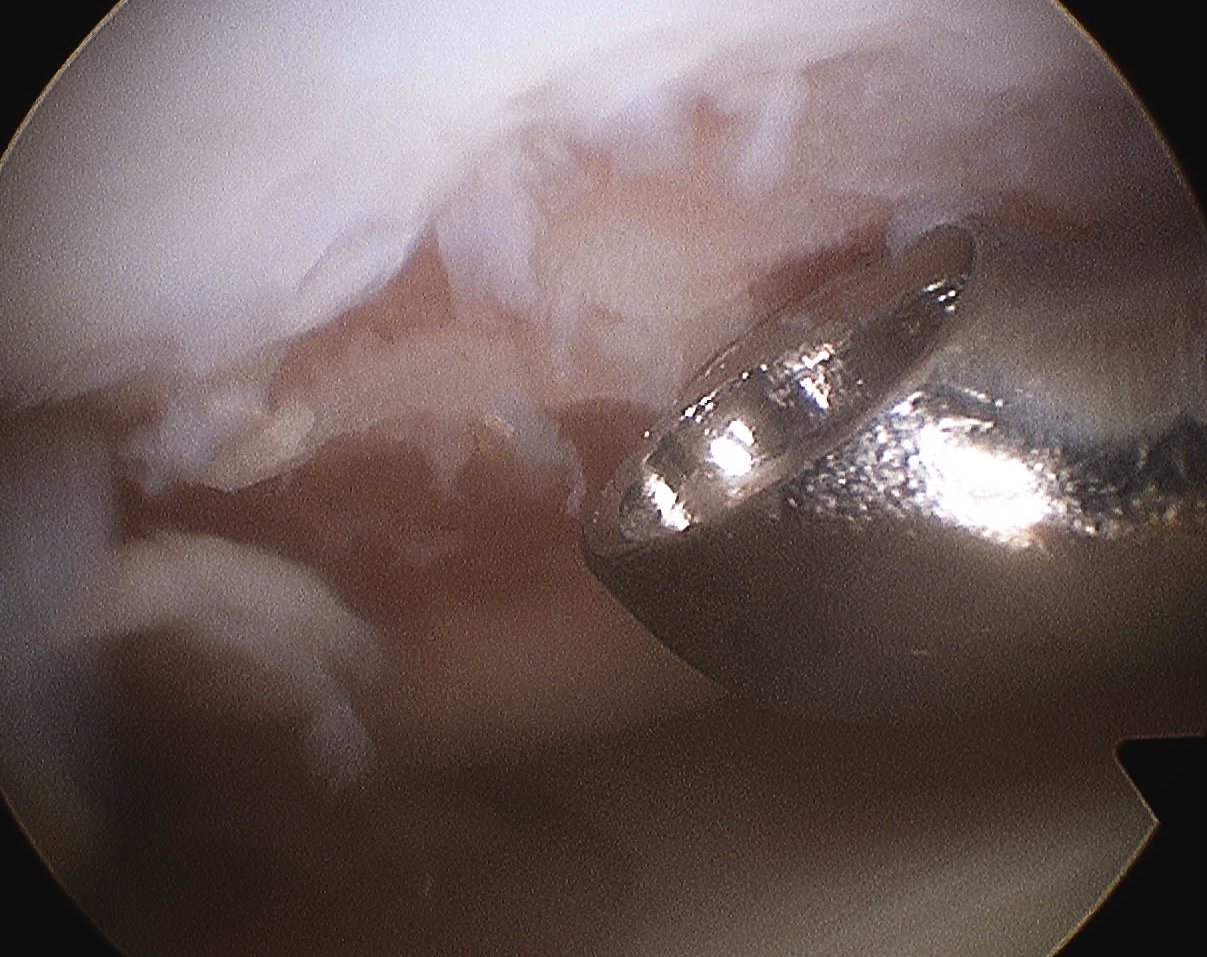
Technique
Prepare Defect
- debride all tissue from defect
- create cylindrical holes with drill
Donor sites
- periphery of femoral trochlea
- trochlea notch
- plug size 4.5 mm usually
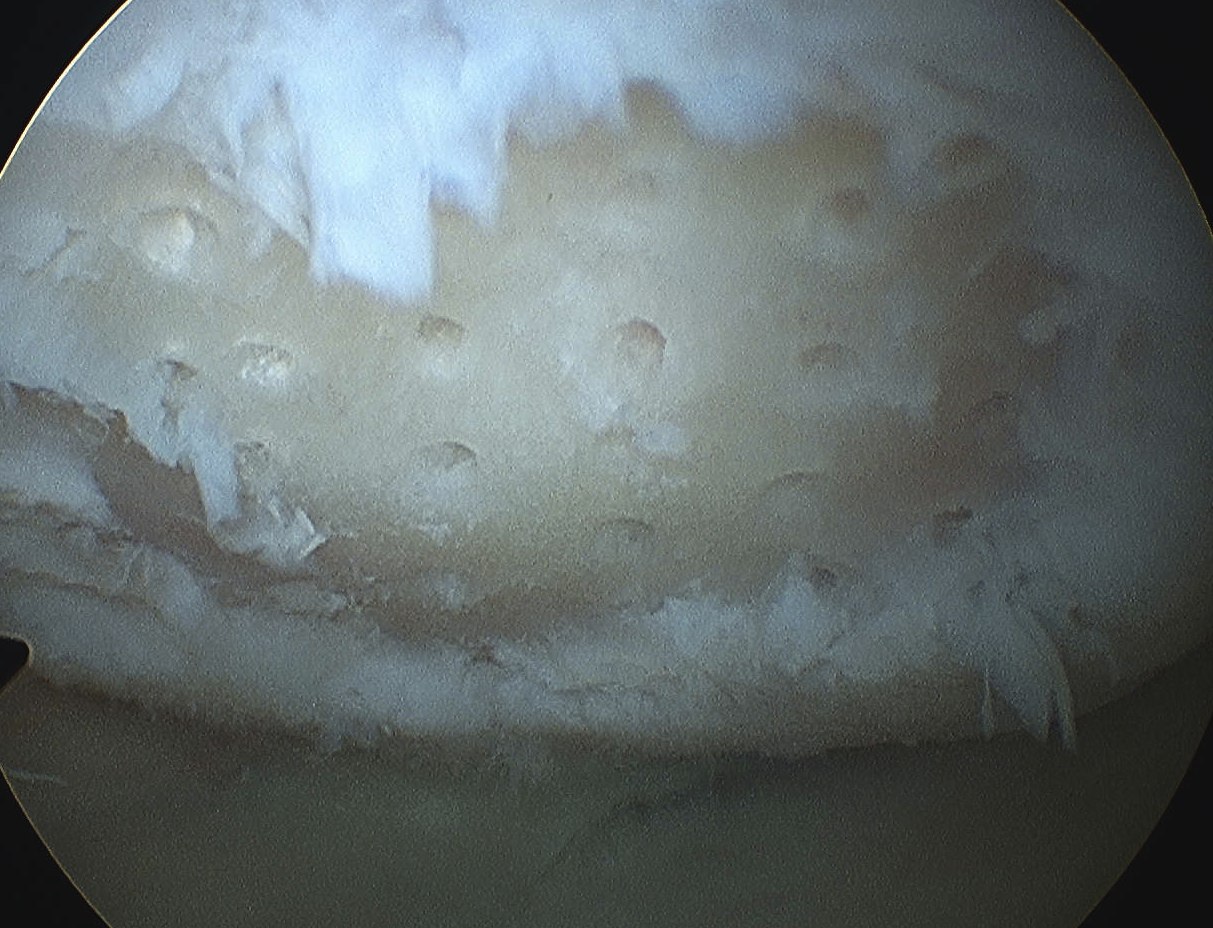
Implant
- fill with plugs of bone and cartilage in mosaic fashion
- fill 60 - 80%
- slightly recess cartilage on plugs
- attempt to match radius of curvature
Post op
MRI at six months
