Types
|
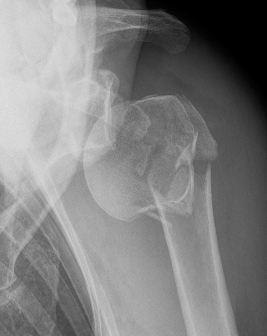
Proximal humerus Surgical neck of humerus |
Proximal third | Midshaft |
Distal 1/3 extra-articular |
Distal 1/3 intra-articular |
|---|---|---|---|---|
 |
 |
 |
 |
 |
Nonoperative Management
Indications
< 20o sagittal
< 30o coronal
< 3 cm of shortening

Options
1. Vietnam Cast / hanging cast
2. Functional bracing / Sarmiento





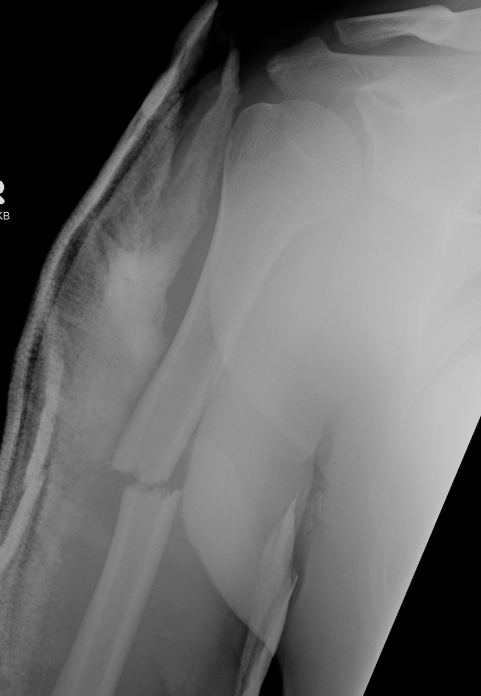
Union of a midshaft humerus fracture treated nonoperatively




Union of distal humerus fracture treated nonoperatively
Results
Union rates
- non operative v operative treatment 213 fractures
- non operative: 20% nonunion and 12% malunion
- operative group: 8% nonunion and 1% malunion
- no difference in time to union in two groups
Ali et al. J Shoulder and Elbow Surgery 2015
- retrospective review of 138 patients treated nonoperatively
- 17% nonunion (24/138)
- proximal fractures highest nonunion rate
Time to union and functional outcome
- literature review of functional bracing humerus shaft fractures
- average time to union 10.7 weeks
- full shoulder ROM in 80%
- full elbow ROM in 85%
Complications of nonoperative care


Intolerance of sarmiento brace


Nonunion in a proximal humerus shaft fracture treated nonoperatively


Nonunion in a proximal humerus shaft fracture treated nonoperatively
Radial Nerve Injury
Incidence
- systematic review of humerus shaft fracture
- 11.8% (532/4517) radial nerve injuries
- most common with middle, and middle/distal fractures
- 70% spontaneously recovered without intervention
- recovery rate 88% in those undergoing delayed exporation (14 weeks)
- recovery rate 88% in those undergoing immediate exploration
Holstein Lewis fracture


Holstein-Lewis JBJS Am 1963
- series of 7 oblique distal third fractures with radial nerve injury
- all were treated operatively
- nerve in fracture gap in 2 / impaled in 1 / severed in 2 / contused +/- in callus in 2
- advised against attempted closed reduction
- risk of contusing nerve between fragments
- advised early open reduction through anterolateral approach
- the radial nerve is closely assoicated with the fracture site and the fracture spike
Korompilias et al. Injury 2013
- 25 patients with complete nerve palsy and humerus shaft fractures
- 13 fully recovered by 12 weeks
- explored 12 patients with no recovery at 16 weeks
- nerve lacerated in two patients
- intact in remainder - these fully recovered by 20 - 24 weeks
Management
Absolute indications for exploration
- open fractures
- radial nerve palsy following closed reduction
Relative
- Holstein-Lewis fracture patterns
- patient undergoing ORIF
- no recovery at 10 - 12 weeks
Expectant management
- wait 10 - 12 weeks
- if no recovery EMG
- consider exploration +/- neurolysis +/- nerve graft at that time
- if that fails, tendon transfer for radial nerve palsy
Operative Management of Humeral Shaft Fractures
Indications