- assess cartilage regrowth

Results
Hangody et al Am J Sports Med 2010
- 354 patients followed up for average 9 years
- 91% good results in femur
- 86% good results in tibia
- 74% good results in PFJ
- 92& good results in talus
Gudas et al Arthroscopy 2005
- RCT of OATS v microfracture of 60 young adults
- all with chondral defects, followed up for 3 years
- 93% OATS and 50% microfracture returned to sport
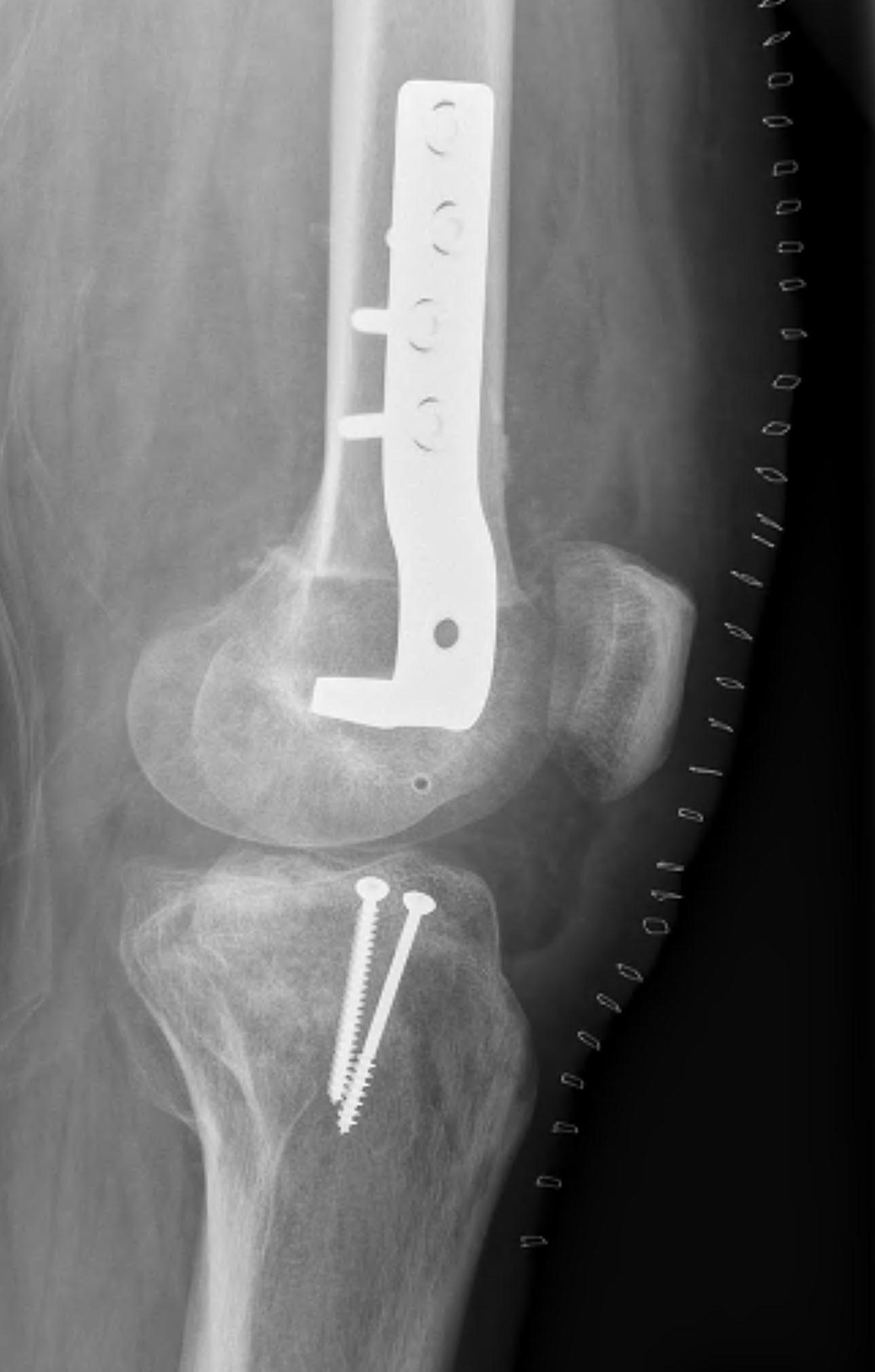
5. Osteochondral allografts


Advantage
Very large, non contained defects
Restore anatomic contour
Nil donor site morbidity
Viable chondrocytes
Fresh grafts
- 70% viable
- None on frozen, irradiated grafts
Technique
CT
- match curvature of radius of donor
Combine with HTO if any malalignment
- usually HTO for medial femoral condyle defects / in varus
- usually distal femoral osteotomy for valgus deformity
Press fit
- if surrounding by good bone
Cases
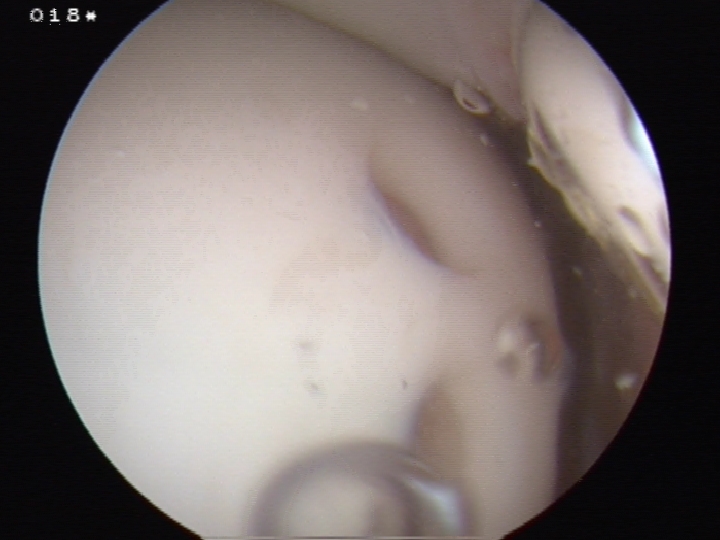
Case 1
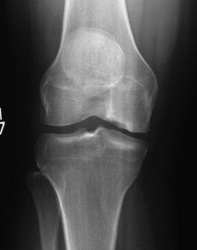

Case 2


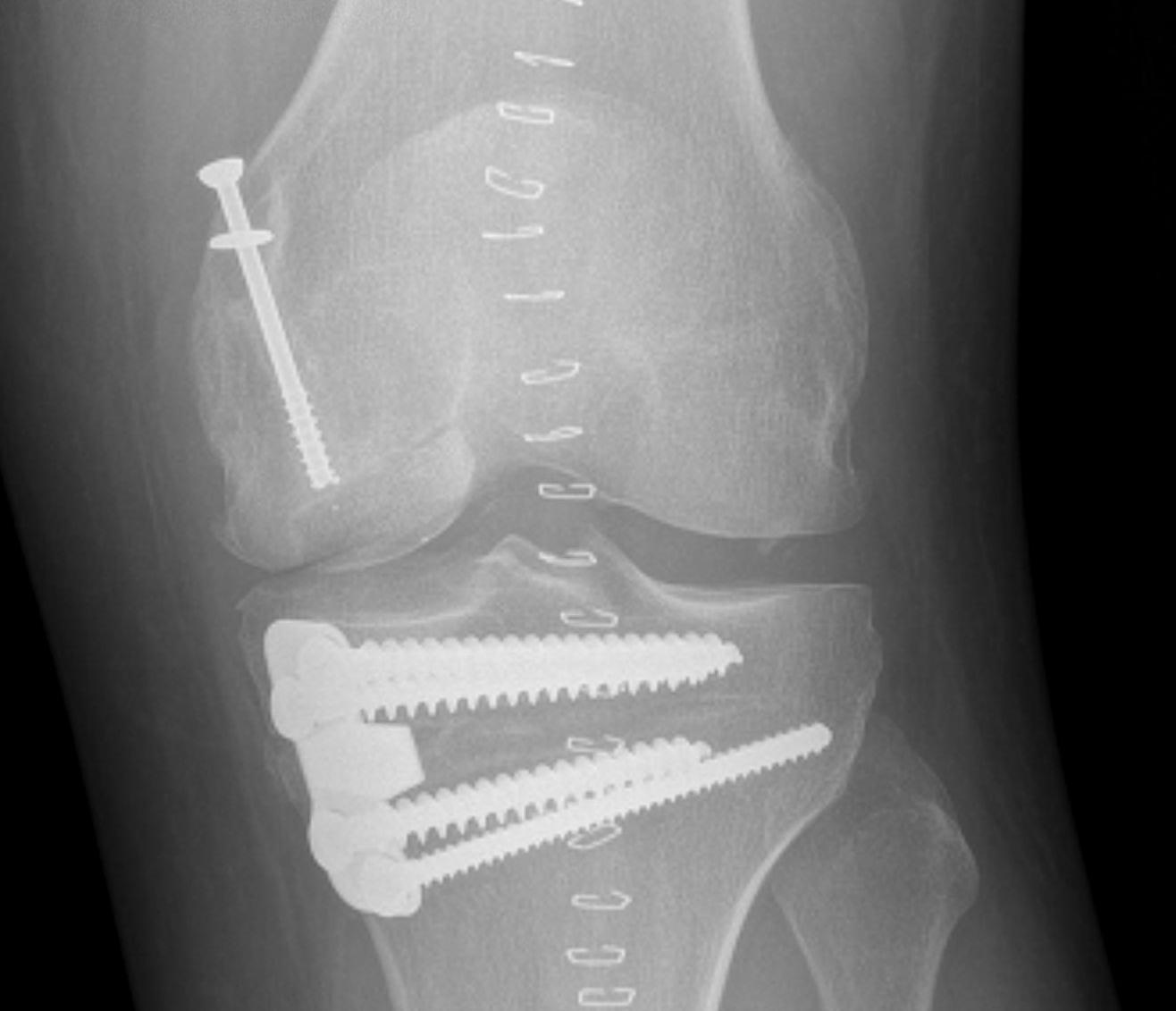

Case 3



Results
Gross et al CORR 2001
- 75 distal femoral osteochondral allografts
- patient average age 27, average follow up 10 years
- 68% had HTO or DRVO
- 20% graft failures (3 graft removals, 9 TKR)
- of the remaining cases, 40/48 patients had good or excellent outcome
6. Hemicap