Absolute
Compound fracture
Failure to obtain / maintain acceptable reduction
Radial nerve palsy post reduction
Nonunion
Relative
Multi-trauma
Floating elbow
Segmental fracture
Proximal fracture
Displaced Holstein Lewis with radial nerve palsy
Pathological fracture - won't heal
Bilateral humeral fractures
Obese (very difficult to splint)
Brachial plexus injury - allows early rehab
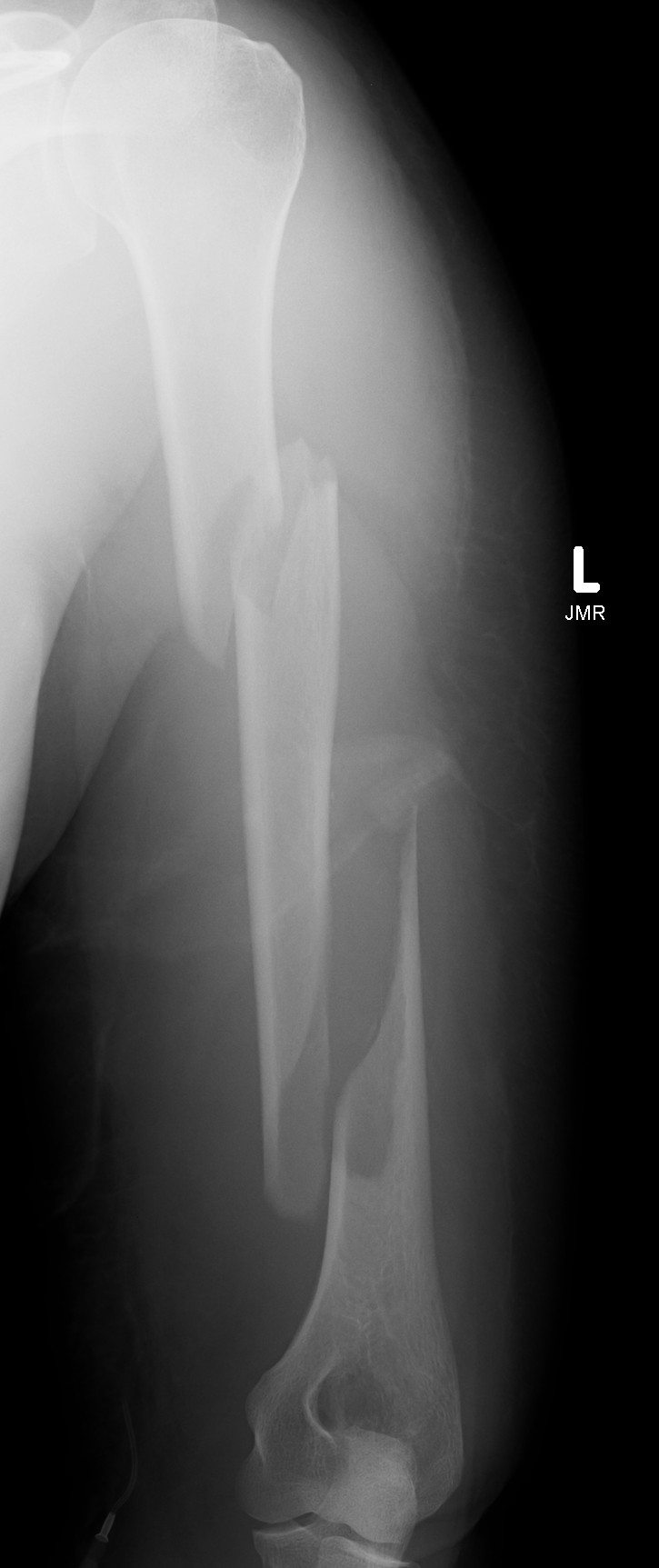


Segmental fracture ORIF
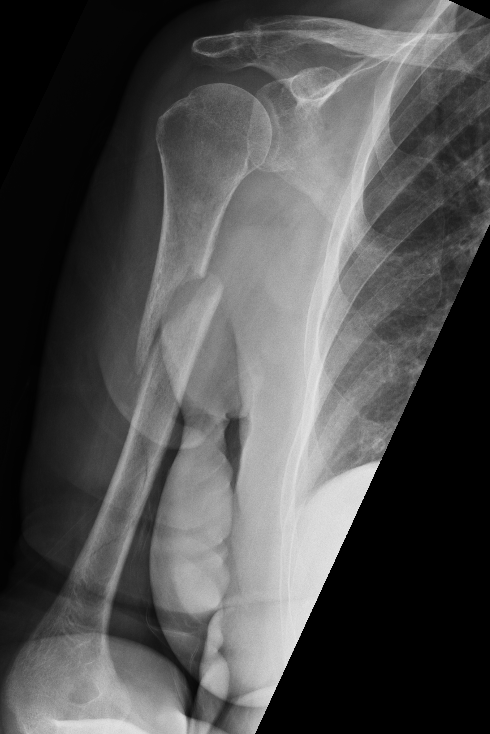



Proximal third humerus ORIF of nonunion
